Felbamate (Monograph)
Brand name: Felbatol
Drug class: Anticonvulsants, Miscellaneous
VA class: CN400
Chemical name: 2-Phenyltrimethylene ester carbamic acid
Molecular formula: C11H14N2O4
CAS number: 25451-15-4
Warning
- Aplastic Anemia
-
Risk of aplastic anemia in patients receiving felbamate may be more than 100 times higher than risk in general population (about 2–5 cases per million untreated individuals per year).
-
Potentially fatal; current estimated case fatality rate for untreated individuals ranges from 20–30%, but rates as high as 70% have been reported.
-
Limit use to patients whose seizure disorder is so severe that the benefits of therapy outweigh the substantial risk of aplastic anemia. (See Seizure Disorders under Uses.)
-
Clinical manifestations of aplastic anemia (e.g., bleeding, infection) may develop without premonitory clinical or laboratory signs after several months of therapy (range: 5–30 weeks). Routine blood tests are unreliable but may, nevertheless, result in early detection of the syndrome in some patients. (See Hematologic Effects under Cautions.)
- Hepatic Failure
-
Risk of acute hepatic failure resulting in death or hepatic transplantation reported at an estimated rate of about 6 cases per 75,000 patient years of use. Actual rate believed to be considerably higher.
-
Severe hepatic dysfunction followed by hepatic failure reported as early as 3 weeks after initiation of felbamate; has resulted in death or hepatic transplantation in about 67% of reported cases, usually within 5 weeks of the onset of signs and symptoms of hepatic failure. Prodromal symptoms (e.g., anorexia, malaise, other GI symptoms) and/or dark urine may or may not precede onset of jaundice.
-
Do not initiate therapy in patients with active liver disease, abnormal baseline serum transaminase concentrations, or a history of hepatic dysfunction.
-
Periodic serum transaminase testing has not been proven to prevent serious injury but may, nevertheless, result in early detection of the syndrome in some patients. (See Hepatic Effects under Cautions.)
Introduction
Anticonvulsant; a dicarbamate derivative.
Uses for Felbamate
Seizure Disorders
Not indicated as a first-line antiepileptic therapy; use only in patients whose seizure disorder is refractory to alternative safer therapy and is so severe that the benefits of felbamate therapy are believed to outweigh the substantial risk of aplastic anemia or acute hepatic failure. (See Boxed Warning.)
Management (alone or in combination with other anticonvulsants) of partial seizures with or without secondary generalization in adults and adolescents ≥14 years of age.
Management (in combination with other anticonvulsants) of partial and generalized seizures associated with Lennox-Gastaut syndrome in children 2–14 years of age (designated an orphan drug by FDA for this use).
Felbamate Dosage and Administration
General
-
Prior to initiation of therapy, discuss the risks associated with use of felbamate with the patient, parent, or guardian and obtain written patient/physician acknowledgment form.
-
Obtain expert hematologic consultation prior to initiation of therapy and whenever any hematologic abnormality is detected during the course of therapy.
-
Closely monitor for notable changes in behavior that could indicate emergence or worsening of suicidal thoughts or behavior or depression. (See Suicidality Risk under Cautions.)
-
Abrupt withdrawal may result in increased seizure frequency; withdraw gradually and reduce dosage slowly. (See Discontinuance of Therapy under Cautions.)
Administration
Oral Administration
Tablets
Administer orally in 3 or 4 divided doses; food does not appear to affect absorption of the tablet.
Suspension
Administer orally in 3 or 4 divided doses; effect of food on absorption of the suspension not evaluated. Shake well before administration.
Dosage
When adding to an existing anticonvulsant regimen, add gradually while reducing dosage(s) of other anticonvulsant(s). (See Specific Drugs under Interactions.)
Pediatric Patients
Lennox-Gastaut Syndrome
Adjunctive Therapy
OralChildren 2–14 years of age: Initially, 15 mg/kg daily administered in 3 or 4 divided doses. Dosage may be increased by 15 mg/kg daily at weekly intervals to 45 mg/kg daily administered in 3 or 4 divided doses.
As felbamate is added to existing anticonvulsants (e.g., phenytoin, valproic acid, phenobarbital, carbamazepine), dosage(s) of other anticonvulsant(s) must be gradually decreased, initially by at least 20%; further reductions in dosage(s) of concomitant anticonvulsant(s) may be necessary as felbamate dosage is increased to avoid adverse effects caused by drug interactions.
Partial Seizures With or Without Secondary Generalization
Oral
Adolescents ≥14 years of age should receive dosages recommended for adults. (See Adults under Dosage and Administration.)
Adults
Partial Seizures With or Without Secondary Generalization
Monotherapy
OralInitially, 1.2 g daily administered in 3 or 4 divided doses. Titrate previously untreated patients under close clinical supervision, increasing dosage in 600-mg daily increments every 2 weeks to 2.4 g daily based on clinical response and thereafter to 3.6 g daily if clinically indicated. Felbamate has not been evaluated systematically as initial monotherapy.
The majority of patients in monotherapy trials received a felbamate dosage of 3.6 g daily.
Conversion to Felbamate Monotherapy
OralInitially, 1.2 g daily administered in 3 or 4 divided doses. At the same time, reduce the dosage(s) of concomitantly administered anticonvulsant(s) by 33%. At week 2, increase the felbamate dosage to 2.4 g daily while reducing the dosage(s) of other anticonvulsant(s) by up to an additional 33% of their baseline dosage(s). At week 3, increase the felbamate dosage to 3.6 g daily and continue to reduce the dosage(s) of other anticonvulsant(s) as clinically indicated.
The majority of patients in monotherapy trials received a felbamate dosage of 3.6 g daily.
Adjunctive Therapy
OralInitially, 1.2 g daily administered in 3 or 4 divided doses. Dosage may be increased by 1.2-g daily increments at weekly intervals to 3.6 g daily administered in 3 or 4 divided doses.
As felbamate is added to existing anticonvulsants (e.g., phenytoin, valproic acid, phenobarbital, carbamazepine), dosage(s) of other anticonvulsant(s) must be gradually decreased, initially by at least 20%; further reductions in dosage(s) of concomitant anticonvulsant(s) may be necessary as felbamate dosage is increased to avoid adverse effects caused by drug interactions.
The majority of patients in adjunctive therapy trials received a felbamate dosage of 3.6 g daily.
Special Populations
Hepatic Impairment
Do not use in patients with hepatic impairment. (See Boxed Warning.)
Renal Impairment
Reduce initial and maintenance dosages by 50%. Adjunctive therapy with drugs that affect plasma felbamate concentrations, especially other anticonvulsants, may warrant further reductions in felbamate daily dosage in patients with renal impairment. (See Renal Impairment under Cautions.)
Geriatric Patients
Initial dosage usually should be at the low end of dosage range. (See Geriatric Use under Cautions.)
Cautions for Felbamate
Contraindications
-
History of any blood dyscrasia or hepatic dysfunction.
-
Known hypersensitivity to felbamate, other carbamates, or any ingredient in the formulation.
Warnings/Precautions
Warnings
Hematologic Effects
Increased risk of potentially fatal aplastic anemia. (See Boxed Warning.)
Risk factors for development of aplastic anemia not identified; no known documented effective means to monitor patients to avoid and/or reduce the risk of aplastic anemia.
Consider expert hematologic consultation prior to initiation of therapy and whenever any hematologic abnormality is detected during therapy.
Full hematologic evaluations (e.g., CBC) recommended before initiation of felbamate therapy, at frequent intervals during therapy, and for a substantial period of time following discontinuance of therapy.
If any evidence of bone marrow depression occurs, discontinue the drug. Patients remain at risk for a variable, and unknown, period of time following drug discontinuance.
Hepatic Effects
Increased risk of acute hepatic failure resulting in death or hepatic transplantation. (See Boxed Warning.)
Risk factors for development of hepatic failure not identified; no known documented effective means to monitor patients to avoid and/or reduce the risk of acute hepatic failure.
Monitor serum transaminase (ALT, AST) concentrations prior to initiation of therapy and periodically thereafter (precise schedule for monitoring based on clinician’s judgment). Time course for progression from normal hepatic function to hepatic failure currently unknown.
If serum ALT or AST concentrations increase to ≥2 times ULN or if clinical signs and symptoms suggestive of hepatic failure occur, discontinue felbamate and monitor hepatic function until values return to normal.
Do not reinitiate therapy in patients who develop evidence of hepatocellular injury and are withdrawn from felbamate for any reason.
Discontinuance of Therapy
Abrupt withdrawal may result in increased seizure frequency; withdraw gradually.
To minimize the risk of adverse withdrawal effects, it has been recommended that dosage be decreased at 4- to 5-day intervals in increments that are one-third of the baseline daily dosage; according to this schedule, therapy usually can be discontinued over a period of 8–10 days. If the clinician determines that abrupt discontinuance is necessary, felbamate therapy may be stopped without gradual decreases in dosage provided that the patient receives adequate doses of another anticonvulsant.
Suicidality Risk
Increased risk of suicidality (suicidal ideation or behavior) observed in an analysis of studies using various anticonvulsants in patients with epilepsy, psychiatric disorders (e.g., bipolar disorder, depression, anxiety), and other conditions (e.g., migraine, neuropathic pain); risk in patients receiving anticonvulsants (0.43%) was approximately twice that in patients receiving placebo (0.24%). Increased suicidality risk was observed as early as 1 week after initiation of anticonvulsant therapy and continued through 24 weeks. Relative risk was higher for patients with epilepsy compared with those receiving anticonvulsants for other conditions.
Closely monitor all patients currently receiving or beginning anticonvulsant therapy for changes in behavior that may indicate emergence or worsening of suicidal thoughts or behavior or depression.
Balance risk of suicidality with the risk of untreated illness. Epilepsy and other illnesses treated with anticonvulsants are themselves associated with morbidity and mortality and an increased risk of suicidality. If suicidal thoughts or behavior emerge during anticonvulsant therapy, consider whether these symptoms may be related to the illness itself. (See Advice to Patients.)
Sensitivity Reactions
Dermatologic and Sensitivity Reactions
Severe dermatologic reactions (i.e., toxic epidermal necrolysis [TEN], Stevens-Johnson syndrome [SJS]) and photosensitivity reported rarely.
Specific Populations
Pregnancy
Category C. In animal studies in rats, decreased pup weight and increased pup mortality observed during lactation; however, no studies in pregnant women. Use during pregnancy only if clearly needed.
North American Antiepileptic Drug (NAAED) pregnancy registry (for patients) at 888-233-2334 or [Web].
Lactation
Distributed into milk; since the potential effect in nursing infants is not known, some clinicians state that the drug probably should not be used during breast-feeding.
Pediatric Use
Safety and efficacy for the management of Lennox-Gastaut syndrome not established in children <2 years of age.
Safety and efficacy in children other than those with Lennox-Gastaut syndrome not established. However, may be used in adolescents ≥14 years of age with partial seizures.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults; select dosage with caution. Consider the greater frequency of decreased hepatic, renal, and cardiac function and of concomitant disease and other drug therapy observed in the elderly.
Hepatic Impairment
Contraindicated in patients with hepatic impairment. (See Contraindications under Cautions and also see Boxed Warning.)
Renal Impairment
Use with caution; decreased clearance; dosage adjustments necessary. (See Renal Impairment under Dosage and Administration and also see Special Populations under Pharmacokinetics.)
Common Adverse Effects
Adjunctive therapy in children: Anorexia, vomiting, insomnia, headache, and somnolence.
Monotherapy or adjunctive therapy in adults: Anorexia, nausea, vomiting, insomnia, and headache; dizziness and somnolence also are frequent during adjunctive therapy.
Drug Interactions
Partially metabolized by CYP isoenzymes, principally CYP3A4 and CYP2E1. Inhibits CYP2C19; weakly induces CYP3A4.
Drugs Affecting Hepatic Microsomal Enzymes
Inducers of CYP3A4: Potential pharmacokinetic interaction (decreased plasma felbamate concentrations).
Inhibitors of CYP3A4: Pharmacokinetic interaction unlikely.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP3A4: Potential pharmacokinetic interaction (decreased plasma substrate concentrations).
Substrates of CYP2C19: Potential pharmacokinetic interaction (increased plasma substrate concentrations).
Specific Drugs
|
Drug |
Interaction |
Comment |
|---|---|---|
|
Antacids |
Pharmacokinetic interaction unlikely |
|
|
Carbamazepine |
Increased felbamate clearance; steady-state trough concentrations of felbamate decreased approximately 40% Decreased steady-state plasma carbamazepine concentrations and increased steady-state plasma carbamazepine epoxide concentrations |
Reduce carbamazepine dosage by 20–33% |
|
Clobazam |
Possible decreased plasma concentrations of clobazam |
|
|
Clonazepam |
Possible increased plasma concentrations of clonazepam |
|
|
Contraceptives, oral (e.g., low-dose combinations containing ethinyl estradiol and gestodene [not commercially available in the US]) |
Decreased gestodene AUC; intermenstrual bleeding reported No clinically relevant effect on ethinyl estradiol pharmacokinetics |
Use of felbamate with low-dose estrogen not recommended |
|
Erythromycin |
Effect on felbamate pharmacokinetics unlikely |
|
|
Phenobarbital |
Possible decreased plasma felbamate concentrations by 29% Increased plasma phenobarbital concentrations |
Reduce phenobarbital dosage by 20–33% |
|
Phenytoin |
Felbamate clearance doubled; steady-state trough concentrations of felbamate decreased approximately 45% Increased steady-state plasma phenytoin concentrations |
Reduce phenytoin dosage by 20–33% |
|
Valproate |
No clinically important effect on plasma felbamate concentrations Increased steady-state plasma valproate concentrations |
Reduce valproate dosage by 20–33% |
|
Warfarin |
Possible increased plasma concentrations of warfarin |
Dosage reduction of warfarin may be necessary |
Felbamate Pharmacokinetics
Absorption
Bioavailability
Well absorbed after oral administration. Oral bioavailability estimated to be ≥90%.
Commercially available tablets and oral suspension are bioequivalent to the capsule formulation used in clinical trials; pharmacokinetic profiles of the tablets and oral suspension are similar.
Food
Food has no effect on absorption of tablets; effect of food on absorption of the suspension has not been evaluated.
Distribution
Extent
Crosses the placenta in rats.
Distributed into human milk.
Plasma Protein Binding
22–25% (principally albumin).
Elimination
Metabolism
Undergoes partial hepatic metabolism via N-glucuronidation, oxidation, and hydroxylation mediated by CYP3A4 and 2E1; monocarbamate, p-hydroxy, and 2-hydroxy metabolites appear to contribute little, if any, to the anticonvulsant action of the drug.
Elimination Route
Excreted principally in urine (>90%) as unchanged drug (40–50%), unidentified metabolites and conjugates (40%), and monocarbamate, p-hydroxy, and 2-hydroxy metabolites (15%).
Half-life
Terminal half-life is approximately 20–23 hours.
Special Populations
Renal impairment decreases total body clearance by 40–50% and prolongs half-life by 9–15 hours.
Effects of hepatic impairment on felbamate pharmacokinetics have not been evaluated.
Stability
Storage
Oral
Suspension and Tablets
Tight containers at 20–25°C. Some manufacturers recommend to also avoid exposure to light during storage.
Actions
-
Structurally related to but pharmacologically distinct from meprobamate, an anxiolytic agent.
-
Exact mechanism of action of anticonvulsant effect not known, but available data suggest that the drug increases seizure threshold and reduces seizure spread.
-
Exhibits a spectrum of anticonvulsant activity that is pharmacologically distinct from the spectra of other currently available agents.
-
Weak inhibitor in vitro at GABA receptors and benzodiazepine receptors.
Advice to Patients
-
Importance of advising patients or caregivers to read the manufacturer's patient information (Medication Guide).
-
Risk of aplastic anemia; importance of notifying clinicians if signs of infection, bleeding, easy bruising, or signs of anemia (e.g., fatigue, weakness, lassitude) occur.
-
Risk of hepatic failure; importance of immediately notifying clinicians if signs of liver dysfunction (e.g., jaundice, anorexia, GI complaints, malaise) occur and of adhering to prescribed schedule of liver function tests.
-
Risk of suicidality (anticonvulsants, including felbamate, may increase risk of suicidal thoughts or actions in about 1 in 500 people). Importance of patients, family, and caregivers being alert to day-to-day changes in mood, behavior, and actions and immediately informing clinician of any new or worrisome behaviors (e.g., talking or thinking about wanting to hurt oneself or end one’s life, withdrawing from friends and family, becoming depressed or experiencing worsening of existing depression, becoming preoccupied with death and dying, giving away prized possessions).
-
Importance of women informing their clinician if they are or plan to become pregnant or to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Suspension |
600 mg/5 mL* |
Felbamate Suspension |
|
|
Felbatol |
Meda |
|||
|
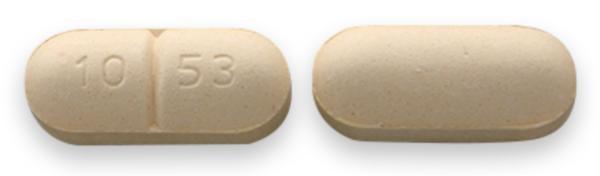
Tablets |
400 mg* |
Felbamate Tablets |
||
|
Felbatol (scored) |
Meda |
|||
|
600 mg* |
Felbamate Tablets |
|||
|
Felbatol (scored) |
Meda |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions December 16, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Lamictal
Lamictal is an anti-epileptic medication used treat seizures in adults and children over 2 years ...
Klonopin
Klonopin (clonazepam) is used to control seizures in epilepsy and for the treatment of panic ...
Dupixent
Dupixent is used to treat eczema, eosinophilic or oral-corticosteroid-dependent asthma, chronic ...
Topamax
Topamax (topiramate) is used to prevent seizures in adults and children and to prevent migraine ...
Epidiolex
Epidiolex (cannabidiol) is an oral prescription liquid CBD medicine that may be used to treat ...
Onfi
Onfi (clobazam) is used to treat seizures associated with Lennox-Gastaut syndrome, a form of ...
Cannabidiol
Cannabidiol information from Drugs.com, includes Cannabidiol side effects, interactions and indications.
Clobazam
Clobazam is used for epilepsy, lennox-gastaut syndrome, seizures
Topiramate
Learn about topiramate, an anticonvulsant used for seizures, migraine prevention, and weight loss ...
More about felbamate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (13)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: carbamate anticonvulsants
- Breastfeeding
- En español