Floxin Side Effects
Generic name: ofloxacin
Medically reviewed by Drugs.com. Last updated on Jul 31, 2024.
Note: This document provides detailed information about Floxin Side Effects associated with ofloxacin. Some dosage forms listed on this page may not apply specifically to the brand name Floxin.
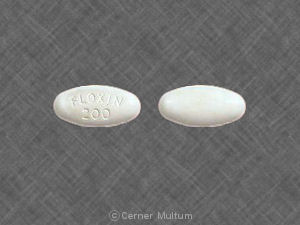
Applies to ofloxacin: oral tablet.
Important warnings
This medicine can cause some serious health issues
Oral route (tablet)
Fluoroquinolones, including ofloxacin, are associated with disabling and potentially irreversible serious adverse reactions that have occurred together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects.
Discontinue ofloxacin and avoid use of fluoroquinolones in patients with these serious adverse reactions.
Reserve use of ofloxacin for patients with no alternative treatment options for acute exacerbation of chronic bronchitis or uncomplicated cystitis.
Fluoroquinolones, including ofloxacin, may exacerbate muscle weakness in persons with myasthenia gravis.
Avoid in patients with known history of myasthenia gravis.
Serious side effects of Floxin
Along with its needed effects, ofloxacin (the active ingredient contained in Floxin) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking ofloxacin:
Less common
- abdominal or stomach pain
- anxiety
- black, tarry stools
- bleeding gums
- blood in the urine or stools
- blurred vision
- body aches or pain
- chest pain
- chills
- cloudy urine
- cold sweats
- coma
- confusion
- congestion
- cool, pale skin
- cough
- depression
- diarrhea
- dry mouth
- dryness or soreness of the throat
- eye pain
- fast heartbeat
- fever
- flushed, dry skin
- fruit-like breath odor
- general feeling of illness
- headache
- hoarseness
- increased hunger
- increased thirst
- increased urination
- lower back or side pain
- nausea
- nightmares
- painful or difficult urination
- pale skin
- pinpoint red spots on the skin
- pus in the urine
- runny nose
- seizures
- shakiness
- slurred speech
- sore throat
- sores, ulcers, or white spots on the lips or in the mouth
- sweating
- swollen glands
- tender, swollen glands in the neck
- trouble with swallowing
- troubled breathing with exertion
- unexplained weight loss
- unusual bleeding or bruising
- unusual tiredness or weakness
- voice changes
- vomiting
Rare
- burning while urinating
- burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feelings
- change in color vision
- continuing ringing or buzzing or other unexplained noise in the ears
- convulsions
- decrease in frequency of urination
- decrease in urine volume
- decreased hearing or any change in hearing
- difficult or painful urination
- difficulty in passing urine (dribbling)
- difficulty seeing at night
- difficulty with moving
- discouragement
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- false or unusual sense of well-being
- fast, irregular, pounding, or racing heartbeat or pulse
- feeling of constant movement of self or surroundings
- feeling of warmth or heat
- feeling sad or empty
- flushing or redness of the skin, especially on the face and neck
- hearing loss
- hives or welts, itching, or skin rash
- increased need to urinate
- increased sensitivity of the eyes to sunlight
- increased sweating
- irritability
- joint pain
- lack of appetite
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- loss of bladder control
- loss of interest or pleasure
- muscle aching or cramping
- muscle pains or stiffness
- muscle spasm or jerking of all extremities
- no blood pressure or pulse
- no breathing
- passing urine more often
- pounding in the ears
- redness, soreness, or itching skin
- seeing, hearing, or feeling things that are not there
- sensation of spinning
- shakiness in the legs, arms, hands, or feet
- slow or fast heartbeat
- sores, welting, or blisters
- stopping of the heart
- sudden loss of consciousness
- swelling
- swollen joints
- trembling or shaking of the hands or feet
- trouble concentrating
- trouble performing routine tasks
- trouble sleeping
- unconsciousness
Incidence not known
- abdominal or stomach tenderness
- actions that are out of control
- back, leg, or stomach pains
- blistering, peeling, or loosening of the skin
- bloating
- blue lips and fingernails
- burning, dry, or itching eyes
- changes in behavior
- confusion about identity, place, and time
- coughing that sometimes produces a pink frothy sputum
- coughing up blood
- cracks in the skin
- crying
- dark-colored urine
- darkening of the skin
- delusions of persecution, mistrust, suspiciousness, and/or combativeness
- depersonalization
- diarrhea, watery and severe, which may also be bloody
- difficulty with breathing, chewing, speaking, or swallowing
- discharge or excessive tearing
- double vision
- drooling
- drooping eyelids
- dysphoria
- euphoria
- feeling of discomfort
- general body swelling
- heartburn
- high fever
- hyperventilation
- increased blood pressure
- increased menstrual flow or vaginal bleeding
- increased sensitivity of the skin to sunlight
- increased sweating
- indigestion
- inflammation of the joints
- irregular heartbeats
- irregular or slow heart rate
- itching of the vagina or outside the genitals
- loss of ability to use or understand speech or language
- loss of appetite
- loss of balance control
- loss of heat from the body
- mental depression
- mood or mental changes
- muscle weakness
- noisy breathing
- nosebleeds
- numbness of the hands
- pain during sexual intercourse
- pain in the ankles or knees
- pain, inflammation, or swelling in the calves, shoulders, or hands
- painful, red lumps under the skin, mostly on the legs
- paralysis
- prolonged bleeding from cuts
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- quick to react or overreact emotionally
- rapidly changing moods
- red or black, tarry stools
- red or dark brown urine
- red skin lesions, often with a purple center
- red, irritated eyes
- red, swollen skin
- redness or other discoloration of the skin
- redness, pain, or swelling of the eye, eyelid, or inner lining of the eyelid
- restlessness
- scaly skin
- severe abdominal or stomach pain, cramping, or burning
- severe sunburn
- severe tiredness
- shaking
- shuffling walk
- stiffness of the limbs
- stomach pain, continuing
- swelling of the face, fingers, or lower legs
- swollen lymph glands
- talking, feeling, and acting with excitement
- thick, white, curd-like vaginal discharge without odor or with mild odor
- thoughts of killing oneself
- twisting movements of the body
- uncontrolled eye movements
- uncontrolled movements, especially of the face, neck, and back
- unexplained bleeding or bruising
- unpleasant breath odor
- unsteadiness or awkwardness
- unusual behavior, such as disorientation to time or place, failure to recognize people, hyperactivity, or restlessness, especially in children using 2% cyclopentolate
- unusual weight loss
- upper right abdominal or stomach pain
- vomiting of blood or material that looks like coffee grounds
- weakness in the arms, hands, legs, or feet
- weight gain
- yellowing of the eyes or skin
Other side effects of Floxin
Some side effects of ofloxacin may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
- change in taste
- excess air or gas in the stomach or intestines
- full feeling
- loss of taste
- passing gas
- runny nose
For healthcare professionals
Applies to ofloxacin: intravenous solution, oral tablet.
General
This drug was generally well tolerated, and side effects were mild in nature. In clinical trials, 11% of patients experienced side effects. Therapy was discontinued due to side effects in 4% of patients.[Ref]
Gastrointestinal
- Common (1% to 10%): Nausea, diarrhea, vomiting, abdominal pain and cramps, dry mouth, flatulence, gastrointestinal distress, constipation
- Uncommon (0.1% to 1%): Abdominal pain
- Rare (0.01% to 0.1%): Enterocolitis (sometimes hemorrhagic)
- Frequency not reported: Dyspepsia
- Postmarketing reports: Pseudomembranous colitis, gastrointestinal hemorrhage, intestinal perforation, hiccough, pyrosis, painful oral mucosa, pancreatitis, stomatitis[Ref]
The onset of pseudomembranous colitis symptoms has been reported during or after antimicrobial therapy.
Dyspepsia, flatulence, and constipation have also been reported during postmarketing experience. According to some authorities, pseudomembranous colitis was reported very rarely.[Ref]
Nervous system
- Common (1% to 10%): Headache, dizziness, dysgeusia, somnolence
- Uncommon (0.1% to 1%): Vertigo
- Rare (0.01% to 0.1%): Paresthesia, parosmia
- Very rare (less than 0.01%): Extrapyramidal symptoms or other disorders of muscular coordination, tinnitus, hearing loss
- Frequency not reported: Seizures, cognitive change, syncope, tremor, decreased hearing acuity, sensory axonal polyneuropathy, sensorimotor axonal polyneuropathy, idiopathic intracranial hypertension
- Postmarketing reports: Peripheral neuropathy (may be irreversible), peripheral sensory neuropathy, convulsion, peripheral sensory motor neuropathy, ataxia, incoordination, exacerbation of myasthenia gravis, exacerbation of extrapyramidal disorders, dysphasia, lightheadedness, taste disturbance, smell disturbance, hearing disturbance, equilibrium disturbance, dyskinesia, ageusia, hearing impaired[Ref]
Seizures were more likely to occur in elderly patients and in patients with renal dysfunction.
Cases of sensory or sensorimotor axonal polyneuropathy (affecting small and/or large axons) resulting in paresthesias, hypoesthesias, dysesthesias, and weakness have been reported.
A survey reported 6 cases of peripheral neuropathy associated with this drug. In 1 case, a 49-year-old female developed diffuse numbness, "pins and needles" sensation, burning pain, memory loss, visual impairment, joint pain, palpitations, altered sense of smell, insomnia, tinnitus, and severe panic attacks, with some symptoms persisting after 3 years.
Disturbances of taste, smell, hearing, and equilibrium were usually reversible after the drug was stopped.
Syncope and tremor have also been reported during postmarketing experience. According to some authorities, peripheral sensory neuropathy, peripheral sensory motor neuropathy, and convulsion were reported very rarely.[Ref]
Renal
- Common (1% to 10%): Increased serum creatinine, increased BUN
- Very rare (less than 0.01%): Acute renal failure
- Frequency not reported: Nephrogenic diabetic insipidus
- Postmarketing reports: Renal calculi, renal failure, interstitial nephritis, acute interstitial nephritis[Ref]
Hepatic
- Common (1% to 10%): Elevated AST, elevated ALT
- Rare (0.01% to 0.1%): Elevated liver enzymes (ALT, AST, LDH, GGT, alkaline phosphatase), elevated blood bilirubin
- Very rare (less than 0.01%): Cholestatic jaundice
- Postmarketing reports: Hepatic dysfunction (including hepatic necrosis, jaundice [cholestatic or hepatocellular], hepatitis [including severe cases]), hepatic failure (including fatal cases), elevated liver function tests (including GGT, LDH, bilirubin), severe liver injury (including acute liver failure [sometimes fatal])[Ref]
Severe liver injury (including cases of acute liver failure [sometimes fatal]) has been reported, primarily in patients with underlying liver disorders.[Ref]
Hematologic
- Common (1% to 10%): Anemia, leukopenia, leukocytosis, neutropenia, neutrophilia, increased band forms, lymphocytopenia, eosinophilia, lymphocytosis, thrombocytopenia, thrombocytosis, elevated erythrocyte sedimentation rate
- Very rare (less than 0.01%): Hemolytic anemia
- Postmarketing reports: Aplastic anemia, hemorrhage, pancytopenia, agranulocytosis, reversible bone marrow depression, thrombotic thrombocytopenic purpura, petechiae, prothrombin time prolongation, ecchymosis/bruising, bone marrow failure[Ref]
Anemia (including hemolytic), leukopenia, and thrombocytopenia have also been reported during postmarketing experience.[Ref]
Local
IV formulation:
- Common (1% to 10%): Injection site reactions (including phlebitis, swelling, erythema, pain)[Ref]
Musculoskeletal
- Rare (0.01% to 0.1%): Tendinitis
- Very rare (less than 0.01%): Arthralgia, myalgia, tendon rupture (e.g., Achilles tendon)
- Postmarketing reports: Muscular weakness, rhabdomyolysis, myopathy, muscle tear, muscle rupture, ligament rupture, arthritis[Ref]
Tendinitis and tendon rupture have also been reported during postmarketing experience. Tendon rupture (sometimes bilateral) has been reported within 48 hours of starting therapy.[Ref]
Cardiovascular
- Rare (0.01% to 0.1%): Tachycardia, hypotension
- Frequency not reported: Cardiac arrest, hypertension, palpitations, vasodilation
- Postmarketing reports: Cerebral thrombosis, hypotension/shock, ventricular arrhythmias, ECG QT prolonged, torsades de pointes[Ref]
Torsades de pointes were reported primarily in patients with risk factors for QT prolongation. This drug was associated with 2 cases of torsades de pointes reported to the US FDA between 1996 and 2001.
Tachycardia has also been reported during postmarketing experience. Tachycardia and hypotension have occurred during IV infusion (during postmarketing experience); in very rare cases, such a decrease in blood pressure has been severe.[Ref]
Hypersensitivity
- Postmarketing reports: Anaphylactic reactions/shock, anaphylactoid reactions/shock, serum sickness[Ref]
According to some authorities, anaphylactic reaction and anaphylactoid reaction were reported rarely and anaphylactic shock and anaphylactoid shock were reported very rarely.[Ref]
Genitourinary
- Common (1% to 10%): External genital pruritus in women, vaginitis, vaginal discharge, glucosuria, proteinuria, alkalinuria, hyposthenuria, hematuria, pyuria
- Frequency not reported: Dysuria; urinary frequency; urinary retention; dysmenorrhea; menorrhagia; metrorrhagia; burning, irritation, pain, and rash of the female genitalia
- Postmarketing reports: Vaginal candidiasis, albuminuria, candiduria, anuria, polyuria
Quinolones:
- Frequency not reported: Crystalluria, cylindruria[Ref]
Hematuria has also been reported during postmarketing experience.
Crystalluria and cylindruria have been reported with other quinolones.[Ref]
Dermatologic
- Common (1% to 10%): Rash, pruritus
- Rare (0.01% to 0.1%): Urticaria, hyperhidrosis, pustular rash
- Very rare (less than 0.01%): Erythema multiforme, toxic epidermal necrolysis, drug eruption, vascular purpura, vasculitis (sometimes leading to skin necrosis)
- Frequency not reported: Angioedema, diaphoresis
- Postmarketing reports: Hyperpigmentation, Stevens-Johnson syndrome, erythema nodosum, exfoliative dermatitis, photosensitivity/phototoxicity reaction, vesiculobullous eruption, purpura, acute generalized exanthematous pustulosis, drug rash[Ref]
A 75-year-old male developed toxic epidermal necrolysis and died of complications after receiving a total of 23.6 g of this drug orally over 51 days.
Angioedema, erythema multiforme, and toxic epidermal necrolysis have also been reported during postmarketing experience. According to some authorities, angioedema was reported rarely and photosensitivity was reported very rarely.[Ref]
Ocular
- Common (1% to 10%): Visual disturbances
- Uncommon (0.1% to 1%): Eye irritation
- Frequency not reported: Photophobia
- Postmarketing reports: Diplopia, nystagmus, blurred vision, conjunctivitis, uveitis
Quinolones:
- Frequency not reported: Ophthalmologic abnormalities (including cataracts, multiple punctate lenticular opacities)[Ref]
Ophthalmologic abnormalities (including cataracts and multiple punctate lenticular opacities) have been reported with other quinolones.[Ref]
Other
- Common (1% to 10%): Fatigue, chest pain, fever, trunk pain, elevated alkaline phosphatase
- Uncommon (0.1% to 1%): Fungal infection, pathogen resistance
- Rare (0.01% to 0.1%): Hot flushes
- Frequency not reported: Asthenia, chills, malaise, edema, extremity pain, pain, thirst, weight loss
- Postmarketing reports: Elevated serum triglycerides, elevated serum cholesterol, elevated serum potassium, pyrexia, pain (including back, chest, extremities)[Ref]
Asthenia has also been reported during postmarketing experience.[Ref]
Respiratory
- Common (1% to 10%): Pharyngitis
- Uncommon (0.1% to 1%): Cough, nasopharyngitis
- Rare (0.01% to 0.1%): Dyspnea, bronchospasm
- Frequency not reported: Respiratory arrest, rhinorrhea, epistaxis
- Postmarketing reports: Allergic pneumonitis, pulmonary edema, stridor[Ref]
Dyspnea (including severe dyspnea) and bronchospasm have also been reported during postmarketing experience.[Ref]
Metabolic
- Common (1% to 10%): Decreased appetite, hyperglycemia, hypoglycemia
- Rare (0.01% to 0.1%): Anorexia
- Postmarketing reports: Acidosis, hypoglycemic coma, porphyria attacks[Ref]
Hyperglycemia and hypoglycemia (especially in diabetic patients on insulin or oral hypoglycemic agents) have also been reported during postmarketing experience. Attacks of porphyria have been reported in patients with porphyria.[Ref]
Psychiatric
- Common (1% to 10%): Insomnia, nervousness, sleep disorders
- Uncommon (0.1% to 1%): Agitation
- Rare (0.01% to 0.1%): Anxiety, depression, confusional state, psychotic disorder/reactions (e.g., hallucination), nightmares
- Frequency not reported: Dream abnormality, euphoria, hallucinations
- Postmarketing reports: Restlessness, psychotic disorder and depression with self-endangering behavior (including suicidal ideation, suicide attempt), suicidal thoughts or acts, disorientation, paranoia, phobia, aggressiveness/hostility, manic reaction, emotional lability[Ref]
In 1 patient, a psychotic reaction to this drug presented with irritability, restlessness, insomnia, and irrational fear. The reaction was treated with haloperidol and resolved within 48 hours. One study suggests that the central nervous system effects of quinolones may be due to an interaction with the benzodiazepine-gamma-aminobutyric acid receptor complex and may be controlled by benzodiazepine administration.
Agitation, nervousness, psychotic reactions, and nightmares have also been reported during postmarketing experience.[Ref]
References
1. Todd PA, Faulds D (1991) "Ofloxacin: a reappraisal of its antimicrobial activity, pharmacology, and therapeutic use." Drugs, 42, p. 825-76
2. Smith JT (1991) "Ofloxacin, a bactericidal antibacterial." Chemotherapy, 37, p. 2-13
3. Guay DR, Opsahl JA, McMahon FG, Vargas R, Matzke GR, Flor S (1992) "Safety and pharmacokinetics of muliple doses of intravenous ofloxacin in healthy volunteers." Antimicrob Agents Chemother, 36, p. 308-12
4. (2001) "Product Information. Floxin (ofloxacin)." Ortho McNeil Pharmaceutical
5. Cerner Multum, Inc. "UK Summary of Product Characteristics."
6. Marchbanks CR, Dudley MN, Flor S, Beals B (1992) "Pharmacokinetics and safety of single rising doses of ofloxacin in healthy volunteers." Pharmacotherapy, 12, p. 45-9
7. Basista MP (1991) "Randomized study to evaluate efficacy and safety of ofloxacin vs trimethoprim and sulfamethoxazole in treatment of uncomplicated urinary tract infection." Urology, 37, p. 21-7
8. Fostini R, Girelli M, Dalle VP, Benedetti M, Recchia G (1988) "Safety profile of ofloxacin in elderly patients." Drugs Exp Clin Res, 14, p. 393-5
9. Giamarellou H, Tsagarakis J (1987) "Efficacy and tolerance of oral ofloxacin in treating various infections." Drugs, 34, p. 119-23
10. Wendel GD, Cox SM, Bawdon RE, Theriot SK, Heard MC, Nobles BJ (1991) "A randomized trial of ofloxacin versus cefoxitin and doxycycline in the outpatients treatment of acute salpingitis." Am J Obstet Gynecol, 164, p. 1390-6
11. Dan M, Samra Z (1989) "Clostridium difficile colitis associated with ofloxacin therapy." Am J Med, 87, p. 479
12. Tack KJ, Smith JA (1989) "The safety profile of ofloxacin." Am J Med, 87, s78-81
13. Unseld E, Ziegler G, Gemeinhardt A, Janssen U, Klotz U (1990) "Possible interaction of fluoroquinolones with benzodiazepine-GABA-receptorn complex." Br J Clin Pharmacol, 30, p. 63-70
14. Fennig S, Mauas L (1992) "Ofloxacin-induced delirium." J Clin Psychiatry, 53, p. 137-8
15. Kohler RB, Arkins N, Tack KJ (1991) "Accidental overdose of intravenous ofloxacin with benign outcome." Antimicrob Agents Chemother, 35, p. 1239-40
16. Getenet JC, Croisile B, Vighetto A, et al. (1993) "Idiopathic intracranial hypertension after ofloxacin treatment." Acta Neurol Scand, 87, p. 503-4
17. Thomas RJ, Regan DR (1996) "Association of a tourette-like syndrome with ofloxacin." Ann Pharmacother, 30, p. 138-41
18. Traeger SM, Bonfiglio MF, Wilson JA, Martin BR, Nackes NA (1995) "Seizures associated with ofloxacin therapy." Clin Infect Dis, 21, p. 1504-6
19. Walton GD, Hon JK, Mulpur TG (1997) "Ofloxacin-induced seizure." Ann Pharmacother, 31, p. 1475-7
20. Cohen JS (2001) "Peripheral neuropathy associated with fluoroquinolones." Ann Pharmacother, 35, p. 1540-7
21. Hofer T, Becker EW, Weigand K, Berg PA (1992) "Demonstration of sensititzed lymphocytes to trimethoprim/sulfamethoxazole and ofloxacin in a patient with cholestatic hepatitis." J Hepatol, 15, p. 262-3
22. Blum A (1991) "Ofloxacin-induced acute severe hepatitis." South Med J, 84, p. 1158
23. Carro PG, Huidobro MLL, Zabala AP, Vicente EM (2000) "Fatal subfulminant hepatic failure with ofloxacin." Am J Gastroenterol, 95, p. 1606
24. Huminer D, Cohen JD, Majadla R, Dux S (1989) "Hypersensitivity vasculitis due to ofloxacin." Br Med J, 299, p. 303
25. Pace JL, Gatt P (1989) "Fatal vasculitis associated with ofloxacin." BMJ, 299, p. 658
26. Baril L, Maisonobe T, JassonMolinier M, Haroche J, Bricaire F, Caumes E (1999) "Acute rhabdomyolysis during treatment with ofloxacin - A case report." Clin Infect Dis, 29, p. 1598-9
27. Khaliq Y, Zhanel GG (2003) "Fluoroquinolone-Associated Tendinopathy: A Critical Review of the Literature." Clin Infect Dis, 36, p. 1404-1410
28. Frothingham R (2001) "Rates of torsades de pointes associated with ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin." Pharmacotherapy, 21, p. 1468-72
29. Owens RC Jr, Ambrose PG (2002) "Torsades de pointes associated with fluoroquinolones." Pharmacotherapy, 22, 663-8; discussion 668-72
30. Berger RE (2005) "Rates of torsades de pointes associated with ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin." J Urol, 174, p. 165
31. Briasoulis A, Agarwal V, Pierce WJ (2011) "QT Prolongation and Torsade de Pointes Induced by Fluoroquinolones: Infrequent Side Effects from Commonly Used Medications." Cardiology, 120, p. 103-110
32. Tsuda S, Kato K, Karashima T, Inou YH, Sasai Y (1993) "Toxic pustuloderma induced by ofloxacin." Acta Derm Venereol, 73, p. 382-4
33. Melde SL (2001) "Ofloxacin: a probable cause of toxic epidermal necrolysis." Ann Pharmacother, 35, p. 1388-90
34. Maunz G, Conzett T, Zimmerli W (2009) "Cutaneous vasculitis associated with fluoroquinolones." Infection, 37, p. 466-8
35. Bharani A, Kumar H (2001) "Diabetes inspidus induced by ofloxacin." BMJ, 323, p. 547
More about Floxin (ofloxacin)
- Check interactions
- Compare alternatives
- Reviews (2)
- Drug images
- Dosage information
- During pregnancy
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
Patient resources
Professional resources
Related treatment guides
Further information
Floxin side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.