Diabetic Gastroparesis
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
What is diabetic gastroparesis?
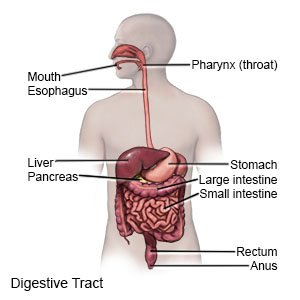
Diabetic gastroparesis is a type of nerve damage that slows digestion. High blood sugar levels from diabetes can damage nerves and tissues in your stomach. The damage prevents your stomach from emptying normally. Gastroparesis is also called delayed gastric emptying.
 |
What increases my risk for diabetic gastroparesis?
- History of type 1 or type 2 diabetes for at least 5 years
- Eye, nerve, or kidney problems due to diabetes
What are the signs and symptoms of diabetic gastroparesis?
Your symptoms may be worse if you drink alcohol or smoke. You may have any of the following:
- Constipation that may be replaced, at times, by diarrhea
- High or low blood sugar levels that you cannot control
- Nausea, vomiting, or loss of appetite
- Bloated or early full feeling while you eat
- Sudden cramps, swelling, or pain in your abdomen
- Weight loss without trying
- Heartburn
How is diabetic gastroparesis diagnosed?
Your healthcare provider will feel your abdomen and ask about your diabetes. Tell him or her about all medicines you currently take. Certain medicines can affect how your digestive system works. Examples include opioids, tricyclic antidepressants, and certain COPD or asthma medicines. Some medicines used to treat type 2 diabetes may also affect your digestive system. Make sure your provider knows about all your current medicines. You may also need any of the following tests:
- A gastric emptying breath test (GEBT) will show how fast food moves from your stomach to your small intestine. The test measures the amount of carbon in your breath after you eat a meal prepared by healthcare providers.
- An x-ray or ultrasound may show how your stomach is working. You may be given a chalky liquid to drink before the pictures are taken. This liquid helps your stomach and intestines show up clearly on the monitor.
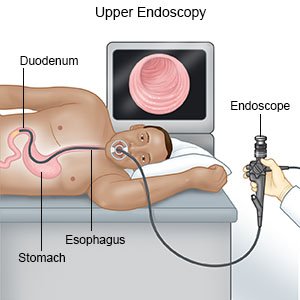
- An endoscopy may show what is causing your digestive problems. A scope is used to show images of the inside of your stomach. A scope is a thin, bendable tube with a light and camera on the end. Samples may be taken from your digestive tract and sent to a lab for tests.
- A scintigraphy , or gastric-emptying scan, measures how quickly food moves out of your stomach. A slightly radioactive substance is placed in food. The amount of radiation is small and safe. You eat the food and then lie under a machine that takes pictures of the food inside your stomach. Pictures will be taken every 15 minutes, up to 4 hours after you eat, or as directed.
Related medications
Tresiba
Tresiba (insulin degludec) is used to treat diabetes mellitus. Includes Tresiba side effects ...
Metformin
Metformin is an oral diabetes medicine used together with diet and exercise to improve blood sugar ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Rybelsus
Rybelsus tablets are used to improve blood sugar control in adults with type 2 diabetes, and may ...
Mounjaro
Mounjaro is used for type 2 diabetes to help lower blood sugar levels. Mounjaro has also been shown ...
Januvia
Januvia is used to treat type 2 diabetes. Learn about side effects, interactions and indications.
Victoza
Victoza helps control blood sugar levels and reduce the risk of serious heart problems in people ...
Jardiance
Jardiance (empagliflozin) is used to treat type 2 diabetes, chronic kidney disease and reduce the ...
How is diabetic gastroparesis treated?
Your healthcare provider may change one or more of your current medicines. Do not change your medicines without direction from your provider. Any of the following may also be used to treat gastroparesis:
- Medicines:
- Motility medicines help your stomach muscles move food and liquids out of your stomach faster. These medicines also may help you digest food better.
- Nausea medicine helps calm your stomach and prevent vomiting.
- An antibiotic may be given for a short time to help your stomach empty more quickly.
- A feeding tube may be needed if your stomach cannot process food. You may need the feeding tube for a short time, until your stomach starts working properly. You may instead need a long-term feeding tube if your gastroparesis is severe. Ask for more information about feeding tubes.
- Stomach stimulation may be helpful if your symptoms are severe and other treatments do not work. Surgery is needed to implant a device in your abdomen. The device sends mild signals to the nerves and muscles in your stomach to relieve nausea and vomiting.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage my symptoms?
- Walk after you eat. This may help speed digestion.

- Follow the meal plan that your healthcare or dietitian gave you. This meal plan can help decrease your symptoms. The following may also help you manage your symptoms:
- Eat less fat and fiber. High-fat and high-fiber foods may be hard for your stomach to digest. You may need to avoid fruits and vegetables such as oranges and broccoli.

- Eat 4 to 6 small meals a day. Smaller, more frequent meals are easier for your stomach to handle.
- Drink more liquids with your meals. Your healthcare provider may recommend liquid meals, such as soup. Liquid is easier to digest than solid food.
- Ask if you should prepare your food in a blender. Blended foods are easier to digest. Ask for directions on which foods to use and how to blend the food correctly.
- Ask about vitamins you may need and how to add them to your meals.
- Eat less fat and fiber. High-fat and high-fiber foods may be hard for your stomach to digest. You may need to avoid fruits and vegetables such as oranges and broccoli.
- Do not smoke. Nicotine can damage blood vessels, slow your digestion, and make it more difficult to manage diabetes. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your healthcare provider for information if you currently smoke and need help quitting.
- Do not drink alcohol. Alcohol may slow your digestion more.
- Follow your diabetes treatment plan. You may need to check your blood sugar more often. High blood sugar levels slow digestion and can make your symptoms worse.
When should I seek immediate care?
- You are vomiting more severely or for a longer period than usual.
- You urinate less than usual, and your mouth is dry.
- You feel dizzy and weak, or you have fainted.
- You have severe pain in your stomach or abdomen.
When should I call my doctor or diabetes care team provider?
- Your blood sugar level is higher or lower than healthcare providers have told you it should be.
- You continue to have pain and bloating in your abdomen.
- You continue to have nausea and vomiting, or you are not able to eat.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Diabetic Gastroparesis
- Diabetes Medications and Alcohol Interactions
- FDA-Approved Weight Loss Drugs: Can They Help You?
- OneTouch Blood Glucose Meters
- Side Effects of Weight Loss Drugs
- Top 10 Diabetes Treatments You May Have Missed
- Which Drugs Cause Weight Gain?
Treatment options
- Medications for Diabetes Mellitus
- Medications for Diabetes, Type 1
- Medications for Gastroparesis
- Medications for Type 2 Diabetes
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
