Cardioversion
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about cardioversion?
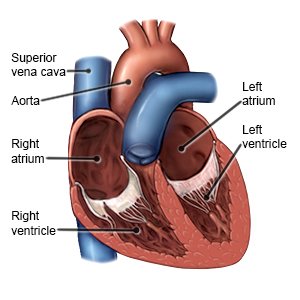
Cardioversion is a procedure that uses medicine or electric shocks to correct arrhythmias. An arrhythmia is a heartbeat that is too slow, too fast, or irregular. It may prevent your body from getting the blood and oxygen it needs. Your heart has 4 chambers, called the atria and ventricles. The atria are at the top of your heart, and the ventricles are at the bottom of your heart. Most arrhythmias that need cardioversion start in the atria.
 |
How do I prepare for cardioversion?
You may need a transesophageal echocardiogram (TEE) before your cardioversion. A TEE is an ultrasound to check for clots in your heart. You may need to take blood thinner medicine for several weeks before your cardioversion. This will help prevent blood clots. Your provider will talk to you about how to prepare for cardioversion. He or she may tell you not to eat or drink anything after midnight on the day of your cardioversion. He or she will tell you what medicines to take or not take on the day of your cardioversion. Arrange for someone to drive you home and stay with you for 24 hours. This person can call 911 if you have problems after your cardioversion.
What will happen during a chemical cardioversion?
You will be placed on a heart monitor. A heart monitor is an EKG that records your heart's electrical activity. Your provider will inject 1 or more medicines into your IV. The medicines will help change your heartbeat to a normal rhythm. You may feel light headed, dizzy, or nauseous. You may have pain or pressure in your chest, jaw, shoulders, or arms. These symptoms are normal, and usually last for a minute or less. You may need electrical cardioversion if chemical cardioversion does not change your heartbeat to a normal rhythm.
Related medications
What will happen during an electrical cardioversion?
You will be given medicine through your IV to keep you asleep and free from pain. You will be placed on a heart monitor. A heart monitor is an EKG that records your heart's electrical activity. A provider will also monitor your blood pressure and oxygen levels during the procedure. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils.
- In external cardioversion your provider will place sticky pads on your chest and back. Your heart will be shocked with electricity through the pads. Your heart may be shocked more than once to help it return to its normal rhythm.
- In internal cardioversion your provider will insert a catheter through a vein and into your heart. Your heart will be shocked through the catheter. Your heart may be shocked more than once to help it return to its normal rhythm.
What will happen after cardioversion?
Providers will monitor your heartbeat, blood pressure, and oxygen levels. You may feel drowsy from the medicine you were given during the procedure. Your chest may be red or sore where the pads were placed. This should go away in a few days. You may go home when they say it is okay or you may need to stay in the hospital.
What are the risks of cardioversion?
Your skin may be burned from the electric shocks. Cardioversion may cause a blood clot to travel to your heart or brain and cause a heart attack or stroke. You may develop a life-threatening arrhythmia or low blood pressure during cardioversion. You may need medicine or more electric shocks to treat this. Even with cardioversion, your heartbeat may not change or may not stay regular.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
