Octreotide (oral/injection)
Generic name: octreotide (oral/injection) [ ok-TREE-oh-tide ]
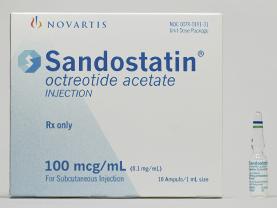
Brand names: Bynfezia, Mycapssa, SandoSTATIN, SandoSTATIN LAR Depot
Dosage forms: injectable solution (100 mcg/mL; 1000 mcg/mL; 200 mcg/mL; 50 mcg/mL; 500 mcg/mL),
... show all 4 dosage forms
Drug class: Somatostatin and somatostatin analogs
What is octreotide?
Octreotide is a man-made protein that is similar to a hormone in the body called somatostatin. Octreotide lowers many substances in the body such as insulin and glucagon (involved in regulating blood sugar), growth hormone, and chemicals that affect digestion.
Octreotide is used to treat acromegaly. Octreotide is also used to reduce flushing episodes and watery diarrhea caused by cancerous tumors (carcinoid syndrome) or tumors called vasoactive intestinal peptide tumors (VIPomas).
Octreotide may also be used for purposes not listed in this medication guide.
Octreotide side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Octreotide may cause serious side effects. Call your doctor at once if you have:
-
severe constipation;
-
slow or uneven heartbeats;
-
signs of gallstones--fever, chills, nausea, vomiting, severe pain in your upper stomach spreading to your back, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
high blood sugar--increased thirst, increased urination, dry mouth, fruity breath odor;
-
low blood sugar--headache, hunger, sweating, irritability, dizziness, fast heart rate, and feeling anxious or shaky; or
-
underactive thyroid--extreme tired feeling, dry skin, joint pain or stiffness, muscle pain or weakness, hoarse voice, feeling more sensitive to cold temperatures, weight gain.
Common side effects of octreotide may include:
-
gallstones;
-
nausea, vomiting, diarrhea, stomach pain, gas;
-
headache, back pain; or
-
dizziness, tiredness.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Warnings
Follow all directions on your medicine label and package. Tell each of your healthcare providers about all your medical conditions, allergies, and all medicines you use.
Before taking this medicine
You should not use octreotide if you are allergic to it.
Tell your doctor if you have ever had:
-
diabetes;
-
heart disease, high blood pressure, or heart rhythm disorder;
-
thyroid problems;
-
liver disease; or
-
kidney disease (or if you are on dialysis).
Tell your doctor if you are pregnant or breastfeeding.
Using octreotide can affect certain hormones that may make it easier for you to get pregnant, even if you were unable to get pregnant before. Talk to your doctor about using birth control to avoid unwanted pregnancy.
Octreotide is not approved for use by anyone younger than 18 years old.
How should I use octreotide?
Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose. Use the medicine exactly as directed.
Octreotide oral is taken by mouth.
Octreotide injection is injected under the skin, into a muscle, or as an infusion into a vein. A healthcare provider will give your first dose and may teach you how to properly use the medication by yourself.
Read and carefully follow any Instructions for Use provided with your medicine. Ask your doctor or pharmacist if you don't understand all instructions.
Swallow the capsule whole and do not crush, chew, break, or open it.
Take the capsule with a full glass of water on an empty stomach, at least 1 hour before or 2 hours after a meal.
You may need to mix octreotide injection with a liquid (diluent) before using it. When using injections by yourself, be sure you understand how to properly mix and store the medicine.
Be sure to follow the instructions for the exact type of octreotide your doctor has prescribed for you.
Prepare an injection only when you are ready to give it. Do not use if the medicine has changed colors or has particles in it. Call your pharmacist for new medicine.
Your healthcare provider will show you where on your body to inject octreotide. Use a different place each time you give an injection. Do not inject into the same place two times in a row.
You will need frequent medical tests.
If you need radiation treatment, you may need to stop using octreotide for a short time. Follow your doctor's instructions very carefully.
Store unopened octreotide in the original carton in the refrigerator. Protect from light. Do not freeze.
Once you have started taking octreotide capsules store them at room temperature away from moisture and heat. Keep each capsule in the blister pack until you are ready to take the medicine.
Take the ampul out of the refrigerator and let it reach room temperature before injecting your dose. Do not heat the ampul. Each ampul is for one use only. Throw it away after one use, even if there is still medicine left inside.
You may also store an unopened ampul at room temperature for up to 14 days. Throw away the ampul if not used within 14 days.
Once you begin using your injection pen, you may store it at room temperature for up to 28 days. Do not freeze, and throw the pen away if it has been frozen.
Throw the injection pen away 28 days after your first use, even if there is still medicine left inside.
Use a needle and syringe only once and then place them in a puncture-proof "sharps" container. Follow state or local laws about how to dispose of this container. Keep it out of the reach of children and pets.
What happens if I miss a dose?
Call your doctor for instructions if you miss a dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Overdose symptoms may include severe upper stomach pain, diarrhea, weight loss, warmth or tingling, numbness or cold feeling, unexplained muscle pain, weakness, weak pulse, fainting, or slow breathing (breathing may stop).
What should I avoid while using octreotide?
Follow your doctor's instructions about any restrictions on food, beverages, or activity.
What other drugs will affect octreotide?
Tell your doctor about all your other medicines, especially:
-
bromocriptine (Cycloset, Parlodel);
-
insulin or oral diabetes medicine; or
-
heart or blood pressure medication.
This list is not complete. Other drugs may affect octreotide, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
More about octreotide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (17)
- Latest FDA alerts (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: somatostatin and somatostatin analogs
- Breastfeeding
- En español
Patient resources
- Octreotide (Injection, Intramuscular, Subcutaneous) advanced reading
- Octreotide (Oral) (Advanced Reading)
- Octreotide Injection (Vials)
- Octreotide Long-Acting Injection
Other brands
Sandostatin, Sandostatin LAR Depot, Mycapssa, Bynfezia Pen
Professional resources
Other brands
Sandostatin, Mycapssa, Bynfezia Pen
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 6.02.