Bexarotene (Monograph)
Brand name: Targretin
Drug class: Antineoplastic Agents
Chemical name: 4-[1-(5,6,7,8-Tetrahydro-3,5,5,8,8-pentamethyl-2-naphthalenyl)ethenyl]benzoic acid
Molecular formula: C24H28O2
CAS number: 153559-49-0
Warning
May cause birth defects in humans; teratogenicity and embryolethality demonstrated in animals. Contraindicated in pregnant women. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Introduction
Antineoplastic agent; synthetic retinoid analog.
Uses for Bexarotene
Cutaneous T-cell Lymphoma
Treatment of skin manifestations of cutaneous T-cell lymphoma (CTCL) in patients who are refractory to at least one prior systemic therapy.
Within CTCL, some experts recommend oral bexarotene with skin directed therapies in mycosis fungoides uncontrolled with initial treatment, or with extracorporeal photopheresis in Sézary syndrome as first-line therapy.
Bexarotene Dosage and Administration
General
Pretreatment Screening
-
Obtain a fasting lipid profile. Fasting triglycerides should be normalized before initiating treatment with bexarotene.
-
Obtain a negative serum pregnancy test (e.g., serum beta-HCG with a sensitivity of at least 50 mIU/L within 1 week prior to initiation of bexarotene).
-
Obtain a CBC.
-
Obtain baseline liver function tests.
-
Obtain baseline thyroid function tests.
Patient Monitoring
-
Monitor lipids weekly during the first 2 to 4 weeks of starting bexarotene and manage elevations in serum lipid values during treatment. In patients who do not develop hyperlipidemia in the first 2 to 4 weeks of treatment, lipid monitoring may be carried out less frequently thereafter.
-
Obtain monthly pregnancy tests while the patient remains on bexarotene treatment.
-
Monitor CBC with differential periodically during treatment.
-
Monitor liver function tests 1, 2, and 4 weeks after treatment initiation, and if stable, at least every 8 weeks thereafter during treatment.
-
Monitor thyroid function tests during treatment as indicated.
Administration
Oral Administration
Administer orally once daily with a meal.
Dosage
Adults
CTCL
Oral
Initially, 300 mg/m2 daily.
Refer to Table 1 for the initial bexarotene dose of 300 mg/m2 daily according to BSA.
If no tumor response is observed after 8 weeks and the 300 mg/m2 daily dosage is well tolerated, increase to 400 mg/m2 daily with careful monitoring.
Continue as long as benefit is derived from therapy. Optimum duration is not known.
|
Body Surface Area (m2) |
Total Daily Dose (mg/day) |
|---|---|
|
0.88–1.12 |
300 |
|
1.13–1.37 |
375 |
|
1.38–1.62 |
450 |
|
1.63–1.87 |
525 |
|
1.88–2.12 |
600 |
|
2.13–2.37 |
675 |
|
2.38–2.62 |
750 |
Dosage Modification for Toxicity
If intolerable adverse effects occur, decrease dosage to 200 mg/m2 daily, then 100 mg/m2 daily, or temporarily discontinue. When toxicity is controlled, carefully readjust dosage upward.
Special Populations
Hepatic Impairment
No specific dosage recommendations for hepatic impairment.
Renal Impairment
No specific dosage recommendations for renal impairment.
Geriatric Patients
No specific dosage recommendations for geriatric patients.
Cautions for Bexarotene
Contraindications
-
Known or suspected pregnancy.
-
Known hypersensitivity to bexarotene or any ingredient in the formulation.
Warnings/Precautions
Fetal/Neonatal Morbidity and Mortality
A boxed warning about the risk of birth defects is included in the prescribing information for bexarotene. May cause fetal harm; teratogenicity and embryolethality demonstrated in animals. Exclude pregnancy 1 week prior to initiation of therapy. Initiate therapy on second or third day of normal menstrual period. Repeat pregnancy tests monthly during therapy. To facilitate pregnancy test assessment and counseling, dispense no more than 1 month supply.
If pregnancy occurs, immediately discontinue and apprise of potential fetal hazard.
Hyperlipidemia
Lipid abnormalities (e.g., hyperlipidemia, elevated fasting triglycerides and cholesterol, decreased HDL cholesterol) occur in most patients; usually develop within 2–4 weeks and are reversible with cessation of therapy.
If fasting triglycerides are or become elevated, institute antilipemic therapy and reduce bexarotene dosage or suspend therapy. Gemfibrozil is not recommended due to a potential drug-drug interaction. Monitor fasting blood lipid levels weekly until lipid response is established, then at 8-week intervals. For patients without hyperlipidemia, monitoring can be performed less frequently after 2–4 weeks of therapy.
Pancreatitis
Possible acute pancreatitis; possibly fatal. Patients with risk factors for pancreatitis (e.g., prior pancreatitis, uncontrolled hyperlipidemia or diabetes mellitus, excessive alcohol consumption, biliary tract disease, or therapy with drugs associated with pancreatic toxicity or known to increase triglyceride concentrations) generally should not receive bexarotene. Interrupt bexarotene treatment and evaluate if pancreatitis is suspected.
Hepatotoxicity, Cholestasis, and Hepatic Failure
Possible elevations in AST and ALT; usually resolve within 1 month following decrease in dosage or discontinuance.
Monitor liver function tests at baseline; after 1, 2, and 4 weeks of treatment; and at least every 8 weeks thereafter. Consider interruption or discontinuance if transaminases or bilirubin increase to 3 times ULN.
Hypothyroidism
Possible hypothyroidism. Consider thyroid supplementation in patients with laboratory evidence of hypothyroidism. Obtain baseline thyroid function tests and monitor during treatment.
Hematologic Effects
Leukopenia (generally neutropenia) possible, rarely associated with serious adverse events; time to onset usually 4–8 weeks, with resolution occurring within 30 days of dosage reduction or discontinuance of the drug in most patients. Obtain CBC with differential at baseline and periodically during therapy.
Cataracts
New cataracts or worsening of existing cataracts possible. Ophthalmologic evaluation recommended if visual difficulties occur.
Vitamin A Supplementation Hazard
Due to the relationship between bexarotene and vitamin A, limit vitamin A intake to <15,000 IU/day to limit toxic effects.
Photosensitivity Reactions
Sunburn and skin sensitivity to sunlight possible in patients exposed to direct sunlight. Minimize exposure to sunlight and artificial UV light.
Hypoglycemia Risk in Patients with Diabetes Mellitus
Patients using insulin, sulfonylureas, thiazolidinediones, or other oral agents while on bexarotene are at an increased risk for hypoglycemia, since bexarotene may enhance their effects. When used as monotherapy, bexarotene has not been associated with hypoglycemia.
Drug-Laboratory Test Interaction
In patients with ovarian cancer, CA125 assay values may be increased by bexarotene.
Specific Populations
Pregnancy
Contraindicated in pregnancy. Associated with birth defects in humans. In animal studies, bexarotene administration resulted in fetal harm. Obtain a negative serum pregnancy test within 1 week prior to starting bexarotene therapy, and perform pregnancy testing at monthly intervals during bexarotene therapy. (See Fetal/Neonatal Morbidity and Mortality and also Contraindications under Cautions.)
Lactation
Not known whether bexarotene is distributed into milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Females and Males of Reproductive Potential
Obtain a negative serum pregnancy test within 1 week prior to starting bexarotene therapy, and perform pregnancy testing at monthly intervals during bexarotene therapy. Use contraception (with 2 reliable forms, including at least one nonhormonal method) for 1 month before, during, and for at least 1 month after bexarotene administration. Male patients receiving the drug should use condoms during sexual intercourse with women who are or may become pregnant, and for at least 1 month after discontinuing bexarotene.
Geriatric Use
No substantial differences in safety relative to younger adults, but increased sensitivity cannot be ruled out.
Hepatic Impairment
No formal studies have been conducted with bexarotene. Hepatic impairment may reduce drug clearance; monitor for signs and symptoms of toxicity with reduced hepatic function.
Renal Impairment
No formal studies have been conducted with bexarotene. Due to changes in protein binding, the pharmacokinetics of bexarotene may be altered in renal impairment.
Common Adverse Effects
The most common adverse reactions (occurring in >10% of patients in clinical trials and at least possibly related to treatment) include: lipid abnormalities (elevated triglycerides, elevated total and LDL cholesterol, and decreased HDL cholesterol), hypothyroidism, headache, asthenia, rash, leukopenia, anemia, nausea, infection, peripheral edema, abdominal pain, dry skin.
Drug Interactions
Metabolized by CYP3A4. Possibly also an inducer of CYP3A4.
In vitro, bexarotene inhibits CYP2C8 and induces CYP3A4.
In vitro, bexarotene does not significantly inhibit CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, CYP2E1, or CYP3A4.
Drugs Affected by Hepatic Microsomal Enzymes
Substrates of CYP3A4: potential pharmacokinetic interaction (decreased plasma substrate concentrations).
Protein-bound Drugs
Potential pharmacokinetic interaction (bexarotene displacement by, or bexarotene displacement of, other protein-bound drugs).
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Antidiabetic agents (e.g., insulin, sulfonylureas, other oral antidiabetic agents) |
Potential increased incidence of hypoglycemia |
Use concomitantly with caution |
|
Antifungals (e.g., itraconazole, ketoconazole) |
Likely no interaction that alters bexarotene plasma concentrations |
|
|
Atorvastatin |
Decreased atorvastatin plasma concentrations |
|
|
Gemfibrozil |
Increased plasma bexarotene concentrations |
Concomitant use not recommended |
|
Hormonal contraceptives |
Decreased plasma concentrations of hormonal contraceptives |
|
|
Paclitaxel (plus carboplatin) |
Increased plasma bexarotene concentrations ; when administered with carboplatin Decreased plasma concentrations of paclitaxel |
|
|
Tamoxifen |
Decreased plasma tamoxifen concentrations |
|
|
Vitamin A |
Possible increased toxicity |
Bexarotene Pharmacokinetics
Absorption
Bioavailability
Absorbed following oral administration, with peak plasma concentrations attained within approximately 2 hours.
Food
Peak plasma concentrations and AUC (after 75–300 mg doses) increased by approximately 48 and 35%, respectively, after a meal containing fat compared with glucose solution.
Distribution
Extent
Distribution into body tissues and fluids has not been evaluated.
It is not known whether bexarotene is distributed into milk.
Plasma Protein Binding
>99%.
Special Populations
In patients with renal impairment, possible altered protein binding and pharmacokinetics.
No significant differences in pharmacokinetics based on age or gender.
Elimination
Metabolism
Metabolized extensively in the liver; in vitro, metabolized principally via CYP3A4 oxidation. Oxidative metabolites active in vitro; relative contributions of parent drug or metabolites to safety and efficacy unknown.
Elimination Route
Bexarotene and its metabolites eliminated principally via biliary excretion; not excreted in urine in appreciable amounts.
Half-life
Approximately 7 hours.
Special Populations
In patients with hepatic impairment, greatly decreased clearance expected.
Stability
Storage
Oral
Capsules
2–25°C. Avoid exposure to high temperatures and humidity after bottle is opened; protect from light.
Actions
-
Selectively binds with and activates retinoid X receptor (RXR) subtypes (RXRα, RXRβ, and RXRγ). Activated RXRs function as transcription factors that regulate the expression of genes controlling cellular differentiation and proliferation.
-
Exact mechanism(s) of action not determined, but bexarotene is active in all clinical stages of cutaneous T-cell lymphoma.
Advice to Patients
-
Risk of photosensitivity reactions.
-
Risk of hypoglycemia in patients being treated for diabetes mellitus.
-
Importance of women informing clinicians immediately if they are or plan to become pregnant; necessity of advising women and men to avoid pregnancy during therapy. Necessity of advising pregnant women of the risk to the fetus. Necessity of advising women of the importance of monthly pregnancy testing. Necessity of advising women to used effective contraception for 1 month prior to therapy, and for at least 1 month after discontinuing the drug, and that 2 methods of contraception should be used simultaneously, one of which should be non-hormonal. Necessity of advising men to use condoms during sexual intercourse while receiving the drug and for at least 1 month after discontinuing the drug.
-
Importance of advising patients about the risk of developing pancreatitis, which may present with symptoms of nausea, vomiting, and abdominal or back pain, and to contact their healthcare provider if these symptoms arise.
-
Importance of advising patients of the possibility of liver dysfunction or liver failure, and to immediately contact their healthcare provider if signs of liver failure occur, which include jaundice, anorexia, bleeding, or bruising.
-
Importance of advising patients of the possibility of neutropenia and to contact their healthcare provider if they develop a fever, particularly in the presence of any infection.
-
Importance of advising patients of the possibility of cataract development and the need for patients to inform their healthcare provider of any changes in vision.
-
Importance of checking blood sugar more frequently in patients with diabetes who are taking insulin, agents that enhance insulin secretion, or insulin sensitizers due to the increased risk of hypoglycemia with bexarotene.
-
Importance of advising patients of laboratory testing that will occur during therapy, which includes the monitoring of lipids, thyroid function, and white blood cell counts.
-
Importance of limiting vitamin A intake.
-
Importance of taking bexarotene with, or immediately following, a meal.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they plan to breast-feed.
-
Importance of informing patients of other important precautionary information.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
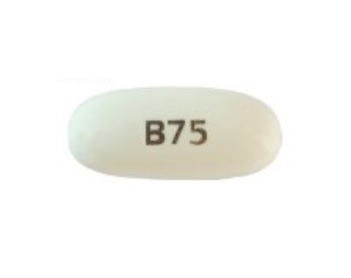
Oral |
Capsules |
75 mg* |
Targretin |
Bausch Health Companies |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 18, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about bexarotene
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- En español