Sick Sinus Syndrome
Medically reviewed by Drugs.com. Last updated on Jun 2, 2025.
What is sick sinus syndrome?
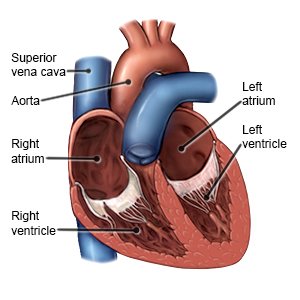
Sick sinus syndrome is a heart rhythm disorder. Your heart's rhythm (heartbeat) is controlled by a part of the heart called the sinus node. A normal rhythm is generally between 60 and 100 beats per minute. If the sinus node does not work properly, your heart may beat too slowly or too quickly. It may go back and forth from too slow to too fast. You may have pauses in between beats. Each of these rhythm problems may cause certain signs and symptoms.
 |
What are the symptoms I might have?
You may have only mild symptoms at first. Symptoms may come and go, or be present all the time. The following are common symptoms:
- Chest pain or heart palpitations (fast heartbeats that pound or flutter)
- Fatigue or weakness
- Shortness of breath, especially with activity
- Dizziness, fainting, or feeling like you are going to pass out
- Confusion or new trouble sleeping
How is sick sinus syndrome diagnosed?
Your healthcare provider will ask about your symptoms and when they started. He or she will ask what triggers your symptoms and if they get worse with exercise. Tell him or her if you have a heart condition or take any medicines. You may also need any of the following:
- An ECG records the electrical activity of your heart. It may be used to check for problems with the way electrical signals travel through your heart.
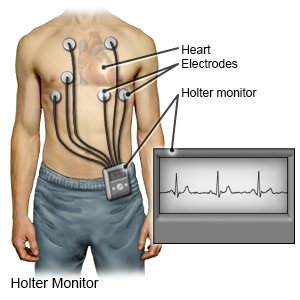
- A cardiac event monitor is used to track your heart rate and rhythm. This device is also called a Holter monitor or mobile telemetry. You may need to wear it for several days at home.
- A cardiac loop recorder is a device implanted in your chest or armpit, just under the skin. The device will record any heart rhythm problems automatically. You may also receive a handheld controller. You will press a button on the controller when you have symptoms, such as dizziness or lightheadedness. The device will record any rhythm problem happening at that moment.
- A cardiac stress test checks if your heart muscle is getting enough blood during rest and stress. Your heart may be placed under stress with medicine or exercise.
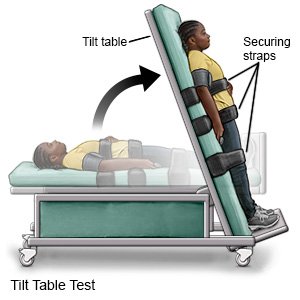
- A tilt table test checks your heart and blood pressure when your body changes positions.
- An electrophysiology study is a procedure to map the electrical pathways in your heart that control your heartbeat.
How is sick sinus syndrome treated?
Treatment may not be needed if your symptoms do not cause problems in your daily life. You may need any of the following if symptoms do cause problems:
- The cause of sick sinus syndrome may need to be treated. Your healthcare provider may make changes to medicines that are causing your symptoms. Heart disease or acute coronary syndrome may need to be managed. Low thyroid or blood sugar levels, or electrolyte balance problems may be corrected. Your provider may recommend that you lose weight if you are overweight.
- Medicines may be given to help control how fast or how strongly your heart beats. You may also need to take blood thinners to prevent clots. Clots can form if your heart does not pump strongly enough to keep the blood from pooling.
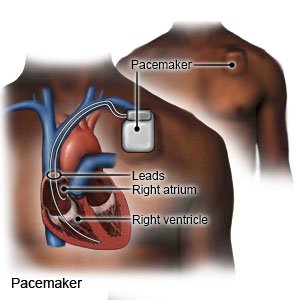
- A pacemaker is a device to help keep your heartbeat stable. A permanent pacemaker is implanted under the skin of your chest or abdomen during surgery. A battery creates electrical impulses that keep your heart rate regular.
What can I do to manage sick sinus syndrome?
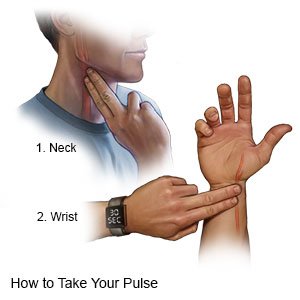
- Check your pulse as directed. Your healthcare provider will show you how to check your pulse. He or she will tell you how often to check it. Keep a record of your pulse rate. Include any details about your pulse. Examples include if it feels regular or like it is skipping beats. Also write down the activity you were doing if your heart rate goes below 60 or above 100 beats per minute. Bring the record with you to your follow-up appointments.
- Do not smoke. Nicotine and other chemicals in cigarettes can cause damage to your heart. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Limit alcohol as directed. Alcohol can worsen heart problems and may lead to heart failure. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Eat heart-healthy foods. These include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Replace butter and margarine with heart-healthy oils such as olive oil and canola oil. Ask for more information on heart-healthy diets such as the DASH eating plan.

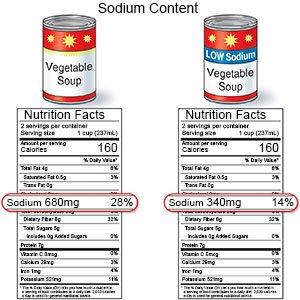
- Limit sodium (salt) as directed. Too much sodium can affect your fluid balance. Check labels to find low-sodium or no-salt-added foods. Your healthcare provider will tell you how much sodium is safe for you to have in a day. He or she may recommend that you limit sodium to 2,300 mg a day.
- Exercise regularly and maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. He or she can help you create a weight loss plan if you are overweight. Exercise can help keep your heart healthy, and help you reach or maintain a healthy weight. Your provider may recommend at least 30 minutes of physical activity on most days of the week.
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
When should I call my doctor?
- You have new or worsening symptoms.
- You have swelling in your ankles or feet.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Sick Sinus Syndrome
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
