Valproic Acid (Monograph)
Brand name: Depakote
Drug class: GABA-mediated Anticonvulsants
- Histone Deacetylase Inhibitors
Warning
- Hepatotoxicity
-
Potentially fatal hepatic failure can occur.
-
Usually occurs during the initial 6 months of therapy.
-
Children <2 years of age are at considerably increased risk of developing fatal hepatotoxicity, especially those receiving multiple anticonvulsants and those with congenital metabolic disorders, severe seizure disorders accompanied by mental retardation, or organic brain disease. Use with extreme caution in this age group and only as single-agent therapy; carefully weigh benefits versus risks. Incidence of fatal hepatotoxicity appears to decrease progressively with increasing age.
-
Serious or fatal hepatotoxicity may be preceded by nonspecific symptoms such as malaise, weakness, lethargy, facial edema, anorexia, and vomiting.
-
In epileptic patients, loss of seizure control also may precede development of hepatotoxicity.
-
Monitor patients closely for development of any such changes.
-
Perform liver function tests prior to and at frequent intervals during therapy, especially during the first 6 months. (See Hepatotoxicity under Cautions.)
-
Increased risk of acute liver failure (sometimes resulting in death) in patients with hereditary mitochondrial disorders caused by mutations in the polymerase gamma (POLG) gene (e.g., Alpers-Huttenlocher syndrome); contraindicated in patients known to have such disorders and in children <2 years of age in whom there is a clinical suspicion of a mitochondrial disorder. In children >2 years of age with suspected hereditary mitochondrial disease, use only if other anticonvulsant therapies have failed; closely monitor such patients with regular clinical assessments and liver function tests. Perform POLG mutation screening according to current clinical practice.
- Fetal Risk
-
Risk of major congenital malformations, particularly neural tube defects (NTDs).
-
Risk of decreased IQ scores following in utero exposure.
-
Contraindicated in pregnant women for migraine prophylaxis. In pregnant women with epilepsy or bipolar disorder, use only if other therapies fail or are otherwise unacceptable.
-
Do not use in women of childbearing potential unless the drug is essential to their medical condition. This is particularly important when contemplating treatment of a spontaneously reversible condition not ordinarily associated with permanent injury or risk of death (e.g., migraine headaches). (See Pregnancy under Cautions.)
-
A medication guide describing the risks of valproic acid is available for patients. (See Advice to Patients.)
- Pancreatitis
-
Life-threatening pancreatitis has occurred both in children and adults.
-
Some cases described as hemorrhagic with rapid progression from initial symptoms to death.
-
Can occur shortly after initial use as well as after several years of use.
-
Warn patients and caregivers that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis that require prompt medical evaluation.
-
Usually discontinue the drug and initiate alternative therapy if pancreatitis is diagnosed.
Introduction
Valproic acid (the active moiety), valproate sodium, and divalproex sodium are carboxylic acid-derivative anticonvulsants; also antimanic, other psychotherapeutic, and antimigraine agents.
Uses for Valproic Acid
Valproic acid (ionized form: valproate) is the active moiety for valproate sodium and divalproex sodium.
Absence (Petit Mal) Seizures
Alone or with other anticonvulsants (e.g., ethosuximide) as first-line therapy in the prophylactic management of simple and complex absence (petit mal) seizures.
In conjunction with other anticonvulsants in the management of multiple seizure types that include absence seizures.
Complex Partial Seizures
Alone or with other anticonvulsants (e.g., carbamazepine, phenytoin) as first-line therapy in the prophylactic management of complex partial seizures that occur either by themselves or in association with other seizure types.
Generalized Seizures
First-line therapy for generalized seizures, including primary generalized tonic-clonic† [off-label], primary generalized tonic-clonic absence† [off-label], myoclonic† [off-label], or atonic seizures† [off-label], especially when more than one type of generalized seizure is present.
Simple Partial Seizures
First-line therapy for the management of simple partial seizures† [off-label].
Status Epilepticus
Has been administered rectally† or by intragastric drip† with some success in the management of status epilepticus† refractory to IV diazepam.
A parenteral formulation of valproic acid has been studied and has been effective when administered IV† in the management of status epilepticus.
Seizures Associated with Dravet Syndrome
Has been used in the treatment of seizures associated with Dravet syndrome†. Although evidence from controlled studies limited, considered a first-line therapy for this condition.
Bipolar Disorder
Alone or as a component of combination therapy (e.g., with lithium, antipsychotic agents [e.g., olanzapine], antidepressants, carbamazepine) for the treatment of acute manic or mixed episodes associated with bipolar disorder, with or without psychotic features.
American Psychiatric Association (APA) currently recommends combined therapy with valproic acid plus an antipsychotic agent or with lithium plus an antipsychotic agent as first-line drug therapy for the acute treatment of more severe manic or mixed episodes and monotherapy with one of these drugs for less severe episodes.
Valproic acid or lithium also is recommended for the initial acute treatment of rapid cycling.
Some clinicians recommend that valproic acid therapy be used in patients with bipolar disorder or schizoaffective disorder, bipolar type, who have responded inadequately to or have been unable to tolerate treatment with lithium salts or other therapy (e.g., carbamazepine), particularly if the patient displays residual manic symptoms, or in the presence of rapid-cycling, dysphoric mania or hypomania, associated neurologic abnormalities, or organic brain disorder.
Migraine
Prophylaxis of migraine headache.
Because valproic acid poses a hazard to the fetus (see Fetal Risk in Boxed Warning and also see Pregnancy under Cautions), do not use in pregnant women for migraine prophylaxis; in such patients, the risks of the drug outweigh any possible benefits. Use in women of childbearing potential only if the drug is essential.
The US Headache Consortium states that valproic acid has medium to high efficacy for the prophylaxis of migraine headache.
Has also been used IV† for the acute management† (i.e., abortive therapy) of migraine headache; however, role of drug relative to other acute therapies requires further elucidation.
Schizophrenia
As an adjunct to antipsychotic drugs in the symptomatic management of schizophrenia† in patients who fail to respond sufficiently to an adequate trial of an antipsychotic agent alone.
APA and some clinicians state that anticonvulsant agents such as valproic acid and divalproex sodium may be useful adjuncts in schizophrenic patients with prominent mood lability or in those with agitated, aggressive, hostile, or violent behavior.
APA states that, with the exception of patients with schizophrenia whose illness has strong affective components, monotherapy with valproic acid or divalproex sodium has not been shown to be substantially effective in the long-term treatment of schizophrenia.
Valproic Acid Dosage and Administration
General
Do not abruptly discontinue anticonvulsants, including valproic acid, in patients with seizure disorders; withdraw gradually to minimize the potential for increased seizure frequency.
Closely monitor patients for marked changes in behavior that could indicate emergence or worsening of suicidal thoughts or behavior or depression. (See Suicidality Risk under Cautions.)
Distribute medication guide explaining risks and benefits of therapy to patients receiving oral formulations of the drug.
Administration
Administer valproate sodium orally or by IV infusion; administer valproic acid and divalproex sodium orally.
Valproic acid also has been administered rectally† by enema or in wax-based suppositories, but a rectal dosage form is not commercially available in the US.
Oral Administration
Valproic acid, valproate sodium, and divalproex sodium are administered orally.
If GI irritation occurs, may administer with food or gradually increase dosage from an initial low dosage.
Patients unable to tolerate the GI effects of valproic acid or valproate sodium may tolerate divalproex sodium.
If a dose is missed, take as soon as possible unless it is almost time for the next dose. Do not double a dose to make up for a missed dose.
Divalproex sodium extended-release tablets are not bioequivalent to the delayed-release tablets.
Although the extent of GI absorption of valproic acid from capsules containing coated particles or delayed-release tablets of divalproex sodium is equivalent, peak and trough plasma concentrations achieved may vary (e.g., peak valproic acid concentrations generally are higher with the delayed-release tablets); increased monitoring of plasma valproic acid concentrations is recommended if one dosage form is substituted for the other.
Formulation-specific Administration Instructions
Administer divalproex sodium extended-release tablets (e.g., Depakote ER) once daily; for other oral formulations, administer in divided doses if total daily dosage >250 mg.
Valproic acid capsules: Swallow capsules whole, not chewed, in order to prevent mouth and throat irritation.
Valproate sodium oral solution: Do not administer in carbonated beverages.
Divalproex sodium delayed-release (e.g., Depakote) or extended-release (e.g., Depakote ER) tablets: Swallow tablets intact; do not chew or crush.
Capsules containing coated particles of divalproex sodium (e.g., Depakote Sprinkle Capsules): Swallow capsules intact or sprinkle entire contents of capsule(s) on a small amount (about 5 mL) of soft food (e.g., applesauce, pudding) and swallow (not chew) immediately. Do not store the mixture for future use.
IV Administration
Valproate sodium injection is intended for IV use only.
Dilution
For IV use, dilute the appropriate dose of valproate sodium injection with at least 50 mL of a compatible IV solution (e.g., 5% dextrose injection, 0.9% sodium chloride injection, lactated Ringer’s injection).
Rate of Administration
Infuse diluted IV solutions over 60 minutes; the manufacturer recommends that the rate not exceed 20 mg/minute.
Rapid IV infusion has been associated with an increased risk of adverse effects.
Experience from clinical studies of rates >20 mg/minute or infusion periods <60 minutes is limited.
In a study of the safety of initial 5- to 10-minute IV infusions of valproate sodium (1.5–3 mg/kg per minute of valproic acid), patients generally tolerated such rapid infusions; however, the study was not designed to assess the efficacy of the regimen.
Use of rapid infusions as a parenteral replacement for oral valproic acid has not been established.
Dosage
Dosage of valproate sodium and divalproex sodium is expressed in terms of valproic acid.
Must adjust dosage carefully and slowly according to individual requirements and response.
An anticonvulsant therapeutic range of 50–100 mcg/mL has been suggested; seizure control occasionally may occur with lower or higher concentrations, but >150 mcg/mL usually is toxic.
For acute manic or mixed episodes in bipolar disorder, usually dosed to clinical response with trough plasma concentrations of 50–125 mcg/mL.
Frequency of adverse effects (particularly elevated liver enzyme concentrations and thrombocytopenia) may be dose related; carefully weigh the benefit of improved therapeutic effect that may accompany higher dosages against the risk of adverse effects. (See Thrombocytopenia under Cautions.)
When switching to divalproex sodium delayed-release tablets in patients receiving conventional valproic acid, use same daily dosage and schedule. After stabilization with the delayed-release formulation, may divide daily dosage and administer 2 or 3 times daily in selected patients.
Pediatric Patients
Seizure Disorders
Complex Partial Seizures (Monotherapy and Adjunctive Therapy)
Oral (conventional, delayed-, and extended-release preparations)Dosages apply to conventional (capsules and solution), delayed-release (tablets), and extended-release (tablets) dosage forms of valproic acid (active moiety), valproate sodium, and divalproex sodium.
Children ≥10 years of age: Initially, 10–15 mg/kg daily.
Increase dosage by 5–10 mg/kg daily at weekly intervals, according to response and tolerability, up to maximum recommended dosage of 60 mg/kg daily.
When used adjunctively, may continue concurrent anticonvulsant therapy, adjusting dosages according to response and tolerability. (See Interactions.)
Alternatively, may attempt to decrease dosage of the current anticonvulsant by 25% every 2 weeks, either starting concomitantly with initiation of valproic acid therapy or delayed by 1–2 weeks if there is a concern that seizures are likely to occur with a reduction.
Speed and duration of withdrawal of the current anticonvulsant can be highly variable; monitor patients closely during this period for increased seizure frequency.
When converting a patient from a current anticonvulsant to valproic acid therapy for the treatment of complex partial seizures, initiate valproic acid therapy at usual starting dosages.
IVMay employ IV therapy in patients in whom oral therapy temporarily is not feasible, but switch to oral administration as soon as clinically possible.
IV administration can be used for monotherapy or as adjunctive therapy in the management of seizure disorders.
The usual total daily dosages are equivalent for IV or oral administration, and the doses and frequency of administration employed with oral therapy in seizure disorders are expected to be the same with IV therapy, although plasma concentration monitoring and dosage adjustment may be necessary.
Administer daily dosages >250 mg in divided doses.
Use of IV therapy for >14 days not established.
Use of IV valproate sodium for initial monotherapy has not been systematically studied; however, usual dosages and titration employed with oral therapy can be employed with parenteral therapy.
Monitor patients receiving dosages near the usual maximum recommended dosage of 60 mg/kg daily closely, particularly when enzyme-inducing drugs are not used concomitantly.
Simple or Complex Absence Seizures
Oral (conventional, delayed-, and extended-release preparations)Dosages apply to conventional (capsules and solution), delayed-release (tablets), and extended-release (tablets) dosage forms of valproic acid (active moiety), valproate sodium, and divalproex sodium.
Initially, 15 mg/kg daily.
Increase dosage by 5–10 mg/kg daily at weekly intervals, according to response and tolerability, up to maximum recommended dosage of 60 mg/kg daily.
IVMay employ IV therapy in patients in whom oral therapy temporarily is not feasible, but switch to oral administration as soon as clinically possible.
The usual total daily dosages are equivalent for IV or oral administration, and the doses and frequency of administration employed with oral therapy in seizure disorders are expected to be the same with IV therapy, although plasma concentration monitoring and dosage adjustment may be necessary.
Administer daily dosages >250 mg in divided doses.
Use of IV therapy for >14 days has not been studied to date.
Use of IV valproate sodium for initial monotherapy has not been systematically studied; however, usual dosages and titration employed with oral therapy can be employed with parenteral therapy.
Monitor patients receiving dosages near the usual maximum recommended dosage of 60 mg/kg daily closely, particularly when enzyme-inducing drugs are not used concomitantly.
Seizures Associated with Dravet Syndrome†
OralInitial dosages of 10–15 mg/kg daily (in 2–3 divided doses) with target daily dosages of 25–60 mg/kg daily have been used, based on clinical response, tolerability, and blood concentrations.
Adults
Seizure Disorders
Complex Partial Seizures
Oral (conventional, delayed-, and extended-release preparations)Dosages apply to conventional (capsules and solution), delayed-release (capsules and tablets), and extended-release (tablets) dosage forms of valproic acid (active moiety), valproate sodium, and divalproex sodium.
Initially, 10–15 mg/kg daily.
Increase dosage by 5–10 mg/kg daily at weekly intervals until seizures are controlled or adverse effects prevent further dosage increases, usually up to 60 mg/kg daily according to response and tolerability.
When used adjunctively, may continue concurrent anticonvulsant therapy, adjusting dosages according to response and tolerability. (See Interactions.)
Alternatively, may attempt to decrease dosage of the current anticonvulsant by 25% every 2 weeks, either starting concomitantly with initiation of valproic acid therapy or delayed by 1–2 weeks if there is a concern that seizures are likely to occur with a reduction.
Speed and duration of withdrawal of the current anticonvulsant can be highly variable; monitor patients closely during this period for increased seizure frequency.
IVMay employ IV therapy in patients in whom oral therapy temporarily is not feasible, but switch to oral administration as soon as clinically possible.
IV administration can be used for monotherapy or as adjunctive therapy in the management of seizure disorders.
The usual total daily dosages are equivalent for IV or oral administration, and the doses and frequency of administration employed with oral therapy in seizure disorders are expected to be the same with IV therapy, although plasma concentration monitoring and dosage adjustment may be necessary.
Administer daily dosages >250 mg in divided doses.
Use of IV therapy for >14 days not established.
Use of IV valproate sodium for initial monotherapy has not been systematically studied; however, usual dosages and titration employed with oral therapy can be employed with parenteral therapy.
Monitor patients receiving dosages near the usual maximum recommended dosage of 60 mg/kg daily closely, particularly when enzyme-inducing drugs are not used concomitantly.
Simple or Complex Absence Seizures
Oral (conventional, delayed-, and extended-release preparations)Dosages apply to conventional (capsules and solution), delayed-release (tablets), and extended-release (tablets) dosage forms of valproic acid (active moiety), valproate sodium, and divalproex sodium.
Initially, 15 mg/kg daily.
Increase dosage by 5–10 mg/kg daily at weekly intervals, according to response and tolerability, up to maximum recommended dosage of 60 mg/kg daily.
IVMay employ IV therapy in patients in whom oral therapy temporarily is not feasible, but switch to oral administration as soon as clinically possible.
The usual total daily dosages are equivalent for IV or oral administration, and the doses and frequency of administration employed with oral therapy in seizure disorders are expected to be the same with IV therapy, although plasma concentration monitoring and dosage adjustment may be necessary.
Administer daily dosages >250 mg in divided doses.
Use of IV therapy for >14 days not established.
Use of IV valproate sodium for initial monotherapy has not been systematically studied; however, usual dosages and titration employed with oral therapy can be employed with parenteral therapy.
Monitor patients receiving dosages near the usual maximum recommended dosage of 60 mg/kg daily closely, particularly when enzyme-inducing drugs are not used concomitantly.
Seizures Associated with Dravet Syndrome†
OralInitial dosages of 10–15 mg/kg daily (in 2–3 divided doses) with target daily dosages of 25–60 mg/kg daily have been used, based on clinical response, tolerability, and blood concentrations.
Seizure Disorders
Conversion from Divalproex Sodium Delayed-release (e.g., Depakote) to Extended-release (e.g., Depakote ER) Tablets
OralWhen converting a patient whose seizure disorder is controlled with divalproex sodium delayed-release tablets to the extended-release tablets, give the drug once daily using a total daily dose that is 8–20% higher than the corresponding delayed-release dosage that the patient was receiving.
For patients whose delayed-release daily dosage cannot be directly converted to a corresponding commercially available extended-release dosage, consider increasing the delayed-release total daily dosage to the next higher dosage before converting to the appropriate extended-release total daily dosage at the clinician’s discretion.
Refractory Status Epilepticus
Rectally†
400–600 mg of valproic acid has been administered by enema or in wax-based suppositories at 6-hour intervals.
Bipolar Disorder
Manic or Mixed Episodes
OralInitially, 750 mg daily in divided doses as delayed-release tablets (e.g., Depakote) or 25 mg/kg once daily as extended-release tablets (e.g., Depakote ER) for acute episodes.
For acute episodes, increase dosage as quickly as possible to achieve the lowest therapeutic dosage producing the desired clinical effect or desired plasma concentration; however, the manufacturers recommend that the dosage not exceed 60 mg/kg daily.
In clinical studies, dosed to clinical response with trough plasma concentrations of 50–125 mcg/mL.
Efficacy beyond 3 weeks not systematically evaluated; if continued, periodically reevaluate long-term usefulness and risk for the individual patient.
Safety of longer-term antimanic therapy is supported by data from record reviews involving approximately 360 patients treated for >3 months.
Dosing guidelines for maintenance therapy† are less evidence-based than those for acute therapy, and dosages lower than those employed for acute therapy occasionally have been used.
Migraine
Prophylaxis of Chronic Attacks
OralInitially, 500 mg once daily as extended-release tablets (e.g., Depakote ER).
Maintenance: After 1 week at the initial dosage of extended-release tablets, may increase dosage to 1 g daily. Some patients may benefit from dosages up to 1 g daily. No evidence of additional benefit with higher dosages.
If a patient requires smaller dosage adjustment than that available using the extended-release tablets, use the delayed-release tablets instead.
Schizophrenia†
Oral
In general, for adjunctive therapy, administer in the same dosages, and with the same resulting therapeutic plasma concentrations, as those for the management of seizure disorders.
Prescribing Limits
Pediatric Patients
Seizure Disorders
Oral
Usual maximum recommended dosage is 60 mg/kg daily; if therapeutic response not achieved, monitor plasma concentrations.
Adults
Seizure Disorders
Oral
Usual maximum recommended dosage is 60 mg/kg daily; if therapeutic response not achieved, monitor plasma concentrations.
Bipolar Disorder
Manic or Mixed Episodes
OralMaximum recommended dosage is 60 mg/kg daily.
Migraine
Prophylaxis of Chronic Attacks
OralMaximum recommended dosage is 1 g daily.
Special Populations
Hepatic Impairment
Because of substantially decreased protein binding, monitoring total (bound + unbound) drug concentrations may be misleading.
Renal Impairment
Dosage adjustment does not appear necessary.
Because of substantially decreased protein binding, monitoring total (bound + unbound) drug concentrations may be misleading.
Geriatric Patients
Reduce initial dosage because of a decrease in clearance of unbound valproic acid and possibility of greater sensitivity to adverse effects (e.g., somnolence); increase subsequent dosage more slowly.
Consider dosage reduction or discontinuance in geriatric patients with reduced food or fluid intake and in those with excessive somnolence. (See Somnolence in Geriatric Patients under Cautions and also see Geriatric Use under Cautions.)
Determine ultimate therapeutic dosage on the basis of tolerability and clinical response.
Gender
No dosage adjustment necessary based solely on gender.
Cautions for Valproic Acid
Contraindications
-
Hepatic disease or substantial hepatic dysfunction.
-
Patients with mitochondrial disorders caused by POLG mutations and children <2 years of age suspected of having a POLG-related disorder.
-
Known hypersensitivity to valproic acid, valproate sodium, divalproex sodium, or any ingredient in the respective formulation.
-
Urea cycle disorders. (See Urea Cycle Disorders [UCD] under Cautions.)
-
Use for prophylaxis of migraine headache in pregnant women. (See Pregnancy under Cautions.)
Warnings/Precautions
Warnings
Hepatotoxicity
May cause serious and potentially fatal hepatotoxicity. (See Hepatotoxicity in Boxed Warning.)
Children and patients receiving multiple anticonvulsants or those with congenital metabolic disorders, severe seizure disorders accompanied by mental retardation, or organic brain disease may be at particular risk.
Higher incidence of acute liver failure and resultant deaths reported in patients with hereditary neurometabolic syndromes caused by POLG mutations than in those without such disorders; most cases identified in children and adolescents.
Use with caution in patients with a history of hepatic disease.
Immediately discontinue valproic acid if substantial hepatic dysfunction, suspected or apparent, is present. In some cases, hepatic dysfunction has progressed despite discontinuance of the drug.
Pancreatitis
May cause life-threatening pancreatitis. (See Pancreatitis in Boxed Warning.)
Urea Cycle Disorders (UCD)
Potentially fatal hyperammonemic encephalopathy can occur following initiation of therapy in patients with UCD, a group of uncommon genetic abnormalities, particularly ornithine transcarbamylase deficiency. (See Contraindications under Cautions.)
Plasma ammonia concentrations not systematically studied following IV administration; however, hyperammonemia with encephalopathy reported in at least 2 patients who received IV infusions of valproate sodium.
Advise patients to contact a clinician promptly if symptoms of this disorder (e.g., lethargy, vomiting, changes in mental status) develop.
If such symptoms are present, determine plasma ammonia concentrations, and, if increased, discontinue therapy.
Initiate appropriate treatment for hyperammonemia and evaluate the patient for an underlying UCD.
Prior to the initiation of therapy, consider evaluating for UCD in patients with: a history of unexplained encephalopathy or coma, encephalopathy associated with a protein load, pregnancy-related or postpartum encephalopathy, unexplained mental retardation, or history of elevated plasma ammonia or glutamine concentrations; patients with cyclical vomiting and lethargy, episodic extreme irritability, ataxia, low BUN concentration, or protein avoidance; patients with a family history of UCD or unexplained infant deaths (particularly males); or those with other signs or symptoms of UCD.
Asymptomatic elevation of ammonia concentrations is more common than symptomatic hyperammonemia. In patients with asymptomatic elevations, closely monitor plasma ammonia concentrations and, if elevations persist, consider discontinuance of the drug.
Fetal Risk
Can produce NTDs and other structural malformations (e.g., craniofacial defects, cardiovascular malformations, anomalies involving various body systems) following in utero exposure. In addition, decreased IQ and other cognitive impairments observed in children exposed in utero. (See Fetal Risk in Boxed Warning.)
In animal studies, adverse fetal effects, including structural malformations (e.g., skeletal, cardiac, urogenital), neural tube closure defects, intrauterine growth retardation, neurobehavioral abnormalities, and death, observed.
Do not use in pregnant women for prevention of migraine headaches; use only in pregnant women with epilepsy or bipolar disorder if absolutely necessary. (See Pregnancy under Cautions.)
Suicidality Risk
Increased risk of suicidality (suicidal ideation or behavior) observed in an analysis of studies using various anticonvulsants in patients with epilepsy, psychiatric disorders (e.g., bipolar disorder, depression, anxiety), and other conditions (e.g., migraine, neuropathic pain); risk in patients receiving anticonvulsants (0.43%) was approximately twice that in patients receiving placebo (0.24%). Increased suicidality risk was observed ≥1 week after initiation of anticonvulsant therapy and continued through 24 weeks. Risk was higher for patients with epilepsy compared with those receiving anticonvulsants for other conditions.
Closely monitor all patients currently receiving or beginning anticonvulsant therapy for changes in behavior that may indicate emergence or worsening of suicidal thoughts or behavior or depression.
Balance risk of suicidality with the risk of untreated illness. Epilepsy and other illnesses treated with anticonvulsants are themselves associated with morbidity and mortality and an increased risk of suicidality. If suicidal thoughts or behavior emerge during anticonvulsant therapy, consider whether these symptoms may be related to the illness itself. (See Advice to Patients.)
Brain Atrophy
Cerebral and cerebellar atrophy (or pseudoatrophy) reported during postmarketing experience; may be irreversible or reversible. Some patients recovered with permanent sequelae.
Monitor patients routinely for motor and cognitive impairments during therapy; if any manifestations of brain atrophy develop or are suspected, evaluate whether therapy should be continued.
Cerebral atrophy also reported in children exposed in utero to valproic acid. (See Pregnancy under Cautions.)
Interaction with Carbapenem Antibiotics
Carbapenem antibiotics (e.g., ertapenem, imipenem, meropenem) may reduce plasma valproic acid concentrations to subtherapeutic levels, resulting in loss of seizure control. (See Specific Drugs and Laboratory Tests under Interactions.)
Somnolence in Geriatric Patients
Somnolence reported, particularly in geriatric patients. (See Advice to Patients.)
In geriatric patients with dementia, somnolence occurred in a significantly higher proportion of patients receiving valproic acid compared with those receiving placebo. Dehydration also occurred in more valproic acid-treated patients, although the difference was not clinically significant. In some patients (approximately half) with somnolence, associated reduced nutritional intake and weight loss occurred. (See Geriatric Use under Cautions.)
In geriatric patients, increase dosage more slowly and monitor patients regularly for fluid and nutritional intake, dehydration, somnolence, and other adverse effects. (See Geriatric Patients under Dosage and Administration.)
Thrombocytopenia
Frequency of valproic acid-associated adverse effects, particularly elevated liver enzyme concentrations and thrombocytopenia, may be dose-related.
The probability of thrombocytopenia appears to increase substantially at total plasma valproic acid concentrations ≥110 mcg/mL (females) or ≥135 mcg/mL (males).
Weigh the therapeutic benefit of relatively high dosages with the possibility of dose-related thrombocytopenia and other adverse effects.
Monitor platelet counts and coagulation tests before initiating valproic acid therapy and periodically during therapy. Such monitoring is also recommended prior to planned (i.e., elective) surgery.
Consider thromboelastography as a more reliable method to assess the effects of valproic acid on coagulation.
If clinical evidence of hemorrhage, bruising, or a disorder of hemostasis/coagulation occurs during therapy, reduce dosage or withdraw the drug pending further evaluation.
Hypothermia
Hypothermia (unintentional drop in body core temperature to <35°C) reported in association with valproic acid therapy both in conjunction with and in the absence of hyperammonemia (see Hyperammonemia under Cautions). May also occur in patients receiving concurrent topiramate and valproic acid after starting topiramate therapy or increasing the daily topiramate dosage. (See Hyperammonemia and Encephalopathy associated with Concurrent Topiramate under Cautions.)
Consider discontinuing valproic acid therapy in patients who develop manifestations of hypothermia, including lethargy, confusion, coma, and significant alterations in other major organ systems (e.g., cardiovascular and respiratory systems). Include examination of blood ammonia concentrations in clinical assessment and management of hypothermia. (See Urea Cycle Disorders [UCD] under Cautions.)
Hyperammonemia
Hyperammonemia reported; may be present despite normal liver function tests. In patients who develop unexplained lethargy and vomiting or changes in mental status, consider hyperammonemic encephalopathy and measure blood ammonia concentrations. Also consider hyperammonemia in patients who present with hypothermia.
If ammonia concentrations are increased, discontinue valproic acid therapy and initiate appropriate treatment interventions. Also evaluate hyperammonemic patients for possible underlying UCD. (See Urea Cycle Disorders [UCD] under Cautions.)
Asymptomatic elevations of ammonia concentrations are more common and, when present, require close monitoring of plasma ammonia concentrations.
Hyperammonemia and Encephalopathy Associated with Concurrent Topiramate
Concomitant administration of topiramate and valproic acid has been associated with hyperammonemia with or without encephalopathy in patients who have previously tolerated either drug alone. Clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function accompanied by lethargy or vomiting. Hypothermia also may be a manifestation of hyperammonemia.
In most cases, signs and symptoms abated upon discontinuance of either drug. It is not known if topiramate monotherapy is associated with hyperammonemia. Patients with inborn errors of metabolism or reduced hepatic mitochondrial activity may be at increased risk for hyperammonemia with or without encephalopathy.
In patients who develop unexplained lethargy, vomiting, or changes in mental status, consider hyperammonemic encephalopathy and measure blood ammonia concentration. (See Urea Cycle Disorders [UCD] under Cautions, see Hyperammonemia under Cautions, and see Specific Drugs and Laboratory Tests under Interactions.)
Posttraumatic Seizures
Fatality rate was higher for valproic acid (IV valproate sodium then oral valproic acid) versus IV phenytoin in patients with acute head injuries receiving the drugs for prevention of posttraumatic seizures; causal relationship not established.
Prudent to not use IV valproate sodium in acute head trauma for posttraumatic seizure prophylaxis pending further study.
Sensitivity Reactions
Multi-organ Hypersensitivity Reactions
Multi-organ hypersensitivity reactions reported rarely in close temporal association to initiation of valproic acid therapy in adult and pediatric patients (median time to detection: 21 days; range: 1–40 days). Many reported cases resulted in hospitalization and at least one death.
Patients typically, although not exclusively, present with fever and rash associated with other organ system involvement. Other associated manifestations may include lymphadenopathy, hepatitis, liver function test abnormalities, hematologic abnormalities (e.g., eosinophilia, thrombocytopenia, neutropenia), pruritus, nephritis, oliguria, hepatorenal syndrome, arthralgia, and asthenia. This disorder is variable in its expression, and signs and symptoms associated with other organ systems also may occur.
If a multi-organ hypersensitivity reaction is suspected, discontinue valproic acid and initiate alternative treatment. Although the existence of cross sensitivity with other drugs that produce this disorder is unclear, experience with drugs associated with multi-organ hypersensitivity would indicate this to be a possibility.
Other Hypersensitivity Reactions
Anaphylaxis, photosensitivity, generalized pruritus, Stevens-Johnson syndrome, erythema nodosum, and erythema multiforme reported.
Rare cases of toxic epidermal necrolysis, including a fatal case in a 6-month-old infant receiving valproic acid therapy; however, infant was receiving other drugs concomitantly.
General Precautions
Discontinuance of Therapy
Do not discontinue anticonvulsant drugs abruptly in patients, including pregnant women, receiving the drugs to prevent major seizures; strong possibility of precipitating status epilepticus with attendant hypoxia and threat to life. (See Pregnancy under Cautions.)
Therapeutic Drug Monitoring
Since valproic acid may interact with concurrently administered drugs that are capable of hepatic enzyme induction, periodic determinations of plasma concentrations of valproic acid and concomitant drugs are recommended during the early course of therapy. (See Interactions.)
Effect on HIV and Cytomegalovirus (CMV) Replication
Appears to stimulate replication of HIV and CMV under certain experimental conditions; however, clinical importance not known.
Relevance to patients receiving maximally suppressive antiretroviral therapy also is not known.
Consider these effects when interpreting test results concerning the clinical condition of patients with HIV (plasma HIV RNA levels [viral load]) or CMV infection.
Medication Residue in Stool
Medication residue in stool reported rarely with divalproex sodium formulations (e.g., Depakote, Depakote ER, Depakote Sprinkle Capsules); some cases occurred in the presence of diarrhea. Some patients had anatomic (e.g., ileostomy, colostomy) or functional GI disorders that decrease GI transit times. Monitor plasma valproic acid concentrations and clinical status in such patients; consider alternative therapy if clinically necessary.
Specific Populations
Pregnancy
Category D (epilepsy, bipolar disorder); category X (migraine prophylaxis). (See Fetal Risk in Boxed Warning.)
North American Antiepileptic Drug (NAAED) Pregnancy Registry at 888-233-2334 (for patients); NAAED registry information also available on the website [Web].
Risk of major congenital malformations, particularly NTDs; risk appears to be greatest during the first trimester of pregnancy. Rate of major malformations in infants exposed in utero to valproic acid is fourfold higher than that observed in infants exposed to other anticonvulsants.
CDC estimates the fetal risk of spina bifida in valproic acid-treated pregnant women to be approximately 1–2%; estimated risk of spina bifida in the general population is 0.06–0.07%.
Folic acid supplementation in pregnant women may decrease risk of congenital NTDs. Not known whether risk of NTDs in offspring of women receiving valproic acid is specifically reduced by folic acid supplementation. Folic acid supplementation prior to conception and during pregnancy should be routinely recommended in women.
In utero exposure to valproic acid also appears to increase risk of adverse cognitive effects in children. Reduced IQ scores and other cognitive deficits (e.g., decreased memory, verbal and nonverbal abilities, cognitive fluency and originality, or executive functions; delayed mental development; increased special education needs) observed in several observational studies in children exposed in utero to valproic acid compared with those with no exposure. Dose-dependent effect observed, with higher dosages associated with worse cognitive outcomes. Long-term effects of such exposure not known; also not known whether risk occurs when fetal exposure is limited with respect to duration or timing (e.g., first trimester) during pregnancy.
Possible association between in utero valproic acid exposure and developmental delay, autism, and/or autism spectrum disorders.
Potentially fatal neonatal clotting abnormalities and hepatic failure have occurred rarely with maternal exposure to the drug.
Do not use in pregnant women for prevention of migraine headaches; use in pregnant women with epilepsy or bipolar disorder only if other treatments have failed to provide adequate symptom relief or are otherwise unacceptable.
Use in women of childbearing potential only if the drug is clearly shown to be essential in the management of their medical condition; use effective contraception. Consider alternative therapies in women contemplating pregnancy.
Tests to detect neural tube and other malformations using current accepted procedures should be considered a part of routine prenatal care and be offered to pregnant women receiving valproic acid.
If used during pregnancy, monitor clotting parameters closely.
Do not discontinue anticonvulsants in pregnant women in whom the drugs are administered to prevent major seizures because of the strong possibility of precipitating status epilepticus with attendant hypoxia and threat to life.
Lactation
Distributes into milk. Caution advised.
Pediatric Use
Experience with oral valproic acid in the management of seizures indicates that children <2 years of age are at an increased risk of developing fatal hepatotoxicity. (See Hepatotoxicity in Boxed Warning.)
Use with extreme caution and only as single-agent therapy in such children, and weigh the benefits of therapy against the risks.
The incidence of fatal hepatotoxicity decreases considerably in progressively older patient groups (i.e., >2 years of age).
Younger children, especially those receiving enzyme-inducing drugs, will require larger maintenance dosages to attain targeted total and unbound valproic acid concentrations for the management of seizures. The variability in free fraction limits the clinical usefulness of monitoring total serum valproic acid concentrations alone.
Interpretation of valproic acid concentration in children should include consideration of factors that affect hepatic metabolism and protein binding.
Safety and efficacy of valproic acid for complex partial seizures not established in pediatric patients <10 years of age.
Efficacy of extended-release tablets (e.g., Depakote ER) for mania or migraine prophylaxis in pediatric patients not demonstrated in placebo-controlled studies.
Safety and tolerability of divalproex sodium in pediatric patients appear similar to those in adults.
Safety of the injection has not been studied in pediatric patients <2 years of age. If a decision is made to use the injection in this age group, use with extreme caution and only as monotherapy, and weigh potential benefits against possible risks.
Geriatric Use
No geriatric patients >65 years of age were enrolled in controlled trials of oral valproic acid for the treatment of manic episodes associated with bipolar disorder. In a case review study, a higher percentage of patients >65 years of age reported accidental injury, infection, pain, somnolence, and tremor compared with younger patients.
Increased risk of somnolence in geriatric patients. (See Somnolence in Geriatric Patients under Cautions.)
Safety and efficacy of valproic acid for the prevention of migraine headaches in geriatric patients >65 years of age not established.
No unique safety concerns were identified in geriatric patients >65 years of age receiving IV valproate sodium in clinical trials.
Dosage adjustments are necessary in geriatric patients. (See Geriatric Patients under Dosage and Administration.)
Regularly monitor geriatric patients for fluid and nutritional intake, dehydration, somnolence, and other adverse effects.
Hepatic Impairment
Liver disease impairs the capacity to eliminate valproic acid. (See Elimination: Special Populations, under Pharmacokinetics.)
Substantially increased unbound (active) drug fraction because of decreased albumin. Because of decreased protein binding, monitoring total (bound + unbound) drug concentrations may be misleading. (See Distribution: Special Populations, under Pharmacokinetics.)
Contraindicated in patients with hepatic disease or substantial hepatic dysfunction. Use with caution in patients with a history of hepatic disease. (See Hepatotoxicity in Boxed Warning and also see Hepatotoxicity under Cautions.)
Common Adverse Effects
The most frequent adverse effects following initiation of therapy are nausea, vomiting, and indigestion.
Eructation, fecal incontinence, gastroenteritis, glossitis, flatulence, hematemesis, periodontal abscess, tooth disorder, dry mouth, stomatitis, and constipation may occur.
Somnolence, asthenia, dizziness, and tremor generally are the most frequently reported adverse nervous system effects.
In addition, IV infusion may cause local effects at the injection site and effects associated with the rate of infusion.
Drug Interactions
CYP microsomal-mediated oxidation is a relatively minor metabolic pathway.
Drugs Affecting Hepatic Enzymes
Drugs affecting expression of hepatic enzymes, particularly glucuronyltransferases, may increase valproic acid clearance.
Phenobarbital or primidone, phenytoin, or carbamazepine can double valproic acid clearance.
Increase monitoring of valproic acid and concomitantly used drug concentrations whenever enzyme-inducing drugs are introduced or withdrawn.
Inhibitors of CYP isoenzymes are unlikely to have a clinically important effect on valproic acid clearance.
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
Limited pharmacokinetic studies reveal little to no interaction following concomitant administration |
|
|
Acyclovir |
May reduce plasma anticonvulsant concentrations to subtherapeutic levels; an increase in seizure frequency and a worsening in the EEG may be observed |
Use concomitantly with caution |
|
Alcohol |
Additive CNS depression may occur |
Use concomitantly with caution |
|
Amitriptyline |
Decreased plasma clearance of amitriptyline and nortriptyline (the pharmacologically active metabolite of amitriptyline) |
Consider monitoring concentrations and reducing dosage of amitriptyline during concomitant use |
|
Antacids |
Limited pharmacokinetic studies reveal little to no interaction during concomitant administration |
|
|
Anticoagulants, oral (warfarin) |
May increase unbound fraction of warfarin |
Clinical relevance unknown; monitor coagulation tests during concomitant use |
|
Anticonvulsants (phenobarbital, phenytoin, and primidone) |
Additive, potentially severe CNS depression may occur (particularly with phenobarbital and primidone) Concomitant administration of valproic acid and phenobarbital (or primidone which is metabolized to phenobarbital) can result in increased plasma phenobarbital concentrations and excessive somnolence May displace phenytoin from protein binding and inhibit its metabolism |
Observe closely for possible neurotoxicity if phenobarbital or primidone is used concomitantly Combination can produce CNS depression (possibly severe) even without substantial increases in serum concentrations of either drug Observe for breakthrough seizures during concomitant phenytoin use; adjust dosage accordingly Since valproic acid also may interact with other anticonvulsants, it is advisable to monitor plasma concentrations of concomitantly administered anticonvulsants during initial valproic acid therapy |
|
Aspirin |
Aspirin can increase unbound (active) valproic acid fourfold Possible combined effects on platelets |
Use concomitantly with caution |
|
Cannabidiol |
Increased risk of hepatic enzyme elevations No effect on systemic exposure of valproate |
If hepatic enzyme elevations occur, consider dosage reduction or discontinuance of cannabidiol and/or valproate |
|
Carbamazepine |
Decreased serum carbamazepine concentrations and increased carbamazepine-10,11-epoxide metabolite concentrations May decrease plasma valproic acid concentration by altering its clearance, which may be clinically important Discontinuance of carbamazepine following concomitant carbamazepine/valproic acid therapy has been reported to result in increased valproic acid concentrations |
Use concomitantly with caution; observe for possible carbamazepine CNS toxicity (e.g., acute psychotic reaction) Closely monitor valproic acid concentrations whenever carbamazepine is initiated or discontinued |
|
Carbapenem antibiotics (e.g., ertapenem, imipenem, meropenem) |
May cause a clinically important and marked decrease in plasma valproic acid concentrations, which may result in loss of seizure control |
Avoid combined therapy, if possible If concurrent therapy is necessary, frequently monitor valproic acid concentrations after carbapenem is initiated or discontinued; more frequent monitoring during concurrent therapy also is recommended by some clinicians Consider alternative anti-infective or anticonvulsant therapy if valproic acid concentrations decrease substantially or seizure control deteriorates |
|
Chlorpromazine |
May increase trough plasma valproic acid concentrations (e.g., by 15%) |
|
|
Clonazepam |
Concomitant use may precipitate absence status in patients with a history of absence-type seizures |
Consider avoiding concomitant use |
|
Clozapine |
Interaction unlikely |
|
|
CNS depressants |
Possible additive CNS depression |
Use concomitantly with caution |
|
Diazepam |
Displaces diazepam from its albumin binding sites and also inhibits its metabolism; increases free fraction of diazepam Possible additive CNS depression |
Use concomitantly with caution |
|
Ethosuximide |
Inhibits the metabolism of ethosuximide |
Monitor plasma concentrations of valproic acid and ethosuximide closely during concomitant use, especially if receiving other concomitant anticonvulsant therapy |
|
Felbamate |
May increase mean peak plasma valproic acid concentration |
A decrease in valproic acid dosage may be required when initiating concomitant felbamate therapy |
|
Haloperidol |
No clinically important effect on trough valproic acid concentrations |
|
|
H2-receptor antagonists (cimetidine, ranitidine) |
Valproic acid clearance unaffected |
|
|
Lamotrigine |
Valproic acid inhibits lamotrigine metabolism; the elimination half-life of lamotrigine is increased (by 165%) during concurrent administration Serious skin reactions (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis) also reported during concurrent administration |
Reduce lamotrigine dosage during concurrent administration |
|
Lithium |
Lithium steady-state pharmacokinetics unaffected |
|
|
Lorazepam |
May decrease lorazepam clearance (e.g., by 17%); unlikely to be clinically important |
|
|
MAO inhibitors and other antidepressants |
Valproic acid may potentiate the effects of MAO inhibitors and other antidepressants. |
Dosage reduction of these drugs may be necessary if valproic acid is administered to patients receiving antidepressants |
|
Nortriptyline |
During concurrent administration of valproic acid and amitriptyline, decreased plasma clearance of amitriptyline and nortriptyline (the pharmacologically active metabolite of amitriptyline) reported |
Consider monitoring nortriptyline concentrations and reducing dosage of nortriptyline during concomitant use |
|
Oral contraceptives |
Pharmacokinetic interaction unlikely |
|
|
Phenytoin |
Valproic acid has been associated both with decreased plasma phenytoin concentrations and increased seizure frequency and with increased plasma concentrations of free phenytoin and phenytoin intoxication |
Important to monitor plasma phenytoin concentrations whenever valproic acid is added to or withdrawn from the patient’s therapy and adjust the dosage of phenytoin as required |
|
Rifampin |
May increase valproic acid clearance (e.g., by 40%) |
Valproic acid dosage adjustment may be required during concurrent rifampin therapy |
|
Test, for urinary ketones |
A ketone metabolite in the urine of patients receiving valproic acid may produce false-positive results for urine ketones |
|
|
Test, for thyroid function |
Valproic acid reportedly alters thyroid function test results, but clinical importance is not known |
|
|
Tolbutamide |
In vitro, addition of tolbutamide to plasma samples of patients receiving valproic acid resulted in an increase in the unbound tolbutamide fraction from 20% to 50% |
Clinical relevance unknown |
|
Topiramate |
Concurrent administration of valproic acid and topiramate associated with hyperammonemia with or without encephalopathy in patients who have tolerated either drug alone Clinical symptoms of hyperammonemic encephalopathy often include acute alterations in level of consciousness and/or cognitive function with lethargy or vomiting; hypothermia may also be a manifestation of hyperammonemia |
Measure blood ammonia concentrations in patients who develop possible symptoms of hyperammonemia (unexplained lethargy, vomiting, or changes in mental status) or hypothermia; promptly treat hyperammonemia, if present, and discontinue valproic acid; consider valproic acid discontinuance in patients with hypothermia (see Cautions) |
|
Zidovudine |
Valproic acid inhibits glucuronidation of zidovudine and increases its oral bioavailability; such concomitant administration may alter the efficacy and toxicity profile of zidovudine |
Valproic Acid Pharmacokinetics
Absorption
Bioavailability
Valproic acid: Rapidly and almost completely absorbed from the GI tract.
Equivalent oral doses of valproic acid and divalproex sodium preparations (but not extended-release tablets) deliver equivalent amounts of valproate ion systemically following oral administration.
Divalproex sodium extended-release tablets have decreased oral bioavailability relative to delayed-release tablets, averaging about 89% relative to delayed-release tablets.
Oral, valproate sodium: Rapidly converted to valproic acid in the stomach.
Oral, divalproex sodium delayed-release tablets: Upon passage of the tablets into the upper small intestine, divalproex sodium dissociates into valproic acid.
Oral, divalproex sodium extended-release tablets: Divalproex sodium dissociates into valproic acid in the GI tract.
Peak concentration usually attained 1–4 hours following a single oral dose of valproic acid or valproate sodium, 3–5 hours following a single oral dose of divalproex sodium, or 6–14 hours after oral administration of multiple doses of divalproex sodium extended-release tablets.
Equivalent valproic acid dosages as the IV injection, administered over 1 hour, or various conventional or delayed-release oral formulations are expected to result in equivalent peak and trough plasma concentrations and total systemic exposure to valproic acid.
Food
Absorption of valproic acid is delayed but not decreased by administration with meals; administration of the drug with milk products does not affect the rate or degree of absorption.
Administration of divalproex sodium with food is expected to slow absorption but not affect the extent of absorption.
Absolute bioavailability of divalproex sodium extended-release tablets after a meal is about 90%.
Plasma Concentrations
An anticonvulsant therapeutic range of 50–100 mcg/mL of total (bound and unbound) valproic acid has been suggested; seizure control occasionally may occur with lower or higher concentrations, but >150 mcg/mL usually is toxic.
For acute manic episodes in bipolar disorder, usually dosed to clinical response with trough plasma concentrations of 50–125 mcg/mL.
Distribution
Extent
Valproic acid is rapidly distributed; distribution appears to be restricted to plasma and rapidly exchangeable extracellular water.
Detected in CSF.
Detected in saliva.
Crosses the placenta.
Distributes into milk.
Plasma Protein Binding
Plasma protein binding of valproic acid is concentration dependent; the free fraction of drug increases from 10% to 18.5% as the plasma concentration increases.
Special Populations
Hepatic impairment: Increased unbound (active) drug fraction (2–2.6-fold increase) because of decreased albumin.
Renal impairment: Substantially decreased protein binding.
Elimination
Metabolism
Valproic acid is metabolized principally in the liver by beta and omega oxidation.
Elimination Route
Valproic acid metabolites are excreted in urine; <3% of an administered dose is excreted in urine unchanged.
Small amounts also are excreted in feces and in expired air.
Half-life
Valproic acid: 5–20 hours.
Special Populations
Neonates: Markedly decreased clearance compared with older children and adults; elimination half-life in neonates <10 days of age ranged from 10–67 hours.
Children 3 months to 10 years of age: 50% increased clearance (on a proportionate weight basis) relative to older children and adults.
Geriatric patients: Clearance may be decreased.
Hepatic impairment: Impairs the ability to eliminate valproic acid; half-life is increased from 12 to 18 hours in hepatic disease. Clearance of free valproic acid was decreased by 50% in cirrhosis and by 16% in acute hepatitis.
Renal impairment: Clearance of unbound (active) drug is decreased by 27% in patients with renal failure. Hemodialysis usually reduces valproic acid concentrations by about 20%.
Stability
Storage
Oral
Capsules
Valproic acid: Tight containers at 15–30°C. Depakene: Tight containers at 15–25°C.
Divalproex sodium capsules containing coated particles (Depakote Sprinkle): <25°C.
Tablets
Divalproex sodium delayed-release tablets: Tight, light-resistant containers at a temperature <30°C.
Divalproex sodium extended-release tablets: 25°C, but may be exposed to temperatures ranging from 15–30°C.
Solution
Valproate sodium: Tight containers at <30°C; avoid freezing.
Parenteral
Injection
15–30°C.
Discard unused portions of the solution.
When stored in glass or PVC containers at 15–30°C, injection that has been further diluted with at least 50 mL of 5% dextrose injection, 0.9% sodium chloride injection, or lactated Ringer’s injection is stable for at least 24 hours.
Actions
-
Mechanism of action not known.
-
Effects may be related, at least in part, to increased brain concentrations of the inhibitory neurotransmitter, GABA.
-
May inhibit neuronal activity by increasing potassium conductance.
Advice to Patients
-
Importance of providing copy of written patient information (medication guide) each time valproic acid is dispensed; importance of patient reading this information prior to taking the drug.
-
Risk of suicidality (anticonvulsants, including valproic acid, may increase risk of suicidal thoughts or actions in about 1 in 500 people). Importance of patients, family, and caregivers being alert to day-to-day changes in mood, behavior, and actions and immediately informing clinician of any new or worrisome behaviors (e.g., talking or thinking about wanting to hurt oneself or end one’s life, withdrawing from friends and family, becoming depressed or experiencing worsening of existing depression, becoming preoccupied with death and dying, giving away prized possessions).
-
Warn patients and caregivers that serious or fatal hepatotoxicity may be preceded by symptoms such as malaise, weakness, lethargy, facial edema, anorexia, nausea, vomiting, abdominal pain, diarrhea, and/or jaundice and to contact a clinician promptly if such symptoms occur. (See Hepatotoxicity in Boxed Warning.)
-
Advise pregnant women and women of childbearing potential that the drug can cause major birth defects such as NTDs (e.g., spina bifida) and decreased IQ in children exposed in utero. Advise such women of alternative therapeutic options. Advise women of childbearing potential to use effective contraceptive methods during valproic acid therapy.
-
Importance of women immediately informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of clinicians informing women about the existence of and encouraging enrollment in pregnancy registries. (See Pregnancy under Cautions.)
-
Warn patients and caregivers that abdominal pain, nausea, vomiting, and/or anorexia can be symptoms of pancreatitis and therefore require prompt medical evaluation. (See Pancreatitis in Boxed Warning.)
-
Importance of advising patients to notify a clinician promptly if symptoms of hyperammonemic encephalopathy (e.g., lethargy, vomiting, changes in mental status) develop. (See Urea Cycle Disorders [UCD] under Cautions.)
-
In patients receiving divalproex sodium formulations (e.g., Depakote, Depakote ER, Depakote Sprinkle Capsules), importance of instructing patients to notify their clinician if they notice any medication residue in their stool.
-
Potential for drug to impair mental alertness or physical coordination; avoid driving or operating machinery until effects are known.
-
Importance of informing patients, including pregnant women, not to suddenly stop taking valproic acid without first talking to their clinician since stopping the drug suddenly can cause serious problems, including seizures.
-
Risk of multi-organ hypersensitivity reaction. Importance of advising patients that a fever associated with other organ system involvement (such as rash or lymphadenopathy) may be drug-related and should be reported to the clinician immediately.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
250 mg (of valproic acid) per 5 mL* |
Valproate Sodium Oral Solution |
|
|
Parenteral |
Injection, for IV use |
100 mg (of valproic acid) per mL* |
Valproate Sodium Injection |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
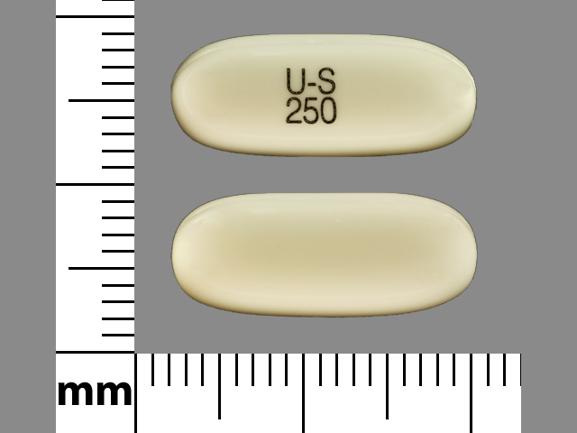
Capsules |
250 mg* |
Valproic Acid Capsules |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules (containing coated particles) |
equivalent to valproic acid 125 mg* |
Depakote Sprinkle Capsules |
AbbVie |
|
Divalproex Sodium Capsules (Sprinkle) |
||||
|
Tablets, delayed-release |
equivalent to valproic acid 125 mg* |
Depakote |
AbbVie |
|
|
Divalproex Sodium Delayed-Release Tablets |
||||
|
equivalent to valproic acid 250 mg* |
Depakote |
AbbVie |
||
|
Divalproex Sodium Delayed-Release Tablets |
||||
|
equivalent to valproic acid 500 mg* |
Depakote |
AbbVie |
||
|
Divalproex Sodium Delayed-Release Tablets |
||||
|
Tablets, extended-release |
equivalent to valproic acid 250 mg* |
Depakote ER |
AbbVie |
|
|
Divalproex Sodium Extended-Release Tablets |
||||
|
equivalent to valproic acid 500 mg* |
Depakote ER |
AbbVie |
||
|
Divalproex Sodium Extended-Release Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Aimovig
Learn about Aimovig (erenumab-aooe) a once-monthly, injectable medication that can be ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Qulipta
Qulipta is used to help prevent episodic or chronic migraine headaches in adults. Qulipta is an ...
Caplyta
Caplyta is used to treat schizophrenia or depression associated with bipolar disorder. It is taken ...
Ubrelvy
Ubrelvy (ubrogepant) tablets are used for the acute treatment of migraine. Includes Ubrelvy side ...
Nurtec ODT
Nurtec ODT (rimegepant) is used to treat acute migraines and prevent episodic migraines, by ...
Vraylar
Vraylar is a once a day antipsychotic medication used to treat mental health or mood disorders ...
Abilify
Abilify (aripiprazole) is an antipsychotic medication used to treat schizophrenia, bipolar I ...
Seroquel
Seroquel is used to treat the symptoms of schizophrenia, bipolar disorder and major depressive ...
More about valproic acid
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (65)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: fatty acid derivative anticonvulsants
- Breastfeeding
- En español
Patient resources
Professional resources
- Valproate prescribing information
- Valproic Acid Capsules (FDA)
- Valproic Acid Oral Solution (FDA)
- Valproic Acid Syrup (FDA)