Chlordiazepoxide (Monograph)
Brand name: formerly available as Librium
Drug class: Benzodiazepines
VA class: CN302
CAS number: 58-25-3
chlordiazePOXIDE (Systemic) is also contained as an ingredient in the following combinations:
chlordiazePOXIDE and Amitriptyline Hydrochloride
chlordiazePOXIDE Hydrochloride and Clidinium Bromide
Warning
- Concomitant Use with Opiates
-
Concomitant use of benzodiazepines and opiates may result in profound sedation, respiratory depression, coma, and death.
-
Reserve concomitant use for patients in whom alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy and monitor closely for respiratory depression and sedation. (See Specific Drugs and Laboratory Tests under Interactions.)
- Potential for Abuse, Addiction, and Other Serious Risks
-
A boxed warning has been included in the prescribing information for all benzodiazepines describing risks of abuse, misuse, addiction, physical dependence, and withdrawal reactions.
-
Abuse and misuse can result in overdose or death, especially when benzodiazepines are combined with other medicines, such as opioid pain relievers, alcohol, or illicit drugs.
-
Assess a patient’s risk of abuse, misuse, and addiction. Standardized screening tools are available ([Web]).
-
To reduce risk of acute withdrawal reactions, use a gradual dose taper when reducing dosage or discontinuing benzodiazepines. Take precautions when benzodiazepines are used in combination with opioid medications.
Introduction
Benzodiazepine. Anxiolytic, sedative.
Uses for Chlordiazepoxide
Alcohol Withdrawal
Relief of agitation and tremor and prevention or symptomatic relief of delirium tremens and hallucinations associated with acute alcohol withdrawal.
Anxiety and Depressive Disorders
Management of anxiety disorders and short-term relief of symptoms of anxiety.
Management of moderate to severe anxiety (in fixed-combination with amitriptyline hydrochloride) in patients with moderate to severe depression.
Preoperative Anxiolysis
Preoperatively to relieve anxiety.
Peptic Ulcer Disease, Irritable Bowel Syndrome, and Acute Enterocolitis
Has been used in fixed combination with clidinium bromide as an adjunct in the treatment of peptic ulcer disease, functional disturbances of GI motility (e.g., irritable bowel syndrome), and acute enterocolitis. Fixed combination is classified by FDA as possibly effective for these indications.
Has limited usefulness in the treatment of peptic ulcer disease because of the advent of more effective therapies for this condition.
Therapeutic benefits achieved with the combination preparation in the management of functional disturbances of GI motility may be attributed to the anxiolytic and/or sedative properties of chlordiazepoxide.
Although the fixed combination has been used in the treatment of acute enterocolitis, antimuscarinic-containing preparations should be used with extreme caution in patients with diarrhea or ulcerative colitis.
Related/similar drugs
duloxetine, escitalopram, hydroxyzine, Lexapro, Xanax, diazepam, Cymbalta
Chlordiazepoxide Dosage and Administration
General
-
Use the smallest effective dosage (especially in geriatric and debilitated patients and in those with liver disease or low serum albumin) to avoid oversedation.
-
Consider the long half-life of chlordiazepoxide and its metabolites when making dosage adjustments. (See Half-life under Pharmacokinetics.)
-
In patients who have received prolonged (e.g., several months) therapy, avoid abrupt discontinuance, since manifestations of withdrawal can be precipitated; gradually taper dosage.
-
Fixed-ratio combination preparations generally should not be used as initial therapy. Administer each drug separately. If the optimum maintenance dosage corresponds to the ratio in a commercial combination preparation, a fixed-combination preparation may be used. If dosage adjustment is necessary, administer the drugs separately. Although chlordiazepoxide hydrochloride is commercially available as single-entity preparations, clidinium bromide is commercially available in the US only in fixed combination with chlordiazepoxide hydrochloride. Fixed-ratio combination preparations do not permit individual titration of dosages.
Anxiety
-
Periodically reassess the usefulness of the drug. Efficacy of chlordiazepoxide beyond 4 months not systematically evaluated. Administer for the shortest possible period of time; frequent dosage adjustments may be required.
Administration
Administer orally.
Has been administered parenterally† [off-label]; however, a parenteral dosage form is no longer commercially available in the US.
Oral Administration
Initially, administer orally in 3 or 4 doses daily. After dosage has been stabilized, may reduce frequency to 1 or 2 doses daily.
Dosage
Available as chlordiazepoxide hydrochloride (alone and in fixed combination with clidinium bromide); dosage expressed in terms of the salt.
Also available as chlordiazepoxide (in fixed combination with amitriptyline hydrochloride); dosage expressed in terms of the base.
On the basis of molecular weight, 89 mg of chlordiazepoxide is equivalent to 100 mg of chlordiazepoxide hydrochloride; however, the manufacturer of chlordiazepoxide base (no longer commercially available in the US as a single-entity preparation) states that chlordiazepoxide and its hydrochloride salt may be used interchangeably on a mg-for-mg basis.
Pediatric Patients
Anxiety Disorders
Oral
Children ≥6 years of age: Usual dosage is 5 mg 2–4 times daily. Initial dosage should not exceed 10 mg daily. If necessary, increase dosage to 10 mg 2 or 3 times daily.
Alternatively, some clinicians have recommended a pediatric dosage of 0.5 mg/kg daily or 15 mg/m2 daily in 3 or 4 divided doses.
Adults
Alcohol Withdrawal
Oral
Initially, 50- to 100-mg dose; repeat dose until agitation is controlled.
Manufacturer states that dosage for acute alcohol withdrawal should not exceed 300 mg daily; however, some clinicians have used dosages of 600–800 mg daily to control symptoms without adverse effects.
Slowly withdraw the drug after agitation is controlled.
Anxiety and Depressive Disorders
Monotherapy
OralMild to moderate anxiety: 5–10 mg 3 or 4 times daily.
Severe anxiety: 20–25 mg 3 or 4 times daily.
Chlordiazepoxide/Amitriptyline Combination Therapy
OralInitially, chlordiazepoxide 30 or 40 mg daily (in fixed combination with amitriptyline hydrochloride 75 or 100 mg daily, respectively) in divided doses. If needed, increase dosage to chlordiazepoxide 60 mg daily (in fixed combination with amitriptyline hydrochloride 150 mg daily) in divided doses.
Alternatively, in patients who do not tolerate larger dosages, initial dosage of chlordiazepoxide 15 or 20 mg daily (in fixed combination with amitriptyline hydrochloride 37.5 or 50 mg daily, respectively) in divided doses.
For some patients, chlordiazepoxide 20 mg daily (in fixed combination with amitriptyline hydrochloride 50 mg daily) in divided doses may be adequate.
Preoperative Anxiolysis
Oral
5–10 mg 3 or 4 times daily for several days preceding surgery.
Peptic Ulcer Disease, Irritable Bowel Syndrome, and Acute Enterocolitis
Oral
Usual maintenance dosage is 5 or 10 mg (in fixed combination with clidinium bromide 2.5 or 5 mg, respectively) 3 or 4 times daily (before meals and at bedtime).
Prescribing Limits
Pediatric Patients
Anxiety Disorders
Oral
Children ≥6 years of age: Maximum initial dosage of 10 mg daily.
Adults
Alcohol Withdrawal
Oral
Maximum 300 mg daily recommended by manufacturer. Some clinicians have used higher dosages (600–800 mg daily) to control symptoms without adverse effects.
Special Populations
Hepatic Impairment
Reduce dosage; use the smallest effective dosage.
Renal Impairment
No specific dosage recommendations.
Geriatric or Debilitated Patients
Reduce initial dosage. Use the smallest effective dosage to avoid oversedation.
Anxiety and Depressive Disorders
5 mg 2–4 times daily; initial dosage should not exceed 10 mg daily.
When used in fixed combination with amitriptyline hydrochloride, select initial dosages at the lower end of the usual ranges and gradually increase dosages if needed and tolerated.
Peptic Ulcer Disease, Irritable Bowel Syndrome, and Acute Enterocolitis
Initially, 10 mg daily (given in fixed combination with clidinium bromide 5 mg daily); gradually increase dosages if needed and tolerated.
Cautions for Chlordiazepoxide
Contraindications
-
Known hypersensitivity to chlordiazepoxide, other benzodiazepines, or any ingredient in the formulation.
-
Many manufacturers state that benzodiazepines are contraindicated in patients with acute angle-closure glaucoma but may be administered to patients with open-angle glaucoma who are receiving appropriate therapy; however, clinical rationale for this contraindication has been questioned.
Warnings/Precautions
Warnings
Concomitant Use with Opiates
Concomitant use of benzodiazepines, including chlordiazepoxide, and opiates may result in profound sedation, respiratory depression, coma, and death. Substantial proportion of fatal opiate overdoses involve concurrent benzodiazepine use.
Reserve concomitant use of chlordiazepoxide and opiates for patients in whom alternative treatment options are inadequate. (See Specific Drugs and Laboratory Tests under Interactions.)
CNS Effects
Performance of activities requiring mental alertness and physical coordination may be impaired.
Concurrent use of other CNS depressants may cause additive or potentiated CNS depression. (See Concomitant Use with Opiates under Cautions and also see Specific Drugs and Laboratory Tests under Interactions.)
Paradoxical reactions (e.g., excitement, stimulation, acute rage) reported in psychiatric patients and in hyperactive aggressive children.
Fetal/Neonatal Morbidity
Some retrospective studies suggest increased risk of congenital malformations in infants of mothers who received chlordiazepoxide during the first trimester of pregnancy. Since use of anxiolytics is rarely urgent, their use during the first trimester almost always should be avoided.
Psychiatric Indications
Benzodiazepines should not be used in patients with depressive neuroses or psychotic reactions in which anxiety is not prominent.
Abuse Potential
Possible tolerance, psychologic dependence, and physical dependence following prolonged use.
Patients with a history of drug or alcohol dependence or abuse are at risk of habituation or dependence; use only with careful surveillance in such patients.
Withdrawal Syndrome
Abrupt discontinuance may result in symptoms of withdrawal (similar to barbiturates). Symptoms may be relieved by tapering the dosage.
General Precautions
Suicide
Use with caution in depressed patients; potential for suicidal tendencies. Prescribe and dispense drug in the smallest feasible quantity.
Use of Fixed Combinations
When used in fixed combination with clidinium bromide or amitriptyline hydrochloride, consider the cautions, precautions, and contraindications associated with the concomitant agent.
Porphyria
Exacerbation of porphyria reported; use with caution in patients with this disease.
Laboratory Testing
Monitor blood counts and liver function tests periodically during prolonged therapy. Blood dyscrasias (including agranulocytosis), jaundice, and hepatic dysfunction reported occasionally.
Specific Populations
Pregnancy
Category D. (See Fetal/Neonatal Morbidity under Cautions.)
Lactation
Many benzodiazepines are distributed into milk; distribution of chlordiazepoxide into milk should be expected. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy of chlordiazepoxide hydrochloride not established in children <6 years of age.
Safety and efficacy of the chlordiazepoxide hydrochloride-clidinium bromide and the chlordiazepoxide-amitriptyline hydrochloride fixed combinations not established in pediatric patients.
Response of children to CNS drugs may be unpredictable; initiate therapy at low dosage and increase as required. (See Dosage under Dosage and Administration.)
Monitor hyperactive, aggressive children for paradoxical reactions (e.g., excitement, stimulation, acute rage).
Geriatric Use
Prolonged elimination of chlordiazepoxide and its metabolites.
Possible increased risk of drowsiness, ataxia, and confusion; generally preventable by proper dosage adjustment, but occasionally may be observed at reduced dosages.
No overall differences in safety and efficacy of chlordiazepoxide in fixed combination with amitriptyline hydrochloride in geriatric patients relative to younger adults; however, increased sensitivity cannot be ruled out.
Initiate therapy at low dosages; gradually increase dosage if needed and tolerated. (See Geriatric or Debilitated Patients under Dosage and Administration.)
Hepatic Impairment
Prolonged elimination of chlordiazepoxide and its metabolites. Use with caution. Use smallest effective dosage.
Renal Impairment
Use with caution.
Common Adverse Effects
Drowsiness, ataxia, confusion.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum- and magnesium-containing) |
Possible decrease in rate, but not extent, of chlordiazepoxide absorption |
|
|
Anticoagulants, oral |
Manufacturers state that variable effects on coagulation have been reported; however, several studies found no clinically important effect on hypoprothrombinemia |
|
|
Cimetidine |
Possible decreased clearance and increased plasma concentrations of chlordiazepoxide |
Use with caution; consider reduction of chlordiazepoxide dosage |
|
CNS depressants (e.g., alcohol, anticonvulsants, psychotropic drugs, sedatives) |
Additive CNS effect |
Use caution to avoid overdosage Concomitant use of chlordiazepoxide with other psychotropic agents generally is not recommended Avoid alcohol use |
|
Disulfiram |
Reduced plasma clearance and increased plasma half-life of chlordiazepoxide |
Reduce chlordiazepoxide dosage as necessary |
|
Levodopa |
Possible decreased control of parkinsonian symptoms |
Use with caution |
|
Opiate agonists and partial agonists |
Risk of profound sedation, respiratory depression, coma, or death |
Whenever possible, avoid concomitant use Opiate analgesics: Use concomitantly only if alternative treatment options are inadequate; use lowest effective dosages and shortest possible duration of concomitant therapy; monitor closely for respiratory depression and sedation In patients receiving chlordiazepoxide, initiate opiate analgesic, if required, at reduced dosage and titrate based on clinical response In patients receiving an opiate analgesic, initiate chlordiazepoxide, if required, at lower dosage than indicated in the absence of opiate therapy and titrate based on clinical response Opiate antitussives: Avoid concomitant use Consider offering naloxone to patients receiving benzodiazepines and opiates concomitantly |
|
Test for pregnancy (Gravindex test) |
Possible false-positive reaction |
|
|
Tests for urinary alkaloids |
Possible interference with Frings thin layer chromatography procedure, resulting in falsely elevated readings |
|
|
Tests for urinary 17-ketosteroids |
Possible interference with Zimmerman reaction, resulting in falsely elevated or decreased concentrations |
Chlordiazepoxide Pharmacokinetics
Absorption
Bioavailability
Benzodiazepines are well absorbed from the GI tract after oral administration.
Distribution
Extent
Benzodiazepines are widely distributed into body tissues and cross the blood-brain barrier.
Many benzodiazepines are distributed into milk; distribution of chlordiazepoxide into milk should be expected.
Chlordiazepoxide crosses the placenta.
Plasma Protein Binding
Benzodiazepines are highly bound to plasma proteins.
Elimination
Metabolism
Metabolized in the liver. Major active metabolites include demoxepam, desmethylchlordiazepoxide, desmethyldiazepam, and oxazepam. Hydroxylated metabolites of chlordiazepoxide are conjugated with glucuronic acid.
Elimination Route
Inactive conjugates are excreted principally in urine.
Half-life
Chlordiazepoxide: 5–30 hours.
Metabolites: Demoxepam: 14–95 hours. Desmethylchlordiazepoxide: 18 hours. Desmethyldiazepam: 30–200 hours. Oxazepam: 3–21 hours.
Special Populations
In geriatric patients and patients with liver disease, half-lives of chlordiazepoxide and its metabolites are prolonged.
Benzodiazepines are not appreciably removed by hemodialysis.
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C).
Fixed-combination (with Amitriptyline Hydrochloride) Tablets
Store in a dry place at 25°C (may be exposed to 15–30°C).
Fixed-combination (with Clidinium Bromide) Capsules
25°C (may be exposed to 15–30°C).
Actions
-
Effects appear to be mediated through the inhibitory neurotransmitter GABA; the site and mechanism of action within the CNS appear to involve a macromolecular complex (GABAA-receptor-chloride ionophore complex) that includes GABAA receptors, high-affinity benzodiazepine receptors, and chloride channels.
Advice to Patients
-
Risk of potentially fatal additive effects (e.g., profound sedation, respiratory depression, coma) if used concomitantly with opiates either therapeutically or illicitly. Avoid concomitant use of opiate antitussives; also avoid concomitant use of opiate analgesics unless use is supervised by clinician.
-
Potential for drug to impair mental alertness or physical coordination; avoid driving or operating machinery until effects on individual are known.
-
Importance of informing clinicians of any behavioral or mental changes, memory impairment, tolerance, or dependence/withdrawal symptoms.
-
Importance of taking only as prescribed; do not increase dosage or duration of therapy or abruptly discontinue drug unless otherwise instructed by a clinician.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs. Importance of not consuming alcoholic beverages.
-
Importance of informing clinicians about any concomitant illnesses, particularly depression.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Single-entity preparations of chlordiazepoxide and its hydrochloride salt and preparations containing the drug in combination with amitriptyline hydrochloride are subject to control under the Federal Controlled Substances Act of 1970 as schedule IV (C-IV) drugs.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
5 mg Chlordiazepoxide and Amitriptyline Hydrochloride 12.5 mg* |
chlordiazePOXIDE and Amitriptyline Hydrochloride Tablets ( C-IV) |
|
|
10 mg Chlordiazepoxide and Amitriptyline Hydrochloride 25 mg* |
chlordiazePOXIDE and Amitriptyline Hydrochloride Tablets ( C-IV) |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
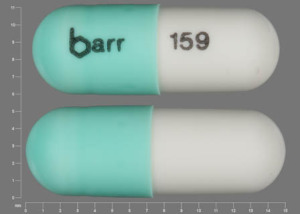
Oral |
Capsules |
5 mg* |
chlordiazePOXIDE Hydrochloride Capsules ( C-IV) |
|
|
10 mg* |
chlordiazePOXIDE Hydrochloride Capsules ( C-IV) |
|||
|
25 mg* |
chlordiazePOXIDE Hydrochloride Capsules ( C-IV) |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
5 mg Chlordiazepoxide Hydrochloride and Clidinium Bromide 2.5 mg* |
chlordiazePOXIDE Hydrochloride and Clidinium Bromide Capsules |
|
|
Librax |
Valeant |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions September 26, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about chlordiazepoxide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (207)
- Drug images
- Latest FDA alerts (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: benzodiazepines
- Breastfeeding
- En español