Ticagrelor (Monograph)
Brand name: Brilinta
Drug class: Platelet-aggregation Inhibitors
Chemical name: (1S,2S,3R,5S)-3-[7-[[(1R,2S)-2-(3,4-Difluorophenyl)cyclopropyl]amino]-5-(propylthio)-3H-1,2,3-triazolo[4,5-d]pyrimidin-3-yl]-5-(2-hydroxyethoxy)-1,2-cyclopentanediol
Molecular formula: C23H28F2N6O4S
CAS number: 274693-27-5
Warning
- Bleeding
-
Potential risk of bleeding; may be serious, sometimes fatal. (See Bleeding under Cautions.)
-
Avoid use in patients with active pathologic bleeding or history of intracranial hemorrhage. Do not initiate in patients undergoing urgent CABG.
-
If bleeding occurs, attempt to manage without discontinuing ticagrelor; increased risk of subsequent cardiovascular events possible with premature discontinuance. (See Discontinuance of Therapy in Patients with Coronary Artery Disease under Cautions.)
- Reduced Efficacy with Higher Aspirin Dosages in Patients with Acute Coronary Syndrome
-
Avoid use of aspirin maintenance dosages >100 mg daily in patients with acute coronary syndrome (ACS). (See Reduced Response with Higher Aspirin Dosages in Patients with ACS under Cautions.)
Introduction
Platelet-activation and -aggregation inhibitor; nonthienopyridine, reversible, P2Y12 platelet adenosine diphosphate (ADP)-receptor antagonist.
Uses for Ticagrelor
Acute Coronary Syndrome or History of MI
Used in conjunction with aspirin to reduce the risk of cardiovascular death, MI, and stroke in patients with ACS.
Dual antiplatelet therapy (DAPT) with a P2Y12 inhibitor (e.g., clopidogrel, prasugrel, ticagrelor) and aspirin is considered the current standard of care in patients with ACS.
ACC/AHA has issued guidelines for treatment options and duration of DAPT. Aspirin should almost always be continued indefinitely; decisions about specific P2Y12 inhibitor and duration of therapy should be based on risks of bleeding versus benefits of ischemic reduction, clinical judgment, and patient preference.
ACC/AHA generally recommends a shorter duration of DAPT for patients at reduced ischemic, but high bleeding, risk and a longer duration for patients at high ischemic, but reduced bleeding, risk.
In ACS patients managed medically (without revascularization or reperfusion therapy) or with PCI and stent implantation (bare-metal or drug-eluting), P2Y12 inhibitor therapy should be given for at least 12 months; in patients who have tolerated DAPT without bleeding complications and do not have a high risk of bleeding, continuation of such therapy for longer than 12 months may be reasonable.
With regard to the specific P2Y12 inhibitor, evidence supports use of clopidogrel or ticagrelor in medically-managed ACS patients; clopidogrel, prasugrel, or ticagrelor may be used in ACS patients treated with PCI.
In patients undergoing CABG, P2Y12 inhibitor therapy should be resumed after surgery to complete 12 months of therapy.
Unlike clopidogrel, genetic polymorphism of the CYP2C19 isoenzyme does not appear to affect the pharmacodynamic or clinical response to ticagrelor. The Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines recommend ticagrelor as an alternative antiplatelet agent to clopidogrel in patients who are poor or intermediate metabolizers of CYP2C19.
When selecting an appropriate antiplatelet regimen, consider individual patient (e.g., ischemic and bleeding risk) and drug-related (e.g., adverse effects, drug interaction potential) factors.
Also used to reduce the risk of cardiovascular death, MI, and stroke in patients with a history of MI; in the principal study establishing efficacy for this indication, patients had a history of MI 1–3 years prior to study entry.
AHA/ACC states that in patients with stable ischemic heart disease (SIHD) being treated with DAPT for previous (1–3 years prior) MI, continuation of such therapy may be reasonable if tolerated without any bleeding complications.
Coronary Artery Disease but No Prior Stroke or MI
Used to reduce the risk of an initial MI or stroke in patients with established CAD who are at high risk for these thrombotic cardiovascular events.
Use in conjunction with aspirin therapy.
There is evidence supporting use of ticagrelor in reducing risk of a first MI and stroke in patients with CAD and type 2 diabetes mellitus, although treatment effect is small. Reduction in ischemic events is accompanied by increased risk of bleeding.
Acute Ischemic Stroke or Transient Ischemic Attack
Used to reduce the risk of stroke in patients with acute ischemic stroke (National Institutes of Health Stroke Scale [NIHSS] ≤5) or high-risk TIA.
Use in conjunction with aspirin therapy.
Not studied in patients with more severe stroke or cardioembolic stroke; those undergoing thrombectomy or thrombolysis; and those in whom treatment was administered >24 hours after symptom onset.
Ticagrelor Dosage and Administration
Administration
Administer orally without regard to meals.
For patients unable to swallow tablets whole, may crush and mix with water. Also can administer crushed tablet in water mixture via a nasogastric tube (CH8 or greater).
If a dose is missed, take next dose at the regularly scheduled time.
Dosage
Adults
Acute Coronary Syndrome or History of MI
Oral
180-mg loading dose followed by maintenance dosage of 90 mg twice daily during the first year. After first year, maintenance dosage of 60 mg twice daily recommended.
Adjunctive aspirin therapy: Administer maintenance dosage of 75–100 mg daily. (See Reduced Response with Higher Aspirin Dosages in Patients with ACS under Cautions.)
Manufacturer makes no specific recommendation regarding duration of maintenance therapy; however, ticagrelor was administered for up to 12 months in the pivotal efficacy study (PLATO). Recommendations for duration of dual antiplatelet therapy can be found in ACC/AHA guidelines. (See Acute Coronary Syndrome or History of MI under Uses.)
Coronary Artery Disease but No Prior Stroke or MI
Oral
60 mg twice daily.
Adjunctive aspirin therapy: Administer maintenance dosage of 75–100 mg daily.
Acute Ischemic Stroke or Transient Ischemic Attack
Oral
180-mg loading dose followed by maintenance dosage of 90 mg twice daily for up to 30 days.
Adjunctive aspirin therapy: After initial loading dose (300–325 mg), administer maintenance dosage of 75–100 mg daily.
Transitioning from Clopidogrel to Ticagrelor Therapy
Oral
May transition patients directly from clopidogrel to ticagrelor therapy without interruption in antiplatelet effects. In clinical trials, patients who switched from clopidogrel to ticagrelor received an initial loading dose of ticagrelor regardless of whether a previous loading dose of clopidogrel had been given.
Special Populations
Renal Impairment
No dosage adjustment required in patients with renal impairment.
Hepatic Impairment
No dosage adjustment required in patients with mild hepatic impairment (Child-Pugh class A). (See Hepatic Impairment under Cautions.)
Geriatric Patients
Dosage adjustment based on age not required.
Cautions for Ticagrelor
Contraindications
-
History of intracranial hemorrhage.
-
Active pathologic bleeding (e.g., peptic ulcer, intracranial hemorrhage).
-
Hypersensitivity to the drug or any components.
Warnings/Precautions
Warnings
Bleeding
Risk of bleeding, including serious, sometimes fatal bleeding. (See Boxed Warning.)
Overall risk of major and minor bleeding somewhat greater with ticagrelor than with clopidogrel in the PLATO trial. Increased risk principally involved non-CABG-related major bleeding, including fatal intracranial hemorrhage. Rates of major CABG-related bleeding were similar between ticagrelor and clopidogrel.
Bleeding was reported more frequently with ticagrelor compared with placebo in other preapproval studies.
In general, risk factors for bleeding include advanced age, history of bleeding disorders, female gender, renal dysfunction, performance of PCI, and concurrent use of other drugs that affect hemostasis (e.g., anticoagulants, thrombolytic agents, high dosages of aspirin, long-term use of NSAIAs).
Contraindicated in patients who are actively bleeding or who have a history of intracranial hemorrhage. Also not recommended in patients likely to undergo urgent CABG. Temporarily discontinue drug at least 5 days prior to surgery (e.g., CABG) whenever possible.
If possible, manage bleeding without discontinuing ticagrelor; premature discontinuance may increase risk of subsequent cardiovascular events. (See Discontinuance of Therapy in Patients with Coronary Artery Disease under Cautions.)
Reduced Response with Higher Aspirin Dosages in Patients with ACS
In the PLATO study, a reduced response to ticagrelor was observed when used with aspirin maintenance dosages >100 mg daily in patients with ACS. Avoid aspirin dosages >100 mg daily. (See Boxed Warning.)
Other Warnings and Precautions
Dyspnea
Risk of dyspnea, generally mild to moderate and self-limiting. Adverse effects on pulmonary function not observed. Mechanism of dyspnea unknown, but thought to be related to an adenosine-mediated response.
If any new, prolonged, or worsening dyspnea related to ticagrelor occurs, no specific treatment required; may continue therapy without interruption if possible. If dyspnea is intolerable and results in discontinuance of ticagrelor, consider another antiplatelet agent.
Discontinuance of Therapy in Patients with Coronary Artery Disease
In general, avoid premature discontinuance of antiplatelet therapy (e.g., P2Y12-receptor antagonists, aspirin) in patients with CAD because of subsequent increased risk of ischemic complications. Stent thrombosis, MI, and/or death observed in patients with coronary stents who prematurely discontinued antiplatelet therapy.
If temporary discontinuance of ticagrelor required (e.g., prior to significant surgery or for bleeding), reinstitute therapy as soon as possible. Interrupt therapy for 5 days prior to surgical procedures with a major bleeding risk if possible; resume therapy when hemostasis is achieved.
Bradyarrhythmias
Ventricular pauses ≥3 seconds, usually occurring during first week of therapy, reported. Mostly asymptomatic and not associated with any clinically important effects (e.g., syncope, need for pacemaker insertion).
Because patients with baseline increased risk of bradycardia (e.g., those with sick sinus syndrome, second- or third-degree AV block, or syncope due to bradycardia without a pacemaker) were excluded from clinical studies, some clinicians recommend caution when used in such patients.
Laboratory Test Interference
May cause false negative results in platelet function tests for heparin-induced thrombocytopenia (e.g., heparin-induced platelet aggregation [HIPA] assay). However, not expected to affect PF4 antibody testing for heparin-induced thrombocytopenia.
Specific Populations
Pregnancy
No drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes identified.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Breast-feeding not recommended during ticagrelor therapy.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
No overall differences in efficacy or safety between geriatric and younger patients.
Ticagrelor pharmacokinetics not substantially affected by age.
Hepatic Impairment
Possible increased exposure and risk of bleeding. (See Absorption: Special Populations under Pharmacokinetics.)
Avoid use in patients with severe hepatic impairment. Carefully consider use in those with moderate hepatic impairment after weighing risks versus benefits. May be used in patients with mild hepatic impairment without dosage adjustment.
Renal Impairment
Pharmacokinetics and clinical efficacy not substantially altered in patients with renal impairment. (See Renal Impairment under Dosage and Administration.)
Not studied in patients with end-stage renal disease (ESRD) on dialysis; however, clinically important differences not expected in such patients receiving intermittent hemodialysis.
Ticagrelor is not dialyzable.
Common Adverse Effects
Bleeding, dyspnea.
Drug Interactions
Metabolized principally by CYP isoenzyme 3A4. Weak inhibitor of CYP3A4/5 and potential activator of CYP3A5. Does not inhibit CYP 1A2, 2C19, or 2E1.
P-glycoprotein substrate and inhibitor.
Drugs Affecting Hemostasis
Possible increased risk of bleeding. (See Bleeding under Cautions and see Specific Drugs under Interactions.)
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Potent CYP3A inhibitors: Potential pharmacokinetic interaction (substantially increased exposure to ticagrelor); possible increased risk of bleeding. Avoid concomitant use.
Moderate CYP3A inhibitors: Possible increased ticagrelor exposure; dosage adjustment not necessary.
Potent CYP3A inducers: Potential pharmacokinetic interaction (substantially decreased plasma ticagrelor concentrations); possible reduced efficacy. Avoid concomitant use.
CYP3A substrates: Potential pharmacokinetic interaction (increased plasma concentrations of substrate drug).
Drugs Affecting or Affected by P-glycoprotein Transport
P-glycoprotein substrates: Potential pharmacokinetic interaction (increased plasma concentrations of substrate drug).
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticoagulants |
Possible increased risk of bleeding |
|
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Substantially reduced plasma ticagrelor concentrations due to CYP3A induction |
Avoid concomitant use |
|
Antifungals, azole (itraconazole, ketoconazole, voriconazole) |
Substantially increased exposure to ticagrelor due to potent CYP3A inhibition |
Avoid concomitant use |
|
Aspirin |
Possible reduced efficacy of ticagrelor when used with aspirin dosages >100 mg daily Increased risk of bleeding possible with high dosages of aspirin Pharmacokinetics of ticagrelor not altered |
Limit concomitant aspirin maintenance dosage to 75–100 mg daily |
|
Atazanavir |
Substantially increased exposure to ticagrelor due to potent CYP3A inhibition |
Avoid concomitant use |
|
Clarithromycin |
Substantially increased exposure to ticagrelor due to potent CYP3A inhibition |
Avoid concomitant use |
|
Cyclosporine |
Possible increased exposure to ticagrelor |
|
|
Desmopressin |
Pharmacokinetics of ticagrelor not affected |
No dosage adjustment necessary |
|
Digoxin |
Pharmacokinetics of digoxin not substantially altered |
No dosage adjustment necessary; monitor serum digoxin concentrations prior to and following any change in ticagrelor therapy |
|
Diltiazem |
Possible decreased exposure to ticagrelor due to moderate CYP3A inhibition |
No dosage adjustment necessary |
|
Enoxaparin |
Pharmacokinetics of ticagrelor not affected Possible increased risk of bleeding |
No dosage adjustment necessary |
|
Heparin |
Pharmacokinetics of ticagrelor not affected Possible increased risk of bleeding |
No dosage adjustment necessary |
|
HMG-CoA reductase inhibitors (statins) |
Lovastatin, simvastatin: Possible increased serum concentrations of the statin Atorvastatin: Pharmacokinetics of atorvastatin not substantially altered |
Lovastatin, simvastatin: Do not exceed dosage of 40 mg daily Atorvastatin: No dosage adjustment necessary |
|
Hormonal contraceptives (ethinyl estradiol/levonorgestrel) |
Increased peak plasma concentrations of and systemic exposure to ethinyl estradiol; pharmacokinetics of levonorgestrel not altered Ticagrelor not expected to affect contraceptive efficacy |
No dosage adjustment necessary |
|
Nefazodone |
Substantially increased exposure to ticagrelor due to potent CYP3A inhibition |
Avoid concomitant use |
|
Nelfinavir |
Substantially increased exposure to ticagrelor due to potent CYP3A inhibition |
Avoid concomitant use |
|
NSAIAs |
Possible increased risk of bleeding with chronic NSAIA use |
|
|
Opiate agonists (e.g., morphine) |
May delay and reduce absorption of ticagrelor and its active metabolite Ticagrelor exposure was decreased and time to peak plasma concentration was delayed when coadministered with IV fentanyl or IV morphine; platelet aggregation was higher up to 3 hours post-loading dose in ACS patients who received these drugs concomitantly |
Consider use of a parenteral antiplatelet agent in ACS patients who require treatment with morphine or other opiate agonist |
|
Proton-pump inhibitors |
Platelet response to ticagrelor not affected |
May be used concomitantly |
|
Rifampin |
Substantially decreased peak plasma concentrations of and systemic exposure to ticagrelor due to potent CYP3A induction |
Avoid concomitant use |
|
Ritonavir |
Substantially increased exposure to ticagrelor due to potent CYP3A inhibition |
Avoid concomitant use |
|
Saquinavir |
Substantially increased exposure to ticagrelor due to potent CYP3A inhibition |
Avoid concomitant use |
|
Thrombolytics |
Possible increased risk of bleeding |
|
|
Tolbutamide |
Pharmacokinetics of tolbutamide not substantially altered |
Dosage adjustment not necessary |
Ticagrelor Pharmacokinetics
Absorption
Bioavailability
Rapidly but incompletely absorbed after oral administration; mean absolute oral bioavailability about 36%.
Plasma concentrations of ticagrelor and its major metabolite increase in a dose-dependent manner; peak concentrations achieved within approximately 1.5 and 2.5 hours, respectively.
Onset
Maximum inhibition of platelet aggregation observed approximately 2 hours after a dose.
Additional inhibition of platelet aggregation (absolute increase of 26.4%) observed in patients who transition from clopidogrel to ticagrelor therapy.
Duration
Maximum inhibition of platelet aggregation maintained for ≥8 hours after a dose. Following discontinuance, platelet activity returns to baseline after 5 days.
Food
High-fat meal increased systemic exposure to ticagrelor by 21% and decreased peak plasma concentrations of the active metabolite by 22%; no effect on plasma concentrations of ticagrelor or systemic exposure to active metabolite.
Special Populations
Individuals with mild (Child-Pugh class A) hepatic impairment had slightly higher systemic exposure to ticagrelor than those with normal hepatic function; however, no clinically important effects observed.
Individuals with severe (Clcr <30 mL/minute) renal impairment had slightly higher systemic exposure to ticagrelor than those with normal renal function; however, no effect on platelet inhibition or tolerability.
Distribution
Plasma Protein Binding
>99% for both ticagrelor and active metabolite.
Elimination
Metabolism
Metabolized principally by CYP3A4 to active metabolite.
Elimination Route
Primarily eliminated in feces; <1% of a dose is recovered in urine (as parent drug and active metabolite).
Half-life
Ticagrelor: Approximately 7 hours.
Active metabolite: Approximately 9 hours.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).
Actions
-
Nonthienopyridine P2Y12 platelet ADP-receptor antagonist; unlike thienopyridines (e.g., clopidogrel, prasugrel), ticagrelor binds reversibly to P2Y12 receptor and does not require hepatic transformation to exerts its pharmacologic effect.
-
Prevents signal transduction of the cyclic adenosine monophosphate (cAMP) pathway, resulting in reduced exposure of fibrinogen binding sites to the platelet glycoprotein (GP IIb/IIIa) complex and subsequent inhibition of platelet activation and aggregation.
-
Inhibits reuptake of adenosine into erythrocytes.
-
Compared with clopidogrel, ticagrelor produces more rapid and effective inhibition of platelet aggregation and has a faster offset of action. However, relationship between inhibition of platelet aggregation and clinical outcomes of either drug not known.
-
Pharmacogenomics: Genetic polymorphism of the CYP2C19 isoenzyme does not appear to affect pharmacodynamic or clinical response to ticagrelor.
Advice to Patients
-
Importance of patients reading the FDA-approved patient labeling (medication guide).
-
Importance of patients informing clinicians (e.g., physicians, dentists) about ticagrelor therapy before any surgery or dental procedure is performed.
-
Importance of informing patients not to take aspirin dosages exceeding 100 mg daily; advise patients to not take any other aspirin-containing drugs.
-
Importance of informing patients that they will bruise and/or bleed more easily and that a longer than usual time will be required to stop bleeding when taking ticagrelor. Importance of patients informing clinicians about any unexpected, prolonged, or excessive bleeding, or blood in urine or stool.
-
Importance of informing patients that ticagrelor can cause dyspnea; advise patient to contact their clinician if they experience any unexpected shortness of breath.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, particularly drugs that affect bleeding risk (e.g., heparin, warfarin).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
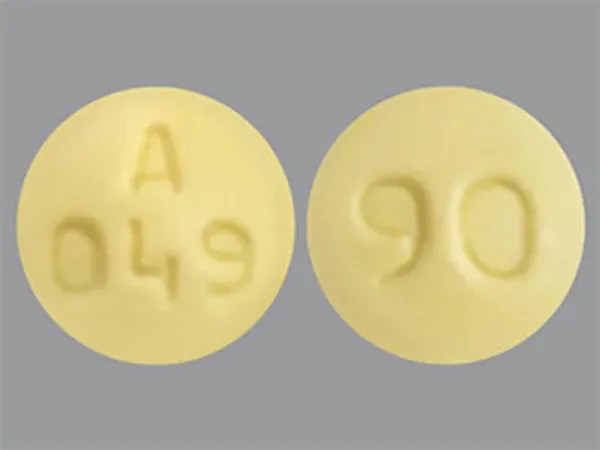
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
60 mg |
Brilinta |
AstraZeneca |
|
90 mg* |
Brilinta |
AstraZeneca |
||
|
Ticagrelor Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 4, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- How long do I take Brilinta after a stent or heart attack?
- What pain medication can I take with Brilinta?
- How long should Brilinta be held/stopped before surgery?
- Brilinta vs Plavix: what's the difference?
- Is there a generic for Brilinta?
- Is ticagrelor better than clopidogrel?
- What is Brilinta (ticagrelor) used for?
- Is ticagrelor a prodrug?
More about ticagrelor
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (117)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: platelet aggregation inhibitors
- Breastfeeding
- En español