Intracranial Hematoma
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is an intracranial hematoma?
An intracranial hematoma is a collection of blood inside your skull. The blood leaks from a tear or rupture in a vein or artery, such as after a hemorrhagic stroke. The collected blood puts pressure on the brain. Serious medical problems can develop, such as seizures or a coma. An intracranial hematoma is a life-threatening emergency that needs immediate medical care.
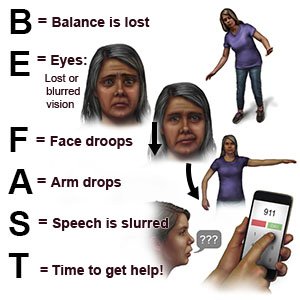
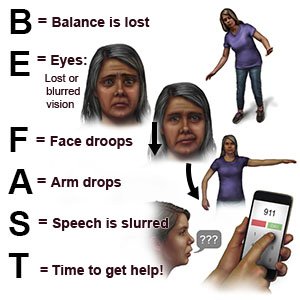
What are the warning signs of a stroke?
The words BE FAST can help you remember and recognize warning signs of a stroke:
- B = Balance: Sudden loss of balance
- E = Eyes: Loss of vision in one or both eyes
- F = Face: Face droops on one side
- A = Arms: Arm drops when both arms are raised
- S = Speech: Speech is slurred or sounds different
- T = Time: Time to get help immediately
 |
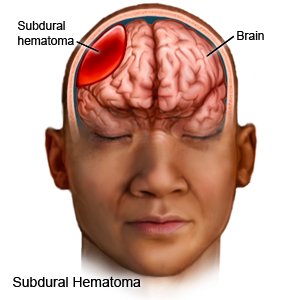
What are the types of intracranial hematoma?
- Intracerebral (or intraparenchymal) hematoma is blood that collects within brain tissue.
- Subdural hematoma is blood that collects between your brain and its protective cover.
- Epidural hematoma is blood that collects between your brain's protective cover and your skull.
What are the signs and symptoms of an intracranial hematoma?
Signs and symptoms may develop over minutes, hours, or years. You may have any of the following, depending on where the hematoma happened:
- Headache, seizures, or confusion
- Weak or numb areas, or a stiff neck
- Trouble speaking, or slurred speech
- Fainting, loss of consciousness, or being less alert
- Nausea and vomiting
- Trouble walking or keeping your balance
- Vision problems
What causes or increases my risk for an intracranial hematoma?
- A head injury, such as a blow to the head or from a sudden stop after fast motion
- Blood thinning medicine
- Older age
- High blood pressure that is not controlled
- Medical conditions such as diabetes, liver disease, or blood vessel weakness
- Use of alcohol or illegal drugs such as cocaine or heroin
How is an intracranial hematoma diagnosed?
Your healthcare provider will check for high blood pressure or another medical condition that increases your risk for bleeding. You may also need any of the following:
- CT or MRI pictures are used to find the bleeding and check for damage to your brain. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- Blood tests may be used to check your overall health. The tests may include a check for diabetes or a blood clotting disorder. Diabetes or a blood clotting disorder can increase your risk for a stroke that can lead to a hematoma.
How is an intracranial hematoma treated?
- Bed rest may be needed if you have a small amount of blood in the dura. Healthcare providers may want to see you often or do CT or MRI scans to be sure there is no more bleeding.
- Medicines are used to prevent seizures, lower swelling, and get rid of extra fluid.
- A catheter (thin tube) may be placed in your skull to drain fluid. This will help decrease pressure in your brain and prevent more damage. The tube may also monitor pressure in your brain.
- Surgery may be used to remove the blood.
What can I do to manage or prevent an intracranial hematoma?
Healthcare providers will help you create goals for your recovery. The following lifestyle changes can help lower your risk for a stroke that can lead to a hematoma:
- Manage health conditions. A condition such as diabetes can increase your risk for a stroke. Control your blood sugar level if you have hyperglycemia or diabetes. Take your prescribed medicines and check your blood sugar level as directed.

- Check your blood pressure as directed. High blood pressure can increase your risk for a stroke. Follow your healthcare provider's directions for controlling your blood pressure.

- Limit alcohol. Large amounts of alcohol can lead to an intracerebral hematoma or a stroke. Alcohol may also raise your blood pressure or thin your blood. Blood thinning can cause a hemorrhagic stroke.
- Do not use nicotine products or illegal drugs. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage. Nicotine and illegal drugs both increase your risk for a stroke. Ask your healthcare provider for information if you currently smoke or use drugs and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Take blood thinners exactly as directed. Blood thinners increase your risk for an intracerebral hematoma. Your healthcare provider may make changes to your blood thinner if it caused your hematoma. Always follow directions so you do not take too much of this medicine.
- Eat a variety of healthy foods. Healthy foods include whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Eat at least 5 servings of fruits and vegetables each day. Choose foods that are low in fat, cholesterol, salt, and sugar. Eat foods that are high in potassium, such as potatoes and bananas. A nutritionist can help you create healthy meal plans.

- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan if you are overweight. He or she can help you create small goals if you have a lot of weight to lose.
- Exercise as directed. Exercise can lower your blood pressure, cholesterol, weight, and blood sugar levels. Healthcare providers will help you create exercise goals. They can also help you make a plan to reach your goals. For example, you can break exercise into 10 minute periods, 3 times in a day. Find an exercise that you enjoy. This will make it easier for you to reach your exercise goals.

- Manage stress. Stress can raise your blood pressure. Find new ways to relax, such as deep breathing or listening to music.
Where can I get support and more information?
- American Stroke Association
Phone: 1- 888 - 478-7653
Web Address: http://www.stroke.org
Have someone call your local emergency number (911 in the US) if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have a seizure.
- You have new problems with balance or movement.
When should I seek immediate care?
- You are sleepier or are harder to wake than usual.
- You have problems thinking.
- Your behavior or personality has changed.
- You have repeated or forceful vomiting or you cannot keep liquids down.
When should I call my doctor?
- You have nausea or are vomiting.
- Your symptoms are getting worse.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Intracranial Hematoma
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
