Mercaptopurine (Monograph)
Brand names: Purinethol, Purixan
Drug class: Antineoplastic Agents
Warning
On 4/29/24, FDA alerted healthcare professionals of the rare risk of intrahepatic cholestasis of pregnancy (ICP) associated with the use of thiopurines (azathioprine, 6-mercaptopurine, and 6-thioguanine). Reported cases of ICP occurred among pregnant patients using azathioprine or 6-mercaptopurine primarily to treat inflammatory bowel disease (IBD), including Crohn's disease (CD) and ulcerative colitis (UC), or systemic lupus erythematosus (SLE). Thiopurines are not FDA-approved to treat these conditions; however, the American Gastroenterological Association and the American College of Rheumatology have published guidelines indicating that these drugs may be appropriate to continue on an individualized basis for the management of some immunologic conditions during pregnancy. Pregnant patients should stop using thiopurines if they develop ICP. FDA is requiring manufacturers to update labeling to include additional warning information on the risk of ICP associated with thiopurines. For additional information, see [Web]
Introduction
Antineoplastic and immunosuppressive agent; purine antagonist.
Uses for Mercaptopurine
Acute Lymphoblastic Leukemia (ALL)
Treatment of adults and pediatric patients with ALL as maintenance therapy in combination with other drugs.
Crohn Disease
Has been used for management of moderate to severe or chronically active Crohn disease† [off-label].
The American Gastroenterological Association (AGA) and American College of Gastroenterology (ACG) guidelines state that thiopurines are generally used for maintenance of remission or in combination with other therapies (e.g., tumor necrosis factor [TNF] blocking agents) for induction and maintenance of remission in patients with moderate to severe Crohn disease.
Ulcerative Colitis
Has been used in the management of ulcerative colitis† [off-label].
AGA guideline suggests the use of thiopurine monotherapy for maintenance of remission in patients with moderate to severe ulcerative colitis; thiopurines also may be used in combination with TNF blocking agents, vedolizumab, or ustekinumab for remission induction.
Mercaptopurine Dosage and Administration
General
Pretreatment Screening
-
Consider genetic testing (i.e., TPMT and NUDT15) or use of previous testing results to guide dosing recommendations.
-
Verify pregnancy status in females of reproductive potential.
Patient Monitoring
-
Monitor CBC and adjust dose to maintain ANC at desired level and avoid excessive myelosuppression.
-
Monitor serum transaminase, alkaline phosphatase, and bilirubin at weekly intervals when first beginning therapy and at monthly intervals thereafter. Monitor liver tests more frequently in patients receiving other hepatotoxic drugs or those with pre-existing liver disease.
-
Monitor for lymphoproliferative disorders and other malignancies such as skin cancers (melanoma and non-melanoma), sarcomas (Kaposi's and non- Kaposi's), and uterine cervical cancer in situ.
-
Monitor for the development of Epstein-Barr virus (EBV) and cytomegalovirus (CMV) infection.
Dispensing and Administration Precautions
-
Handling and Disposal: Mercaptopurine is a cytotoxic drug; consult specialized references for procedures for proper handling and disposal.
-
Based on the Institute for Safe Medication Practices (ISMP), mercaptopurine is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.
Administration
Oral Administration
Administer orally as tablets or oral suspension. Take consistently, either with or without food.
Do not administer tablets to patients who are unable to swallow tablets; use the oral suspension in these patients.
Shake the oral suspension for at least 30 seconds to mix. Use oral dispensing syringes to measure and dispense the dose. Use the suspension within 8 weeks; properly discard any remaining suspension after that time.
If a dose is missed, skip the dose and continue therapy with the next dose.
Pharmacogenomic Testing
Pharmacogenomic testing for thiopurine S-methyltransferase (TPMT) and nucleotide diphosphatase (NUDT15) may be useful for identifying patients at increased risk for life-threatening myelosuppression, or evaluating those with severe myelosuppression or repeated episodes of myelosuppression during treatment. Patients with specific variants of TPMT and NUDT15 are likely to have increased systemic exposure to mercaptopurine and are at increased risk of myelosuppression.
Dosage
Pediatric Patients
Acute Lymphoblastic Leukemia (ALL)
Maintenance Therapy
OralUsually, 1.5–2.5 mg/kg once daily as part of a combination chemotherapy regimen.
Adults
ALL
Maintenance Therapy
OralUsually 1.5–2.5 mg/kg once daily as part of a combination chemotherapy regimen.
Crohn Disease† [off-label]
Oral
Maximal dosage of 0.75–1.5 mg/kg daily.
Dosage Modifications in Patients with TPMT and NUDT15 Deficiency
TPMT intermediate or TPMT possible intermediate metabolizer: Start with reduced doses of mercaptopurine (30-80% of normal dose) if starting dose is ≥75 mg/m2/day or ≥1.5 mg/kg/day (e.g., start at 22.5-60 mg/m2/day or 0.45-1.2 mg/kg/day) and adjust doses based on degree of myelosuppression and disease specific guidelines. Allow 2–4 weeks to reach steady state after each dosage adjustment. If myelosuppression occurs, emphasis should be on reducing mercaptopurine over other agents, dependent on concomitant therapy. If normal starting dose is <75 mg/m2/day or <1.5 mg/kg/day, dose reduction may not be recommended.
TPMT poor metabolizer: For malignancy, start with drastically reduced doses of mercaptopurine (reduce daily dose by 10-fold and reduce frequency to three times weekly instead of daily (e.g., 10 mg/m2/day given just 3 days/week) and adjust doses based on degree of myelosuppression and disease specific guidelines. Allow 4–6 weeks to reach steady state after each dosage adjustment. If myelosuppression occurs, emphasis should be on reducing mercaptopurine over other agents. For non-malignant conditions, consider alternative non-thiopurine immunosuppressant therapy.
NUDT15 intermediate or NUDT15 possible intermediate metabolizer: Start with reduced mercaptopurine doses (30−80% of normal dose) if normal starting dose is ≥75 mg/m2/day or ≥1.5 mg/kg/day (e.g., start at 22.5–60 mg/m2/day or 0.45–1.2 mg/kg/day) and adjust doses based on degree of myelosuppression and disease-specific guidelines. Allow 2–4 weeks to reach steady state after each dosage adjustment. If myelosuppression occurs, emphasis should be on reducing mercaptopurine over other agents, depending on other therapy. If normal starting dose is <75 mg/m2/day or <1.5 mg/kg/day, dose reduction may not be recommended.
NUDT15 poor metabolizer: For malignancy, initiate mercaptopurine at 10 mg/m2/day and adjust dose based on myelosuppression and disease-specific guidelines. Allow 4–6 weeks to reach steady state after each dosage adjustment. If myelosuppression occurs, emphasis should be on reducing mercaptopurine over other agents. For non-malignant conditions, consider alternative nonthiopurine immunosuppressant therapy.
Special Populations
Hepatic Impairment
Use lowest recommended starting dosage. Adjust dosage to maintain ANC at a desirable level and for management of adverse reactions.
Renal Impairment
Use lowest recommended starting dosage in patients with renal impairment (Clcr <50 mL/minute). Adjust dosage to maintain ANC at a desirable level and for management of adverse reactions.
Geriatric Use
Select dosage with caution, usually starting at the low end of the dosing range.
Cautions for Mercaptopurine
Contraindications
-
None.
Warnings/Precautions
Warnings
Myelosuppression
Most consistent, dose-related adverse reaction is myelosuppression, manifested by anemia, leukopenia, thrombocytopenia, or any combination of these effects.
Individuals who are homozygous deficient (2 nonfunctional alleles; poor metabolizer) for an inherited defect in theTPMT gene are unusually sensitive to myelosuppressive effects of mercaptopurine and prone to rapid bone marrow suppression. Substantial dosage reductions generally are required in such patients to avoid life-threatening suppression. Tolerance may vary in individuals who are heterozygous deficient (one nonfunctional allele; intermediate metabolizer) for the defect in theTPMT gene. Although some of these patients may experience greater toxicity, most will tolerate usual doses.
Monitor CBC and adjust dosage for excessive myelosuppression. Consider testing for TPMT or NUDT15 deficiency in patients with severe myelosuppression or repeated episodes of myelosuppression. Patients with heterozygous or homozygous TPMT or NUDT15 deficiency may require dose reduction.
Concomitant use of allopurinol may exacerbate myelotoxicity. Reduction of mercaptopurine dosage is required.
Hepatotoxicity
Mercaptopurine is hepatotoxic; may be associated in some cases with anorexia, diarrhea, jaundice, and ascites. Hepatic encephalopathy and deaths attributed to hepatic necrosis reported.
Hepatic injury occurs with any dosage, but may occur with greater frequency when recommended dosage exceeded.
Clinically detectable jaundice usually appears early in treatment (1 to 2 months); however, it has been reported at 1 week and as late as 8 years after starting mercaptopurine. In some patients, jaundice resolved following withdrawal, but reappeared with rechallenge.
Monitor serum transaminase levels, alkaline phosphatase, and bilirubin levels at weekly intervals when beginning therapy and at monthly intervals thereafter. Monitor liver tests more frequently in patients receiving mercaptopurine with other hepatotoxic drugs or those with pre-existing liver disease. Withhold mercaptopurine at onset of hepatotoxicity.
Immunosuppression
May impair immune response to infectious agents or vaccines. Due to immunosuppression associated with maintenance chemotherapy for ALL, response to all vaccines may be diminished and there is a risk of infection with live virus vaccines.
Consult immunization guidelines for recommendations regarding immunocompromised patients.
Treatment-related Malignancies
May increase risk of neoplasia. Monitor for occurrence of malignancies.
Hepatosplenic T-cell lymphoma, a rare, aggressive, usually fatal malignancy, reported in mercaptopurine-treated patients with inflammatory bowel disease (IBD)† [off-label].
Patients receiving immunosuppressive therapy, including mercaptopurine, are at an increased risk of developing lymphoproliferative disorders and other malignancies, notably skin cancers (melanoma and non-melanoma), sarcomas (Kaposi's and non- Kaposi's) and uterine cervical cancer in situ.
Risk appears to be related to degree and duration of immunosuppression. Discontinuation of immunosuppression may provide partial regression of the lymphoproliferative disorder. Treatment regimens containing multiple immunosuppressants (including thiopurines) should be used with caution as this could lead to potentially fatal lymphoproliferative disorders. A combination of concomitantly administered multiple immunosuppressants increases risk of Epstein-Barr virus (EBV)-associated lymphoproliferative disorders.
Macrophage Activation Syndrome
Macrophage activation syndrome (MAS; hemophagocytic lymphohistiocytosis) may develop in patients with autoimmune conditions, in particular those with IBD† [off-label] . Patients receiving mercaptopurine may have increased susceptibility for this condition.
Discontinue mercaptopurine if MAS occurs or is suspected.
Monitor for and promptly treat infections such as EBV and CMV, as these are known triggers for MAS.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. Women who receive mercaptopurine during the first trimester have increased incidence of miscarriage. Miscarriage and stillbirth reported in women who receive mercaptopurine after first trimester of pregnancy.
Specific Populations
Pregnancy
Can cause fetal harm. Increased incidence of miscarriage and stillbirth. Advise pregnant women of the potential risk to a fetus.
Lactation
No data on presence of mercaptopurine or its metabolites in human milk, effects on the breastfed child, or effects on milk production.
Advise women not to breastfeed during treatment with mercaptopurine and for 1 week after final dose
Females and Males of Reproductive Potential
Can cause fetal harm when administered to pregnant women.
Verify pregnancy status in females of reproductive potential prior to initiating mercaptopurine.
Advise females of reproductive potential to use effective contraception during treatment and for 6 months after final dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with mercaptopurine and for 3 months after final dose.
Based on findings from animal studies, can impair female and male fertility. Long-term effects, including reversibility, not studied.
Pediatric Use
Safety and effectiveness not established, but use is supported by evidence from published literature and clinical experience.
Symptomatic hypoglycemia reported in pediatric patients with ALL. Reported cases were in children <6 yearsof age or those with a low BMI.
Geriatric Use
Insufficient numbers of patients ≥65 years of age to determine whether they respond differently from younger patients. Other clinical experience has not identified differences in responses between elderly and younger patients.
Common Adverse Effects
ALL
Common adverse effects (>20%): myelosuppression, including anemia, neutropenia, lymphopenia, thrombocytopenia.
Common adverse effects (5–20%): anorexia, nausea, vomiting, diarrhea, malaise, rash.
Drug Interactions
Myelosuppressive Drugs
Possible increased risk of myelosuppression; consider reducing mercaptopurine dosage if used concomitantly. Monitor CBC and adjust dose for excessive myelosuppression.
Hepatotoxic Drugs
Possible increased risk of hepatotoxicity; use concomitantly with caution and monitor hepatic function closely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Allopurinol |
Possible decreased mercaptopurine metabolism and increased risk of myelotoxicity |
Reduce mercaptopurine dosage to 25–33% of usual dosage |
|
Aminosalicylates (mesalamine, olsalazine, sulfasalazine) |
Possible decreased mercaptopurine metabolism and increased risk of myelotoxicity |
Use concomitantly with caution. Use lowest possible doses for each drug and monitor more frequently for myelosuppression |
|
Drugs affecting myelopoiesis (e.g., trimethoprim-sulfamethoxazole) |
Possible increased myelosuppression |
Monitor CBC; adjust dose of mercaptopurine for excessive myelosuppression |
|
Warfarin |
Possible inhibition of anticoagulant effect |
Monitor INR and adjust dosage as appropriate. |
Mercaptopurine Pharmacokinetics
Absorption
Bioavailability
Food may decrease exposure of mercaptopurine.
Distribution
Extent
Only negligible concentrations attained in CSF.
Not known whether mercaptopurine is distributed into human milk.
Plasma Protein Binding
Approximately 19%.
Elimination
Metabolism
Rapidly and extensively metabolized in liver by oxidation via xanthine oxidase to 6-thiouric acid. Also undergoes thiol methylation via the enzyme TPMT to form inactive metabolite, methyl-6-MP.
Elimination Route
Excreted principally in urine (about 46%) as unchanged drug and metabolites within first 24 hours.
Half-life
<2 hours after single oral dose.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted to 15-30ºC).
Suspension
15–25°C.
Actions
-
Nucleoside metabolic inhibitor.
-
Converted intracellularly to ribonucleotides that result in a sequential blockade of the synthesis and utilization of purine nucleotides.
-
Inhibits synthesis of RNA and DNA.
-
Also an immunosuppressant that inhibits primary immune response.
Advice to Patients
-
Advise patients and caregivers that mercaptopurine can cause myelosuppression, hepatotoxicity, and GI toxicity. Advise patients to contact their healthcare provider if they experience fever, sore throat, jaundice, nausea, vomiting, signs of local infection, bleeding from any site, or symptoms suggestive of anemia.
-
Instruct patients to minimize sun exposure due to risk of photosensitivity.
-
Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy. Advise females of reproductive potential to use effective contraception during treatment with mercaptopurine and for 6 months after the final dose. Advise males with female partners of reproductive potential to use effective contraception during treatment with mercaptopurine and for 3 months after the final dose.
-
Advise males and females of reproductive potential that mercaptopurine can impair fertility.
-
Advise women not to breastfeed during treatment with mercaptopurine and for 1 week after the final dose.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription (e.g., allopurinol) or OTC drugs, as well as concomitant illnesses.
-
Inform patients of other important precautionary information
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
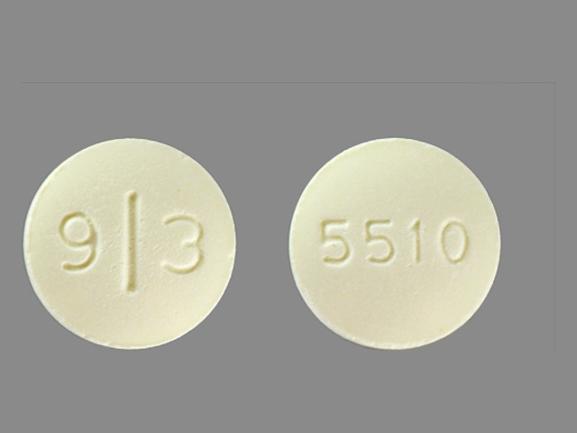
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
50 mg* |
Mercaptopurine Tablets |
|
|
Purinethol (scored) |
Stason Pharmaceuticals |
|||
|
Suspension |
20 mg/mL |
Purixan |
Nova Laboratories |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Gleevec
Gleevec is targeted cancer therapy for specific types of leukemia (blood cancer), bone marrow ...
Sprycel
Sprycel is used to treat chronic myeloid leukemia and acute lymphoblastic leukemia. Learn about ...
Entyvio
Entyvio (vedolizumab) is used to treat ulcerative colitis (UC) and Crohn's disease, reducing ...
Adriamycin
Adriamycin is used for acute lymphoblastic leukemia, acute myeloblastic leukemia, bladder cancer ...
Rasuvo
Rasuvo is used for polyarticular juvenile idiopathic arthritis, psoriasis, rheumatoid arthritis
Ponatinib
Ponatinib is used to treat chronic myeloid leukemia and Philadelphia chromosome positive acute ...
Blinatumomab
Blinatumomab (Blincyto) is an injectable immunotherapy treatment that may be used to treat B-cell ...
Dasatinib
Dasatinib is used to treat Philadelphia chromosome-positive chronic myelogenous leukemia (CML) ...
Imatinib
Imatinib is used to treat certain types of leukemia, bone marrow disorders, and skin cancer ...
Doxorubicin
Doxorubicin is used for acute lymphoblastic leukemia, acute myeloblastic leukemia, bladder cancer ...
More about mercaptopurine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (32)
- Drug images
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimetabolites
- Breastfeeding
- En español