Pirfenidone (Monograph)
Brand name: Esbriet
Drug class: Antifibrotic Agents
Introduction
Antifibrotic agent; synthetic pyridone.
Uses for Pirfenidone
Idiopathic Pulmonary Fibrosis
Treatment of idiopathic pulmonary fibrosis (IPF); designated an orphan drug by FDA for this use.
A joint clinical practice guideline from the American Thoracic Society (ATS), European Respiratory Society (ERS), Japanese Respiratory Society (JRS), and the Latin American Thoracic Association (ALAT) gives a conditional recommendation for use of pirfenidone in patients with IPF; the decision to treat should factor in the potential benefits of therapy and risk of disease progression versus potential adverse effects and costs of therapy.
Pirfenidone Dosage and Administration
General
Pretreatment Screening
-
Monitor liver function tests prior to initiation of therapy.
Patient Monitoring
-
Monitor liver function tests monthly for the first 6 months, and then every 3 months.
Administration
Oral Administration
Administer orally 3 times daily with food.
Administer at the same time every day; do not exceed 3 doses per day.
If a dose is missed, take the next dose as soon as it is remembered; do not take 2 doses at the same time to make up for a missed dose.
Dosage
Adults
Idiopathic Pulmonary Fibrosis
Oral
Recommended maintenance dosage: 801 mg 3 times daily.
Initial dosage titration upward over 2-week period: 267 mg 3 times daily for 7 days, followed by 534 mg (two 267-mg capsules or tablets) 3 times daily for the next 7 days, and then 801 mg 3 times daily thereafter starting on day 15. The maximum recommended daily dosage is 2403 mg (801 mg 3 times daily).
Following treatment interruption of ≥14 days: Titrate dosage upward using the initial 2-week dosage titration regimen.
Following treatment interruption of <14 days: Therapy can be resumed at dosage received prior to treatment interruption.
Dosage Modification
Hepatic Toxicity
ALT or AST elevations >3 times but ≤5 times the ULN without symptoms or hyperbilirubinemia: May continue therapy at full dosage, temporarily interrupt therapy, or reduce dosage until liver function tests return to normal. May resume therapy and subsequently increase to full dosage as tolerated. Monitor patients carefully; discontinue other medications that could cause liver enzyme elevations; exclude other causes of such elevations.
ALT or AST elevations >3 times but ≤5 times the ULN with symptoms or hyperbilirubinemia, or ALT or AST >5 times the ULN: Permanently discontinue therapy.
Other Adverse Effects
If clinically important adverse reactions occur (i.e., GI effects such as nausea, diarrhea, dyspepsia, vomiting; photosensitivity reaction or rash; severe cutaneous adverse reactions), consider interruption of therapy or temporary dosage reduction until symptoms resolve. If severe cutaneous adverse reaction is confirmed, permanently discontinue therapy.
Concomitant Use with Drugs Affecting Hepatic Microsomal Enzymes
If concomitant use with a potent CYP1A2 inhibitor (e.g., fluvoxamine) cannot be avoided, reduce pirfenidone dosage to 267 mg (1 capsule) 3 times daily.
If concomitant use with the moderate CYP1A2 inhibitor ciprofloxacin (at a dosage of 750 mg twice daily) cannot be avoided, reduce pirfenidone dosage to 534 mg (two 267-mg capsules) 3 times daily.
Special Populations
Hepatic Impairment
No initial dosage adjustment required in patients with mild or moderate hepatic impairment (Child-Pugh class A or B); monitor closely for adverse effects.
Not studied in patients with severe hepatic impairment (Child-Pugh class C); use not recommended.
Renal Impairment
No initial dosage adjustment required in patients with mild, moderate, or severe renal impairment; monitor closely for adverse effects.
Not studied in patients with end-stage renal disease requiring dialysis; use not recommended.
Geriatric Patients
Dosage adjustment not required.
Cautions for Pirfenidone
Contraindications
-
None.
Warnings/Precautions
Elevated Liver Enzymes and Drug-Induced Liver Injury
Cases of drug-induced liver injury, both non-serious and serious cases of liver injury that have led to a fatal outcome, have been reported with pirfenidone use. If abnormal liver function test results occur, temporary interruption, dosage reduction, or discontinuance of therapy may be necessary.
Perform liver function tests prior to initiation, monthly for the first 6 months, and then every 3 months thereafter.
Photosensitivity Reaction or Rash
Photosensitivity reactions manifested as rash or other reactions reported. Most of these reactions occurred during the first 6 months following therapy initiation.
Interruption of therapy and/or dosage reduction may be necessary in some patients.
Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS) reported. Interrupt pirfenidone until cause of the reaction determined. Consult a dermatologist and, if a severe cutaneous adverse reaction is confirmed, permanently discontinue therapy.
GI Effects
Nausea, diarrhea, dyspepsia, vomiting, GERD, and abdominal pain may occur. Adverse GI effects generally occur within first 3 months of therapy and decrease over time.
Interruption of therapy and/or dosage reduction may be necessary in some patients.
Specific Populations
Pregnancy
Data are insufficient to determine the drug-associated risks of birth defects and miscarriage. In animal reproductive studies, pirfenidone was not teratogenic when administered at oral doses up to 2 and 3 times the maximum recommended adult dosage.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
No overall differences in safety and efficacy relative to younger adults.
Hepatic Impairment
Increased peak plasma concentrations and systemic exposure to pirfenidone occurred in patients with moderate hepatic impairment (Child-Pugh class B); not studied in patients with severe hepatic impairment (Child-Pugh class C).
Renal Impairment
Increased systemic exposure in patients with mild to severe renal impairment (Clcr <30 to 80 mL/minute); not studied in patients with end-stage renal disease requiring dialysis.
Common Adverse Effects
Adverse effects (≥10%): Nausea, rash, abdominal pain, upper respiratory tract infection, diarrhea, fatigue, headache, decreased appetite, dyspepsia, dizziness, vomiting, GERD, sinusitis, insomnia, decreased weight, arthralgia.
Drug Interactions
Metabolized principally by CYP1A2 and, to a lesser extent, by CYP2C9, 2C19, 2D6, and 2E1.
Has weak inhibitory potential on P-glycoprotein (P-gp) in vitro.
Concentration-dependent inhibition of CYP2C9, 2C19, 1A2, 2D6, and 3A4 in vitro.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP1A2 inhibitors: Potential increased pirfenidone exposure. Avoid concomitant use or reduce pirfenidone dosage to 267 mg 3 times daily (801 mg/day).
Moderate CYP1A2 inhibitors: Potential increased pirfenidone exposure; monitor patients closely during concomitant use.
Avoid concomitant use with drugs or combination of drugs that are potent or moderate inhibitors of both CYP1A2 and one or more other CYP isoenzymes involved with pirfenidone metabolism (i.e., CYP2C9, 2C19, 2D6, 2E1).
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cigarette smoking |
Decreased pirfenidone concentrations |
Advise patients to stop smoking prior to initiation of therapy and to avoid smoking during therapy |
|
Ciprofloxacin |
Increased systemic exposure to pirfenidone following concomitant administration with ciprofloxacin 750 mg twice daily |
Ciprofloxacin 750 mg twice daily: If concomitant therapy cannot be avoided, reduce pirfenidone dosage to 534 mg 3 times a day Ciprofloxacin 250–500 mg once daily: If concomitant therapy required, monitor patient closely |
|
Fluvoxamine |
Increased systemic exposure to pirfenidone approximately fourfold in nonsmokers and sevenfold in smokers |
Discontinue fluvoxamine prior to initiation of pirfenidone; avoid concomitant use If concomitant use cannot be avoided, reduce pirfenidone dosage to 267 mg 3 times a day Monitor patients for adverse effects; consider discontinuance of pirfenidone as needed |
Pirfenidone Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations achieved at a median of 0.5 hours (range: 0.5–4 hours) following oral administration.
Absolute bioavailability not known.
Bioequivalence demonstrated in fasting state between 801 mg tablet and three 267 mg capsules.
Food
Administration with food decreases systemic exposure by 16% and delays median time to peak plasma concentrations by 2.5 hours compared with the fasting state.
Special Populations
Systemic exposure and peak plasma concentrations increased approximately 1.6- and 1.4-fold, respectively, in individuals with moderate hepatic impairment (Child-Pugh class B).
Systemic exposure increased approximately 1.4-, 1.5-, and 1.2-fold in individuals with mild, moderate, and severe renal impairment, respectively.
Distribution
Extent
Not known whether pirfenidone is distributed into human milk.
Plasma Protein Binding
58% (mainly albumin).
Elimination
Metabolism
Undergoes hepatic metabolism, principally by CYP1A2 (70–80%) and, to a lesser extent, by CYP2C9, 2C19, 2D6, and 2E1. Major metabolite 5-carboxy-pirfenidone expected to be pharmacologically inactive.
Elimination Route
Approximately 80% excreted in urine within 24 hours, mainly as 5-carboxy-pirfenidone.
Half-life
Approximately 3 hours.
Stability
Storage
Oral
Capsules and Tablets
25°C (excursions permitted to 15–30°C).
Actions
-
Precise mechanism of action in the treatment of IPF not fully elucidated; may be related to the drug's antifibrotic, anti-inflammatory, and antioxidant properties.
-
Inhibits activation of transforming growth factor-β (TGF-β), a profibrotic, proinflammatory cytokine that plays a role in the differentiation of fibroblasts.
-
Inhibits TGF-β-mediated proliferation of human lung fibroblasts and differentiation into myofibroblasts in vitro, a process which may lead to excessive collagen deposition and fibrosis in the lungs.
-
Inhibits release of proinflammatory cytokines (e.g., IL-1β, IL-6, tumor necrosis factor [TNF]-α, platelet derived growth factor [PDGF]) in animal models and in vitro.
-
Possesses antioxidant activity; shown to scavenge reactive oxygen species (ROS), including hydroxyl radicals and superoxide anions, in vitro.
Advice to Patients
-
Advise patients to read the manufacturer’s patient information prior to beginning pirfenidone therapy and each time the prescription is refilled.
-
Advise patients to take pirfenidone with food to reduce the incidence of adverse effects (e.g., nausea and dizziness).
-
Advise patients that if a dose of pirfenidone is missed, the dose should be taken as soon as it is remembered; 2 doses should not be taken at the same time to make up for a missed dose. No more than 3 doses should be taken per day.
-
Risk of hepatotoxicity; inform patients of the importance of periodic liver function test monitoring. Advise patients to immediately report any manifestations of hepatotoxicity (e.g., jaundice, unusually dark or “tea-colored” urine, right upper quadrant pain, bleeding or bruising more easily than normal, lethargy).
-
Risk of photosensitivity manifesting as rash or other reactions. Advise patients to use sunscreen and protective clothing, and limit exposure to sunlight, including sunlamps, during therapy. Advise patients to report any symptoms of photosensitivity reaction or rash to a clinician.
-
Risk of adverse GI effects (e.g., nausea, diarrhea, dyspepsia, vomiting, gastroesophageal reflux disease [GERD], abdominal pain). Advise patients to contact their clinician if persistent adverse GI effects occur.
-
Risk of severe cutaneous adverse reactions. Advise patients to contact their clinician if severe skin reactions occur during therapy.
-
Advise cigarette smokers to avoid smoking during pirfenidone therapy because plasma concentrations of the drug and efficacy may be reduced.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements as well as any concomitant illnesses (e.g., hepatic impairment).
-
Advise women to inform their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Pirfenidone is available only through certain specialty pharmacies. Contact the manufacturer or consult the Esbriet website ([Web]) for specific availability information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
267 mg |
Esbriet |
Genentech |
|
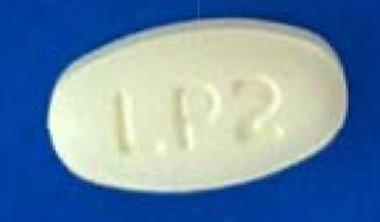
Tablets |
267 mg |
Esbriet |
Genentech |
|
|
801 mg |
Esbriet |
Genentech |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
More about pirfenidone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (21)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous uncategorized agents
- En español