Hysterotomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
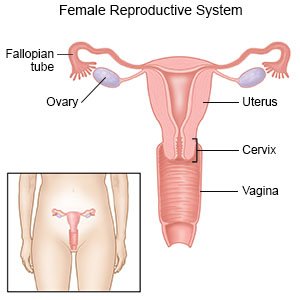
A hysterotomy
is an incision made in your uterus. This allows your surgeon to work directly inside your uterus. A hysterotomy may be used during pregnancy. For example, a heart problem in a fetus may be fixed before he or she is born. A hysterotomy may also be used if a baby needs to be delivered quickly. A hysterotomy may also be used to end a pregnancy during the second or third trimester.
 |
How to prepare for a hysterotomy:
- Your surgeon will tell you how to prepare. This depends on the reason you are having a hysterotomy. Your surgeon may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange for someone to drive you home and stay with you after surgery.
- Tell your surgeon about all your current medicines. Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of your surgery.
- Tell your provider about all your allergies, including to anesthesia or medicines. You will be given an antibiotic to help prevent a bacterial infection.
What will happen during a hysterotomy:
- General anesthesia may be given to keep you asleep and free from pain during surgery. You may instead be given regional anesthesia to numb the surgery area. You will be awake with regional anesthesia, but you should not feel pain.
- Your surgeon will make an incision in your abdomen. Your surgeon may need to bring your uterus partially out of the incision. This depends on the reason you are having a hysterotomy. A second incision will be made in your uterus. Your surgeon will complete any other work, such as surgery on a fetus. When your surgeon finishes, the incision into the uterus will be closed with absorbable stitches. Your uterus may need to be put back through the incision in your abdomen.
- Your surgeon will close the incision in your abdomen with stitches or staples. A bandage will help keep the area clean and dry to prevent infection.
What to expect after a hysterotomy:
- Medicine may be given to prevent or treat pain, nausea, or a bacterial infection.
- You will be helped to walk around after surgery. You may also be given exercises to do in bed. Movement helps prevent blood clots. You may also be given an incentive spirometer to help prevent a lung infection. The spirometer will help you take deep breaths.
- Drains may be used to remove blood or fluid from the surgery area. The drains will be removed at a later time.
Risks of a hysterotomy:
You may bleed more than expected or develop an infection. Your bladder or intestines may be injured during the procedure. You may get a blood clot in your leg. This may become life-threatening.
Call your local emergency number (911 in the US) for any of the following:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have increasing abdominal or pelvic pain.
- You have heavy vaginal bleeding that fills 1 or more sanitary pads in 1 hour.
- You have a fever.
Call your surgeon or gynecologist if:
- You have nausea or are vomiting.
- You feel pain or burning when you urinate, or you have trouble urinating.
- You have pus or a foul-smelling odor coming from your vagina.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
Your surgeon may give you specific instructions based on the reason for your hysterotomy. The following are general guidelines:
- Rest as needed. Get up and move around as directed to help prevent blood clots. Start with short walks and slowly increase the distance every day. Limit the number of times you climb stairs to a few times a day for the first 2 weeks. Plan most of your daily activities on one level of your home. Ask when it is safe for you to drive, return to work, and return to other regular activities.
- Do not put pressure on the surgery area. Do not lift objects heavier than 10 pounds for 6 weeks, or as directed. Do not strain during bowel movements. High-fiber foods and extra liquids can help you prevent constipation. Examples of high-fiber foods are fruit and bran. Prune juice and water are good liquids to drink.

- Keep the area clean and dry. You may need to keep the bandage on for 1 to 2 days or until your follow-up visit. Usually you will not need to cover your incision after the bandage is removed.
Follow up with your surgeon or gynecologist as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
