Travasol: Package Insert / Prescribing Info
Package insert / product label
Generic name: leucine, phenylalanine, lysine hydrochloride, methionine, isoleucine, valine, histidine, threonine, tryptophan, alanine, glycine, arginine, proline, tyrosine and serine
Dosage form: injection
Drug class: Intravenous nutritional products
Medically reviewed by Drugs.com. Last updated on Dec 23, 2024.
On This Page
Highlights of Prescribing Information
TRAVASOL (amino acids) injection, for intravenous use
Initial U.S. Approval: 1984
Recent Major Changes
Dosage and Administration, Preparation Instructions for
- Admixing Using a Parenteral Nutrition Container (2.3) 09/2020
Indications and Usage for Travasol
TRAVASOL is indicated as a source of amino acids for patients requiring parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. TRAVASOL may be used to treat negative nitrogen balance in patients. (1)
Travasol Dosage and Administration
- •
- Pharmacy Bulk Package. Not for direct intravenous infusion. (2.1)
- •
- See full prescribing information for information on preparation, administration, instructions for use, dosing considerations, including the recommended dosage in adults and pediatrics, and dosage modifications in patients with renal impairment. (2.1, 2.2, 2.3, 2.4, 2.5, 2.6, 2.7, 2.8)
- •
- Protect the admixed parenteral nutrition solution from light. (2.3)
Dosage Forms and Strengths
Injection: 10% (0.1 grams/mL), 10 grams of amino acid solution per 100 mL in 500 mL, 1000 mL, and 2000 mL flexible containers. (3)
Contraindications
Warnings and Precautions
- •
- Pulmonary Embolism due to Pulmonary Vascular Precipitates: if signs of pulmonary distress occur, stop the infusion and initiate a medical evaluation. (5.1)
- •
- Hypersensitivity Reactions: monitor for signs and symptoms and discontinue infusion if reactions occur. (5.2)
- •
- Risk of Infections, Refeeding Complications, and Hyperglycemia or Hyperosmolar Hyperglycemic State: monitor for signs and symptoms; monitor laboratory parameters. (5.3, 5.4, 5.5)
- •
- Vein Damage and Thrombosis: solutions with osmolarity of 900 mOsm/L or more must be infused through a central catheter. (2.2, 5.6)
- •
- Hepatobiliary Disorders: monitor liver function parameters and ammonia levels. (5.7)
- •
- Aluminum Toxicity: increased risk in patients with renal impairment, including preterm infants. (5.8, 8.4)
- •
- Parenteral Nutrition Associated Liver Disease: increased risk in patients who receive parenteral nutrition for extended periods of time, especially preterm infants; monitor liver function tests, if abnormalities occur consider discontinuation or dosage reduction. (5.9, 8.4)
- •
- Electrolyte Imbalance and Fluid Overload: patients with cardiac insufficiency or renal impairment may require adjustment of fluid, protein and electrolyte content. (5.10, 8.4)
Adverse Reactions/Side Effects
Adverse reactions include pulmonary vascular emboli, hypersensitivity reactions infection, refeeding syndrome, hyperglycemia and hyperosmolar hyperglycemic state, vein thrombosis, elevated liver function tests, hyperammonemia, electrolyte imbalances, and hypervolemia. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Baxter Healthcare Corporation at 1-866-888-2472 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
- Pediatric Use: increased risk of hypoglycemia/hyperglycemia: monitor serum glucose concentrations. (8.4)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 10/2020
Full Prescribing Information
1. Indications and Usage for Travasol
TRAVASOL is indicated as a source of amino acids for patients requiring parenteral nutrition when oral or enteral nutrition is not possible, insufficient, or contraindicated. TRAVASOL may be used to treat negative nitrogen balance in patients.
2. Travasol Dosage and Administration
2.1 Important Preparation Information
TRAVASOL is supplied as a pharmacy bulk package for admixing only and is not for direct intravenous infusion. Prior to administration, TRAVASOL must be transferred to a separate parenteral nutrition container, diluted and used as an admixture with or without dextrose, electrolytes and/or lipid emulsion.
- •
- The key factor in preparation is careful aseptic technique to avoid inadvertent touch contamination during mixing of solutions and addition of other nutrients.
- •
- Do not remove container from overpouch until ready to use.
- •
- Tear protective overpouch across top at slit and remove solution container. Small amounts of moisture may be found on the solution container from water permeating from inside the container. The amount of permeated water is insufficient to affect the solution significantly. If larger amounts of water are found, the container should be checked for tears or leaks.
- •
- Inspect TRAVASOL prior to use. Some opacity of the plastic due to moisture absorption during the sterilization process may be observed. This is normal and does not affect the solution quality or safety. The opacity will diminish gradually.
- Evaluate the following:
- o
- If the outlet port protector is damaged, detached, or not present, discard container as solution path sterility may be impaired.
- o
- Check to ensure the solution is clear, colorless or slightly yellow. Discard if the solution is bright yellow or yellowish brown.
- o
- Check for minute leaks by squeezing inner container. If leaks are found, discard container.
- •
- TRAVASOL is intended for use in the preparation of sterile, intravenous admixtures. Because additives may be incompatible with TRAVASOL, evaluate all additions for compatibility.
2.2 Administration Instructions
- TRAVASOL is for admixing use only. It is not for direct intravenous infusion. Prior to administration, TRAVASOL must be diluted with other compatible intravenous fluids or used as an admixture with or without dextrose, electrolytes and/or lipid emulsion.
- •
- TRAVASOL is to be used only in a suitable work area such as a laminar flow hood (or an equivalent clean air compounding area). The key factor in the preparation is careful aseptic technique to avoid inadvertent touch contamination during mixing of solutions and addition of other nutrients.
- •
- TRAVASOL is for admixing with dextrose injection and/or lipid emulsions using a parenteral nutrition container.
- •
- When TRAVASOL is admixed with dextrose injection and/or lipid emulsion, the choice of a central or peripheral venous route should depend on the osmolarity of the final infusate. Solutions with greater than 5% dextrose or with osmolarity of 900 mOsm/L or greater must be infused through a central venous catheter [see Warnings and Precautions (5.6)].
- •
- Use a dedicated line for parenteral nutrition solutions.
- •
- Intravenous lipid emulsions can be infused concurrently into the same vein as TRAVASOL-dextrose solutions by a Y-connector located near the infusion site; flow rates of each solution should be controlled separately by infusion pumps.
- •
- For administration without lipid emulsion, use a 0.22 micron in-line filter. If lipid emulsion is also administered, use a 1.2 micron in-line filter
- •
- To prevent air embolism, use a non-vented infusion set or close the vent on a vented set, avoid multiple connections, do not connect flexible containers in series, fully evacuate residual gas in the container prior to administration, do not pressurize the flexible container to increase flow rates, and if administration is controlled by a pumping device, turn off pump before the container runs dry.
- •
- If admixed or infused with lipid emulsion, do not use administration sets and lines that contain di-2-ethylhexyl phthalate (DEHP). Administration sets that contain polyvinyl chloride (PVC) components have DEHP as a plasticizer.
- •
- Calcium and phosphate ratios must be considered. Excess addition of calcium and phosphate, especially in the form of mineral salts, may result in the formation of calcium phosphate precipitates [see Warnings and Precautions (5.1)].
- •
- Prior to infusion, visually inspect the diluted parenteral nutrition solution containing TRAVASOL for particulate matter. The solution should be clear and there should be no precipitates. A slight yellow color does not alter the quality and efficacy of this product. If lipid has been added, ensure the emulsion has not separated. Separation of the emulsion can be visibly identified by a yellowish streaking or the accumulation of yellowish droplets in the mixed emulsion. Discard the admixture if any of the above are observed.
2.3 Preparation Instructions for Admixing Using a Parenteral Nutrition Container
- •
- Open by tearing protective overwrap across top at slit and remove solution container. If overpouch has been previously opened or is damaged, discard solution.
- •
- If the outlet port protector is damaged, detached, or not present, discard the container.
- •
- Some opacity of the plastic due to moisture absorption during the sterilization process may be observed.
- •
- Check for minute leaks by squeezing the inner container firmly. If leaks are found, discard solution.
- •
- Once the protective foil overwrap has been removed, suspend container from eyelet support.
- •
- Remove plastic protector from outlet port at bottom of container.
- •
- Attach solution transfer set. Refer to complete directions accompanying set. Note: The closure shall be penetrated only one time with a suitable sterile transfer device or dispensing set which allows measured dispensing of the contents.
- •
- Prepare the admixture into the parenteral nutrition container using strict aseptic techniques to avoid microbial contamination.
- •
- Do not add the lipid emulsion to the parenteral nutrition container first; destabilization of the lipid emulsion may occur from such an admixture.
- •
- TRAVASOL may be mixed with dextrose injection and/or lipid emulsion. The following proper mixing sequence must be followed to minimize pH related problems by ensuring that typically acidic dextrose injections are not mixed with lipid emulsions alone:
- 1.
- Transfer dextrose injection to the parental nutrition pooling container.
- 2.
- Transfer amino acid injection.
- 3.
- Transfer lipid emulsion.
- •
- Because additives may be incompatible, evaluate all additions to the parenteral nutrition container for compatibility and stability of the resulting preparation. Consult with pharmacist, if available. Questions about compatibility may be directed to Baxter. If it is deemed advisable to introduce additives to the parenteral nutrition container, use aseptic technique.
- •
- Use gentle agitation during admixing to minimize localized concentration effects; shake containers gently after each addition.
- •
- Alternatively, simultaneous transfer to the parenteral nutrition container of TRAVASOL, dextrose injection and lipid emulsion is also permitted.
- •
- For admixing using an automated device, refer to Instructions for Use of the applicable device.
- •
- The prime destabilizers of emulsions are excessive acidity (such as pH below 5) and inappropriate electrolyte content. Give careful consideration to additions of divalent cations (Ca++ and Mg++), which have been shown to cause emulsion instability. Amino acid solutions exert buffering effects that protect the emulsion.
- •
- Inspect the final parenteral nutrition solution containing TRAVASOL to ensure that:
- o
- Precipitates have not formed during the mixing or addition of additives.
- o
- The emulsion has not separated. Separation of the emulsion can be visibly identified by a yellowish streaking or the accumulation of yellowish droplets in the admixed emulsion.
- o
- Discard the admixture if any of the above are observed.
- •
- Containers should not be written on directly since ink migration has not been investigated. Affix accompanying label for date and time of entry.
- Stability and Storage
- •
- Use for admixing should be limited to up to 4 hours at room temperature (25ºC/77ºF) after the container closure has been penetrated.
- •
- Admixtures should be used promptly with storage under refrigeration 2° to 8°C (36° to 46°F) not to exceed 24 hours and must be completely used within 24 hours after removal from refrigeration. Any mixture remaining must be discarded.
- •
- Protect the admixed parenteral nutrition solution from light.
- •
- For single use only. Discard used container of TRAVASOL.
2.4 Dosing Considerations
- •
- TRAVASOL is for admixing only. It is not for direct intravenous infusion. Prior to administration, TRAVASOL must be diluted with other compatible intravenous fluids or used as an admixture with or without dextrose, electrolytes and lipid emulsion.
- •
- TRAVASOL is a part of the parenteral nutrition regimen which also includes dextrose, electrolytes, and lipid emulsion. Protein, caloric, fluid and electrolyte requirements all need to be taken into consideration when determining individual patient dosage needs.
- •
- The dosage of the final parenteral nutrition solution containing TRAVASOL must be based on the concentrations of all components in the solution and the recommended nutritional requirements [see Dosage and Administration (2.5, 2.6, 2.7)]. Consult the prescribing information of all added components to determine the recommended nutritional requirements for dextrose and lipid emulsion, as applicable.
- •
- The dosage of TRAVASOL should be individualized based on the patient’s clinical condition (ability to adequately metabolize amino acids), body weight and nutritional/fluid requirements, as well as additional energy given orally/enterally to the patient. Prior to initiating parenteral nutrition, the following patient information should be reviewed: review of all medications, gastrointestinal function and laboratory data (such as electrolytes (including magnesium, calcium, and phosphorus), glucose, urea/creatinine, liver panel, complete blood count and triglyceride level (if adding lipid emulsion)).
- •
- Lipid emulsion administration should be considered with prolonged use (more than 5 days) of parenteral nutrition and is required in order to prevent essential fatty acid deficiency (EFAD). Serum lipids should be monitored for evidence of EFAD in patients maintained on fat-free parenteral nutrition. See complete prescribing information of lipid emulsion.
- •
- Prior to administration of parenteral nutrition solution containing TRAVASOL, correct severe fluid, electrolyte and acid-base disorders.
- •
- In many patients, provision of adequate calories in the form of hypertonic dextrose may require the administration of exogenous insulin to prevent hyperglycemia and glycosuria.
- •
- Monitor levels of serum potassium during parenteral nutrition therapy. It may be necessary to add additional potassium to the parenteral nutrition admixture.
2.5 Recommended Dosage in Adults
- The recommended adult daily dosage of TRAVASOL and the nutritional requirements for protein (nitrogen) are shown in Table 1.
- As a component of parenteral nutrition, TRAVASOL provides 0.1 g protein/mL, which corresponds to 0.0165 g nitrogen/mL.
- As indicated on an individual basis, vitamins, electrolytes, trace elements and other components (including dextrose, electrolytes and lipid emulsion) can be added to the parenteral nutrition solution to meet nutrient needs and prevent deficiencies and complications from developing.
- A maximum fluid supply of 40 mL/kg/day of parenteral nutrition solution, based on protein, should not be exceeded in adult patients; this volume does not take carbohydrates or electrolytes into consideration.
- The flow rate of the parenteral nutrition solution must be adjusted taking into account the dose being administered, the daily volume intake, and the duration of the infusion. The flow rate should be increased gradually and governed, especially during the first few days of therapy, by the patient’s tolerance to dextrose. Daily intake of TRAVASOL and dextrose should be increased gradually to the maximum required dose as indicated by frequent determinations of blood glucose levels.
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
2.6 Dosage Modifications in Patients with Renal Impairment
Prior to administration, correct severe fluid or electrolyte imbalances. Closely monitor serum electrolyte levels and adjust the volume of parenteral nutrition administered as required [see Warnings and Precautions (5.10)].
Patients with renal impairment not needing dialysis require 0.6 to 0.8 g of protein/kg/day. Serum electrolyte levels should be closely monitored. Patients on hemodialysis or continuous renal replacement therapy should receive 1.2 to 1.8 g of protein/kg/day up to a maximum of 2.5 g of protein/kg/day based on nutritional status and estimated protein losses.2
2.7 Recommended Dosage in Pediatric Patients
The dosage and constant infusion rate of intravenous dextrose must be selected with caution in pediatric patients, particularly neonates and low weight infants, because of the increased risk of hyperglycemia/hypoglycemia [see Use in Specific Populations (8.4)]. Frequent monitoring of serum glucose concentrations is required when dextrose is prescribed to pediatric patients, particularly neonates and low birth weight infants. The infusion rate and volume should be determined by the consulting physician experienced in pediatric intravenous fluid therapy.
In pediatric patients, TRAVASOL is dosed on the basis of protein provided as amino acids. The recommended dosage, by age group is provided in .
Infusion rates are based on protein and do not take carbohydrates, fluid or electrolytes into consideration.
TRAVASOL does not contain the amino acids cysteine and taurine, considered conditionally essential for neonates and infants. If possible, these amino acids should be added to the parenteral nutrition admixture if used in this pediatric population.
| Table 2. Recommended Daily Dosage in Pediatric Patients | |||
|---|---|---|---|
| Age | Recommended Proteina Requirement (g/kg/day)1 | Corresponding Nitrogen Requirement (g/kg/day) | Recommended Daily Dosage of TRAVASOL (mL/kg/day) |
|
Preterm and term infants less than 1 month of age |
3 to 4 |
0.48 to 0.64 |
30 to 40 |
|
Pediatric patients 1 month to less than 1 year of age |
2 to 3 |
0.32 to 0.48 |
20 to 30 |
|
Pediatric patients 1 to 10 years of age |
1 to 2 |
0.16 to 0.32 |
10 to 20 |
|
Pediatric patients greater than 10 to less than 17 years of age |
0.8 to 1.5 |
0.13 to 0.24 |
8 to 15 |
|
|||
3. Dosage Forms and Strengths
TRAVASOL 10% is a sterile solution of 10 grams of amino acids per 100 mL (0.1 gram/mL) available in 500 mL, 1000 mL, and 2000 mL flexible containers, which contain essential and nonessential amino acids. describes the individual components of TRAVASOL.
| Table 3. Ingredients per 100 mL of TRAVASOL | |
|---|---|
| Amino Acids | 10 g |
|
Total Nitrogen |
1.65 g |
|
Essential Amino Acids |
|
|
Leucine |
730 mg |
|
Isoleucine |
600 mg |
|
Lysine (added as the hydrochloride salt) |
580 mg |
|
Valine |
580 mg |
|
Phenylalanine |
560 mg |
|
Histidine |
480 mg |
|
Threonine |
420 mg |
|
Methionine |
400 mg |
|
Tryptophan |
180 mg |
|
Nonessential Amino Acids |
|
|
Alanine |
2.07 g |
|
Arginine |
1.15 g |
|
Glycine |
1.03 g |
|
Proline |
680 mg |
|
Serine |
500 mg |
|
Tyrosine |
40 mg |
|
Anion profiles per liter* |
|
|
Acetate† |
88 mEq |
|
Chloride‡ |
40 mEq |
|
pH (Range); pH adjusted with glacial acetic acid |
6.0 (5.0 to 7.0) |
|
Osmolarity (calc) |
998 mOsm/L |
4. Contraindications
The use of TRAVASOL is contraindicated in:
- •
- Patients with known hypersensitivity to one or more amino acids [see Warnings and Precautions (5.2)].
- •
- Patients with inborn errors of amino acid metabolism due to risk of severe metabolic or neurologic complications.
- •
- Patients with pulmonary edema or acidosis due to low cardiac output.
5. Warnings and Precautions
5.1 Pulmonary Embolism due to Pulmonary Vascular Precipitates
Pulmonary vascular precipitates causing pulmonary vascular emboli and pulmonary distress have been reported in patients receiving parenteral nutrition, including TRAVASOL. In some cases, fatal outcomes due to pulmonary embolism have occurred. TRAVASOL contains no added phosphorus. Patients, especially those with hypophosphatemia, may require the addition of phosphate. To prevent hypocalcemia, calcium supplementation should always accompany phosphate administration. Excessive addition of calcium and phosphate increases the risk of the formation of calcium phosphate precipitates. Precipitates have been reported even in the absence of phosphate salt in the solution. Precipitation following passage through an in-line filter and suspected in vivo precipitate formation has also been reported. If signs of pulmonary distress occur, stop the infusion and initiate a medical evaluation. In addition to inspection of the solution [see Dosage and Administration (2.1, 2.2, 2.3, 2.4)], the infusion set and catheter should also periodically be checked for precipitates.
5.2 Hypersensitivity Reactions
Hypersensitivity reactions including anaphylaxis have been reported with parenteral nutrition solutions containing TRAVASOL. Stop the infusion immediately and treat patient accordingly if any signs or symptoms of a hypersensitivity reaction develop. Signs or symptoms may include: hypotension, hypertension, peripheral cyanosis, tachycardia, dyspnea, vomiting, nausea, urticaria, rash, pruritus, erythema, hyperhidrosis, pyrexia, and chills.
5.3 Risk of Infections
Patients who require parenteral nutrition are at high risk of infections because the nutritional components of these solutions can support microbial growth. Infection and sepsis may also occur as a result of the use of intravenous catheters to administer parenteral nutrition.
The risk of infection is increased in patients with malnutrition-associated immunosuppression, hyperglycemia exacerbated by dextrose infusion, long-term use and poor maintenance of intravenous catheters, or immunosuppressive effects of other concomitant conditions, drugs, or other components of the parenteral formulation (e.g., lipid emulsion).
To decrease the risk of infection, ensure aseptic technique in catheter placement and maintenance, as well as aseptic technique in the preparation and administration of the nutritional formula.
Monitor for signs and symptoms (including fever and chills) of early infections, including laboratory test results (including leukocytosis and hyperglycemia) and frequent checks of the parenteral access device and insertion site for edema, redness and discharge.
5.4 Refeeding Syndrome
Refeeding severely undernourished patients may result in refeeding syndrome, characterized by the intracellular shift of potassium, phosphorus, and magnesium as the patient becomes anabolic. Thiamine deficiency and fluid retention may also develop. To prevent these complications, monitor severely undernourished patients and slowly increase nutrient intakes.
5.5 Hyperglycemia or Hyperosmolar Hyperglycemic State
Administration of parenteral nutrition solutions containing dextrose in patients with diabetes mellitus, impaired glucose tolerance may worsen hyperglycemia. Administration of dextrose at a rate exceeding the patient’s utilization rate may lead to hyperglycemia, coma, and death. Patients with underlying confusion and renal impairment who receive dextrose infusions, may be at greater risk of developing hyperosmolar hyperglycemic state. Monitor blood glucose levels and treat hyperglycemia to maintain optimum levels while administering parenteral nutrition solutions containing dextrose. Insulin may be administered or adjusted to maintain optimal blood glucose levels during administration of parenteral nutrition solutions containing dextrose.
5.6 Vein Damage and Thrombosis
TRAVASOL must be diluted and used as an admixture with or without dextrose, electrolytes and/or lipid emulsion. It is not for direct intravenous infusion. Solutions containing more than 5% dextrose or with an osmolarity of 900 mOsm/L or greater must be infused through a central catheter [see Dosage and Administration (2.2)]. The infusion of hypertonic nutrient injections into a peripheral vein may result in vein irritation, vein damage, and/or thrombosis. The primary complication of peripheral access is venous thrombophlebitis, which manifests as pain, erythema, tenderness or a palpable cord. Remove the catheter as soon as possible, if thrombophlebitis develops.
5.7 Hepatobiliary Disorders
Hepatobiliary disorders are known to develop in some patients without preexisting liver disease who receive parenteral nutrition, including cholecystitis, cholelithiasis, cholestasis, hepatic steatosis, fibrosis and cirrhosis, possibly leading to hepatic failure. The etiology of these disorders is thought to be multifactorial and may differ between patients.
Increase in blood ammonia levels and hyperammonemia may occur in patients receiving amino acid solutions, including TRAVASOL. In some patients this may indicate hepatic insufficiency or the presence of an inborn error of amino acid metabolism [see Contraindications (4) and Use in Specific Populations (8.4)].
Monitor liver function parameters and ammonia levels. Patients developing signs of hepatobiliary disorders should be assessed early by a clinician knowledgeable in liver diseases in order to identify possible causative and contributory factors, and possible therapeutic and prophylactic interventions.
5.8 Aluminum Toxicity
TRAVASOL contains no more than 25 mcg/L of aluminum. However, with prolonged parenteral administration in patients with renal impairment, the aluminum contained in TRAVASOL may reach toxic levels. Preterm infants are at a greater risk because their kidneys are immature, and they require large amounts of calcium and phosphate solutions, which contain aluminum.
Patients with renal impairment, including preterm infants, who receive parenteral levels of aluminum at greater than 4 to 5 mcg/kg/day, accumulate aluminum at levels associated with central nervous system and bone toxicity. Tissue loading may occur at even lower rates of administration.
5.9 Risk of Parenteral Nutrition Associated Liver Disease
Parenteral Nutrition Associated Liver Disease (PNALD) has been reported in patients who receive parenteral nutrition for extended periods of time, especially preterm infants, and can present as cholestasis or steatohepatitis. The exact etiology is unknown and is likely multifactorial. If patients treated with parenteral nutrition solutions containing TRAVASOL develop liver test abnormalities, consider discontinuation or dosage reduction.
5.10 Electrolyte Imbalance and Fluid Overload
Patients with renal impairment, such as pre-renal azotemia, renal obstruction, and protein-losing nephropathy may be at increased risk of electrolyte and fluid volume imbalance. Patients with cardiac insufficiency and pulmonary congestion are susceptible to excess fluid accumulation. Use parenteral nutrition solutions containing TRAVASOL with caution in patients with cardiac insufficiency or renal impairment. The dosage of parenteral nutrition may require adjustment with specific attention to fluid, protein, and electrolyte content in these patients.
Monitor renal function parameters. Patients developing signs of renal impairment should be assessed early by a clinician knowledgeable in renal disease in order to determine the appropriate parenteral nutrition dosage and other treatment options.
5.11 Monitoring/Laboratory Tests
Monitor fluid and electrolyte status, serum osmolarity, blood glucose, liver and kidney function, blood count and coagulation parameters throughout treatment. If electrolyte levels are severely elevated, stop parenteral nutrition containing TRAVASOL until levels have been corrected.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed in greater detail in other sections of the prescribing information.
- •
- Pulmonary embolism due to pulmonary vascular precipitates [see Warnings and Precautions (5.1)]
- •
- Hypersensitivity reactions [see Warnings and Precautions (5.2)]
- •
- Risk of Infections [see Warnings and Precautions (5.3)]
- •
- Refeeding syndrome [see Warnings and Precautions (5.4)]
- •
- Hyperglycemia or hyperosmolar hyperglycemic state [see Warnings and Precautions (5.5)]
- •
- Vein damage and thrombosis [see Warnings and Precautions (5.6)]
- •
- Hepatobiliary disorders [see Warnings and Precautions (5.7)]
- •
- Aluminum toxicity [see Warnings and Precautions (5.8)]
- •
- Parenteral Nutrition Associated Liver Disease [see Warnings and Precautions (5.9)]
- •
- Electrolyte imbalance and fluid overload [see Warnings and Precautions (5.10)]
The following adverse reactions from voluntary reports or clinical studies have been reported with TRAVASOL. Because many of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- •
- Metabolic acidosis
- •
- Alkalosis
- •
- Osmotic diuresis and dehydration,
- •
- Rebound hypoglycemia
- •
- Hypo- and hyper-vitaminosis
Related/similar drugs
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Limited published data with injectable amino acids solutions, including TRAVASOL in pregnant women are not sufficient to inform a drug associated risk for adverse developmental outcomes. However, malnutrition in pregnant women is associated with adverse maternal and fetal outcomes [see Clinical Considerations]. Animal reproduction studies have not been conducted with injectable amino acids solutions, including TRAVASOL.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. However, the background risk in the U.S. general population of major birth defects is 2 to 4% and of miscarriage is 15 to 20% of clinically recognized pregnancies.
Clinical Considerations
Disease-Associated Maternal and/or Embryo-Fetal Risk
Severe malnutrition in pregnant women is associated with preterm delivery, low birth weight, intrauterine growth restriction, congenital malformations and perinatal mortality. Parenteral nutrition should be considered if a pregnant woman’s nutritional requirements cannot be fulfilled by oral or enteral intake.
8.2 Lactation
Risk Summary
There are no data available to assess the presence of injectable amino acids, including TRAVASOL in human milk, the effects of TRAVASOL on the breastfed infant or the effects on milk production. The lack of clinical data during lactation precludes a clear determination of the risk of TRAVASOL to a child during lactation; therefore, the developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for TRAVASOL and any potential adverse effects on the breastfed child from TRAVASOL or from the underlying maternal condition.
8.4 Pediatric Use
Neonates, especially premature infants with low birth weight, are at increased risk of developing hypo- or hyperglycemia and therefore need close monitoring during treatment with intravenous glucose solutions to ensure adequate glycemic control in order to avoid potential long term adverse effects [see Dosage and Administration (2.7)].
Plasma electrolyte concentrations should be closely monitored in the pediatric patients who may have impaired ability to regulate fluids and electrolytes.
Hyperammonemia is of special significance in infants (birth to two years). This reaction appears to be related to a deficiency of the urea cycle amino acids of genetic or product origin. It is essential that blood ammonia be measured frequently in infants [see Warnings and Precautions (5.7)].
Because of immature renal function, preterm infants receiving prolonged parenteral nutrition treatment with TRAVASOL may be at risk of aluminum toxicity [see Warnings and Precautions (5.8)].
Patients, including pediatric patients, may be at risk for PNALD [see Warnings and Precautions (5.9)].
8.5 Geriatric Use
Clinical studies with TRAVASOL have not been performed to determine whether subjects aged 65 and over respond differently from other younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or drug therapy.
8.6 Renal Impairment
In patients with impaired renal function, parenteral nutrition solutions containing TRAVASOL should be administered with caution. Frequent clinical evaluation and laboratory tests to monitor renal function such as serum electrolytes (especially phosphate and potassium) and fluid balance should be conducted [see Dosage and Administration (2.6), Warnings and Precautions (5.10)].
8.7 Hepatic Impairment
In patients with impaired liver function, parenteral nutrition solutions containing TRAVASOL should be administered starting at the low end of the dosing range [see Dosage and Administration (2.5)]. Frequent clinical evaluation and laboratory tests to monitor liver function such as bilirubin and liver function parameters should be conducted [see Warnings and Precautions (5.7)].
10. Overdosage
An increased infusion rate of parenteral nutrition can cause hypervolemia, electrolyte disturbances, acidosis and/or azotemia, hyperglycemia, hyperosmolality [see Warnings and Precautions (5.5, 5.10)].
Severe hyperglycemia and severe dilutional hyponatremia, and their complications, can be fatal.
Discontinue infusion and institute appropriate corrective measures in the event of overhydration or solute overload during therapy, with particular attention to respiratory and cardiovascular systems.
For current information on the management of poisoning or overdosage, contact the National Poison Control Center at 1-800-222-1222 or www.poison.org.
11. Travasol Description
TRAVASOL 10% (amino acids) injection is a sterile, nonpyrogenic hypertonic solution of essential and nonessential amino acids supplied in a flexible container as a Pharmacy Bulk Package. A Pharmacy Bulk Package is a container of a sterile preparation for parenteral use that contains many single doses. The contents are intended for use in a pharmacy admixture program [see Dosage and Administration (2.1)]. TRAVASOL is not for direct intravenous infusion.
The formulas for the individual amino acids found in TRAVASOL are provided in .
| Table 4. Formulas for Amino Acids | |
|---|---|
|
Essential Amino Acids |
|
|
Leucine |
(CH3)2 CHCH2CH (NH2) COOH |
|
Isoleucine |
CH3CH2CH (CH3) CH (NH2) COOH |
|
Lysine (added as the hydrochloride salt) |
H2N (CH2)4 CH (NH2) COOH |
|
Valine |
(CH3)2 CHCH (NH2) COOH |
|
Phenylalanine |
(C6H5) CH2 CH (NH2) COOH |
|
Histidine |
(C3H3N2) CH2CH (NH2) COOH |
|
Threonine |
CH3CH (OH) CH (NH2) COO |
|
Methionine |
CH3S (CH2)2 CH (NH2) COOH |
|
Tryptophan |
(C8H6N) CH2 CH (NH2) COOH |
|
Nonessential Amino Acids |
|
|
Alanine |
CH3CH (NH2) COOH |
|
Arginine |
H2NC (NH) NH (CH2)3 CH (NH2) COOH |
|
Glycine |
H2NCH2COOH |
|
Proline |
[(CH2)3 NH CH] COOH |
|
Serine |
HOCH2CH (NH2) COOH |
|
Tyrosine |
[C6H4 (OH)] CH2CH (NH2) COOH |
TRAVASOL contains no more than 25 mcg/L of aluminum.
12. Travasol - Clinical Pharmacology
12.1 Mechanism of Action
TRAVASOL is used as a supplement of nutrition in patients, providing amino acids parenterally.
The amino acids provide the structural units that make up proteins and are used to synthesize proteins and other biomolecules or are oxidized to urea and carbon dioxide as a source of energy.
15. References
- 1.
- Ayers P. et al. A.S.P.E.N. Parenteral Nutrition Handbook, 2nd ed. 2014 pg. 123
- 2.
- Mueller CM ed. The A.S.P.E.N. Nutrition Support Core Curriculum 2nd ed. 2012. Chapter 29 Wolk R, Foulks C. Renal Disease., pg. 500
16. How is Travasol supplied
TRAVASOL 10% (amino acids) injection is available in plastic Pharmacy Bulk Package flexible containers in the following sizes as shown in Table 5 below.
|
Code |
|
NDC Number |
|
1B6623 |
|
NDC 0338-0644-03 |
|
1B6624 |
1000 mL |
NDC 0338-0644-04 |
|
1B6626P |
2000 mL |
NDC 0338-0644-06 |
Minimize exposure of TRAVASOL to heat and avoid excessive heat.
Protect from freezing.
Store TRAVASOL at room temperature (25ºC/77ºF).
Do not use if protective overpouch has been previously opened or damaged.
For storage of admixed solutions [see Dosage and Administration (2.3)].
17. Patient Counseling Information
Inform patients, caregivers, or home healthcare providers of the following risks of TRAVASOL:
- •
- Pulmonary embolism due to pulmonary vascular precipitates [see Warnings and Precautions (5.1)]
- •
- Hypersensitivity reactions [see Warnings and Precautions (5.2)]
- •
- Risk of Infections [see Warnings and Precautions (5.3)]
- •
- Refeeding syndrome [see Warnings and Precautions (5.4)]
- •
- Hyperglycemia or hyperosmolar hyperglycemic state [see Warnings and Precautions (5.5)]
- •
- Vein damage and thrombosis [see Warnings and Precautions (5.6)]
- •
- Hepatobiliary disorders [see Warnings and Precautions (5.7)]
- •
- Aluminum toxicity [see Warnings and Precautions (5.8)]
- •
- Parenteral Nutrition Associated Liver Disease (PNALD) [see Warnings and Precautions (5.9)]
- •
- Electrolyte imbalance and fluid overload [see Warnings and Precautions (5.10)]
Baxter Healthcare Corporation
Deerfield, IL 60015 USA
Baxter and Travasol are registered trademarks of Baxter International Inc.
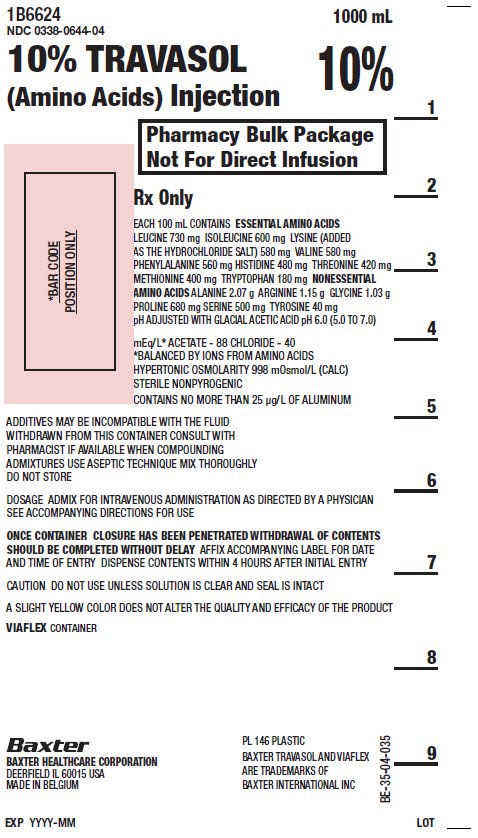
PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
Container Label
1B6624 1000 mL
NDC 0338-0644-04
10% TRAVASOL
10%
(Amino Acid)
Injection
Pharmacy Bulk Package
Not For Direct Infusion
Rx Only
EACH 100mL CONTAINS ESSENTIAL AMINO ACIDS LEUCINE 730 mg
ISOLEUCINE 600 mg LYSINE(ADDED AS THE HYDROCHLORIDE SALT) 580 mg VALINE 580 mg PHENYLALANINE 560 mg HISTIDINE 480 mg
THREONINE 420 mg METHIONINE 400 mg TRYPTOPHAN 180 mg
NONESSENTIALAMINO ACIDS ALANINE 2.07 g ARGININE 1.15 g
GLYCINE 1.03 g PROLINE 680 mg SERINE 500 mg TYROSINE 40 mg
pH ADJUSTED WITH GLACIAL ACETIC ACID pH 6.0 (5.0 TO 7.0)
mEq/L* ACETATE - 88 CHLORIDE - 40
*BALANCED BY IONS FROM AMINO ACIDS
HYPERTONIC OSMOLARITY 998 mOsmo/L (CALC)
STERILE NONPYROGENIC
CONTAINS NO MORE THAN 25 µg/L OF ALUMINUM
ADDITIVES MAY BE INCOMPATIBLE WITH THE FLUID WITHDRAWN
FROM THIS CONTAINER CONSULT WITH PHARMACIST IF AVAILABLE
WHEN COMPOUNDING ADMIXTURES USE ASEPTIC TECHNIQUE
MIX THOROUGHLY DO NOT STORE
DOSAGE ADMIX FOR INTRAVENOUS ADMINISTRATION AS DIRECTED
BY A PHYSICIAN SEE ACCOMPANYING DIRECTIONS FOR USE
ONCE CONTAINER CLOSURE HAS BEEN PENETRATED
WITHDRAWAL OF CONTENTS SHOULDBE COMPLETED
WITHOUT DELAY AFFIX ACCOMPANYING LABEL FOR DATE
AND TIME OF ENTRY DISPENSE CONTENTS WITHIN 4 HOURS
AFTER INITIAL ENTRY
CAUTION DO NOT USE UNLESS SOLUTION IS CLEAR AND
SEAL IS INTACT
A SLIGHT YELLOW COLOR DOES NOT ALTER THE QUALITY AND
EFFICACY OF THE PRODUCT
VIAFLEX CONTAINER
Baxter Logo
BAXTER HEALTHCARE CORPORATION
DEERFIELD IL 60015 USA
MADE IN BELGIUM
PL 146 PLASTIC
BAXTER TRAVASOL AND VIAFLEX
ARE TRADEMARKS OF
BAXTER INTERNATIONAL INC
EXP YYYY-MM
BE-35-04-035
1 2 3 4 5 6 7 8 9
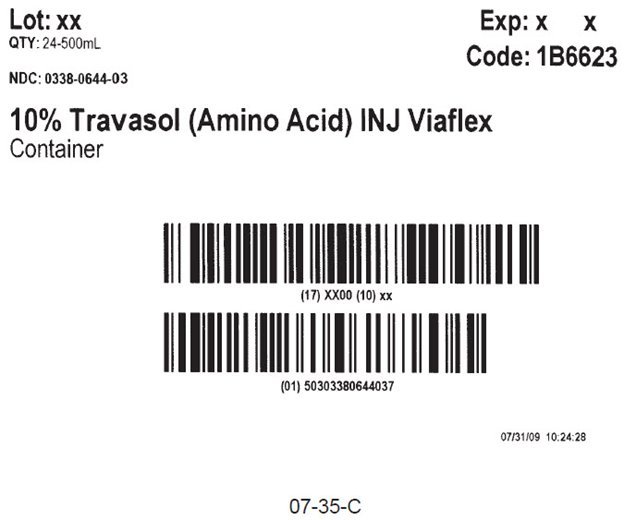
Carton Label
Lot: xx
Qty: 24-500mL
Exp: x x
Code: 1B6623
NDC: 0338-0644-03
10% Travasol (Amino Acid) INJ Viaflex
Container
(17) XX00 (10) xx
(01) 50303380644037
07/31/09 10:24:28
07-35-C
| TRAVASOL
leucine, phenylalanine, lysine hydrochloride, methionine, isoleucine, valine, histidine, threonine, tryptophan, alanine, glycine, arginine, proline, tyrosine, serine injection |
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||
| Labeler - Baxter Healthcare Corporation (005083209) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Baxter Healthcare Corporation | 189326168 | ANALYSIS(0338-0644) , MANUFACTURE(0338-0644) , LABEL(0338-0644) , PACK(0338-0644) , STERILIZE(0338-0644) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Baxter Healthcare Corporation | 194684502 | ANALYSIS(0338-0644) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Baxter SA | 370353835 | ANALYSIS(0338-0644) , MANUFACTURE(0338-0644) , LABEL(0338-0644) , PACK(0338-0644) , STERILIZE(0338-0644) | |
More about parenteral nutrition solution
- Check interactions
- Compare alternatives
- Pricing & coupons
- Latest FDA alerts (2)
- Side effects
- Drug class: intravenous nutritional products
Patient resources
Professional resources
Other brands
Hepatamine, Novamine, FreAmine HBC, Plenamine, ... +5 more