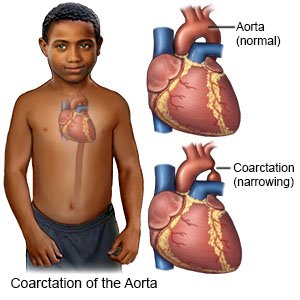
Coarctation of the Aorta
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is coarctation of the aorta (COA)?
COA is a birth defect that causes a narrowing in your child's aorta. The aorta is the large blood vessel that moves blood from your child's heart to the rest of his or her body. COA makes the heart work harder than usual to pump blood and oxygen to your child's body. Over time, this may weaken the heart muscle and cause heart failure.
 |
What causes COA?
There is no known cause of COA. Your child's risk for COA may increase if his or her mother eats or drinks certain foods, or takes certain medicines, during pregnancy. Your child's risk for COA may also increase if he or she has other heart defects.
What are the signs and symptoms of COA?
- Heavy sweating or irritability in infants
- Headaches, nosebleeds, and leg cramps in older children
- Chest pain
- Cold or pale legs and feet
- Fast breathing or shortness of breath that gets worse with exercise
- Feeling tired, dizzy, or faint
- Problems eating, poor weight gain, and slow growth
How is COA diagnosed and treated?
The healthcare provider will examine your child. Your child may need an ultrasound, x-ray, MRI, or CT. These tests will show the narrowed aorta. Your child may be given contrast liquid to help the pictures show up better. Tell the healthcare provider if your child has ever had an allergic reaction to contrast liquid. Do not let your child enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if your child has any metal in or on his or her body. Your child may need any of the following to treat COA:
- Medicine may be given to control or lower your child's blood pressure. Medicine may also be given to decrease stress on your child's heart.
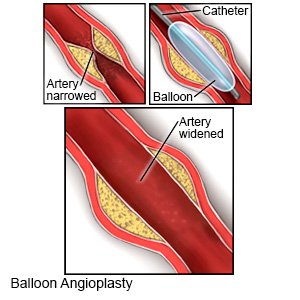
- Balloon angioplasty is a procedure to widen the aorta with a balloon.
- Surgery may be needed to repair the COA. Ask your child's healthcare provider for more information on COA repair.
What can I do to care for my child?
- Do not smoke near your child. Do not let your older child smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Ask your healthcare provider for information if you or your older child currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you or your older child use these products.
- Feed your child heart-healthy foods. Feed your child more fresh fruits and vegetables. Limit foods high in sodium, such as canned and processed foods. Replace butter and margarine with heart-healthy oils such as olive oil and canola oil. Other heart-healthy foods include walnuts, whole-grain breads, low-fat dairy products, beans, and lean meats. Fatty fish such as salmon and tuna are also heart healthy.

- Ask your child's healthcare provider if you need to limit his or her activity. Your child may need to avoid strenuous activities and sports to decrease his or her symptoms. Strenuous activities include running, lifting, and swimming.
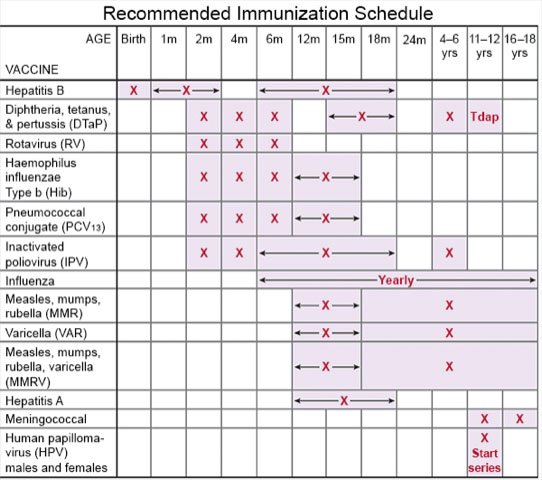
- Get your child vaccinated. Vaccines help decrease your child's risk for infections. Infections can make your child's condition worse. Your child's healthcare provider can tell you which vaccines your child needs and when to get them.
Call your local emergency number (911 in the US) if:
- Your child has severe chest pain.
- Your child has trouble breathing or sudden shortness of breath.
- Your child coughs up blood.
- Your child loses consciousness or stops breathing.
- Your child has any of the following signs of a stroke:
- Part of his or her face droops or is numb
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
When should I seek immediate care?
- Your child is too dizzy to stand.
- Your child's heart is beating faster than usual.
- Your child has swelling in his or her legs or ankles.
- Your child has severe abdominal pain or his abdomen is larger than usual.
When should I call my child's doctor?
- Your child has a fever.
- Your child has chills, a cough, or feels weak and achy.
- You have questions or concerns about your child's condition or care.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
