Tocilizumab Side Effects
Applies to tocilizumab: solution.
Warning
Intravenous route (Solution)
Risk Of Serious InfectionsPatients treated with tocilizumab products including tocilizumab-bavi are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.If a serious infection develops, interrupt tocilizumab-bavi until the infection is controlled.Reported infections include: 1. Active tuberculosis, which may present with pulmonary or extrapulmonary disease. Patients should be tested for latent tuberculosis before tocilizumab-bavi use and during therapy. Treatment for latent infection should be initiated prior to tocilizumab-bavi use. 2. Invasive fungal infections, including candidiasis, aspergillosis, and pneumocystosis. Patients with invasive fungal infections may present with disseminated, rather than localized, disease. 3. Bacterial, viral and other infections due to opportunistic pathogens.The risks and benefits of treatment with tocilizumab-bavi should be carefully considered prior to initiating therapy in patients with chronic or recurrent infection.Patients should be closely monitored for the development of signs and symptoms of infection during and after treatment with tocilizumab-bavi, including the possible development of tuberculosis in patients who tested negative for latent tuberculosis infection prior to initiating therapy.
Serious side effects of Tocilizumab
Along with its needed effects, tocilizumab may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking tocilizumab:
More common
- Black, tarry stools
- bloody or cloudy urine
- blurred vision
- body aches or pain
- chest pain or tightness
- chills
- cough with or without mucus
- diarrhea
- difficult, burning, or painful urination
- difficulty breathing
- difficulty swallowing
- dizziness
- ear congestion
- fast heartbeat
- feeling of warmth
- fever
- frequent urge to urinate
- headache
- hives, itching, skin rash
- loss of appetite
- loss of consciousness
- loss of voice
- lower back or side pain
- nausea
- nervousness
- pain or tenderness around the eyes and cheekbones
- painful blisters on the trunk of the body
- pale skin
- pounding in the ears
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- redness of the face, neck, arms, and occasionally, upper chest
- slow or fast heartbeat
- sneezing
- sore throat
- stomach pain
- stuffy or runny nose
- sudden sweating
- ulcers, sores, or white spots in the mouth
- unusual bleeding or bruising
- unusual tiredness or weakness
Less common
- Accumulation of pus
- anxiety
- bladder pain
- burning feeling in the chest or stomach
- confusion
- dark urine
- decrease in height
- decreased urine
- difficulty moving
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- dry mouth
- fast, irregular, pounding, or racing heartbeat or pulse
- feeling hot
- general feeling of discomfort or illness
- heartburn
- increased thirst
- indigestion
- itching, pain, redness, swelling, tenderness, or warmth on the skin at the injection site
- joint pain
- light-colored stools
- loss of appetite
- mood changes
- muscle ache, pain, cramp, or stiffness
- numbness or tingling in the hands, feet, or lips
- pain in the back, ribs, arms, legs, groin, or genitals
- severe stomach pain
- sharp back pain just below the ribs
- shivering
- stomach upset
- sweating
- swollen joints
- swollen, painful, or tender lymph glands in the face, neck, armpit, or groin
- swollen, red, or tender area of infection
- tenderness in the stomach area
- trouble with sleeping
- unexplained runny nose or sneezing
- vomiting
- yellow eyes and skin
Rare
- Belching
- changes in skin color
- coughing or spitting up blood
- fainting
- gaseous stomach pain
- lightheadedness
- neck pain
- night sweats
- noisy breathing
- rapid, shallow breathing
- recurrent fever
- red, tender, or oozing skin at the wounded area
- sudden high fever or low-grade fever for months
- swelling of the foot or leg
- weight loss
Incidence not known
- Blistering, peeling, loosening of the skin
- bloating
- dilated neck veins
- pains in the stomach, side, or abdomen, possibly radiating to the back
- red skin lesions, often with a purple center
- red, irritated eyes
- severe stomach pain, cramping, or burning
- swelling of the face, fingers, feet, or lower legs
- vomiting of material that looks like coffee grounds, severe and continuous
- weight gain
Other side effects of Tocilizumab
Some side effects of tocilizumab may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Burning, dry, or itching eyes
- constipation
- discharge, excessive tearing
- redness, pain, or swelling of the eye, eyelid, or inner lining of the eyelid
- skin rash, encrusted, scaly and oozing
- swelling or inflammation of the mouth
Less common
- Abnormal or decreased touch sensation
- bleeding or redness and swelling of the gums
- blemishes on the skin
- bloody eye
- chapped, red, or swollen lips
- earache
- feeling of constant movement of self or surroundings
- irritation in the mouth
- loose teeth
- persistent breath odor or bad taste in your mouth
- pimples
- redness or swelling in the ear
- scaling, redness, burning, pain, or other signs of inflammation on the lips
- sensation of spinning
- sore mouth or tongue
- white patches in the mouth or on the tongue
Rare
- Bleeding after passing stool
- blindness
- bloody nose
- burning, numbness, tingling, or painful sensations
- change in hearing
- continuing ringing or buzzing or other unexplained noise in the ears
- coughing or spitting up blood
- decreased vision or other changes in vision
- dry mouth
- ear drainage
- flushed, dry skin
- fruit-like breath odor
- hearing loss
- increased hunger, thirst, urination
- itching ears
- uncomfortable swelling around the anus
- unexplained weight loss
- unsteadiness or awkwardness
- weakness in the arms, hands, legs, or feet
For Healthcare Professionals
Applies to tocilizumab: intravenous solution, subcutaneous solution.
General
The most common adverse reactions were upper respiratory tract infections, nasopharyngitis, headache, hypertension, increased ALT, and injection site reactions. The most common serious adverse reactions were serious infections.[Ref]
Cardiovascular
Common (1% to 10%): Hypertension
Uncommon (0.1% to 1%): Myocardial infarction
Frequency not reported: Hypotension[Ref]
Dermatologic
Common (1% to 10%): Rash, pruritus, urticaria, cellulitis, skin reactions
Frequency not reported: Angioedema
Postmarketing reports: Stevens-Johnson syndrome[Ref]
Endocrine
Uncommon (0.1% to 1%): Hypothyroidism[Ref]
Gastrointestinal
GI perforations were primarily reported as complications of diverticulitis (including generalized purulent peritonitis, lower GI perforation, fistula, and abscess). Most patients who developed GI perforations were taking concomitant nonsteroidal anti-inflammatory medications (NSAIDs), corticosteroids, or methotrexate.[Ref]
Common (1% to 10%): Abdominal pain, mouth ulceration, gastritis, diarrhea, oral herpes simplex, upper abdominal pain, constipation, nausea
Uncommon (0.1% to 1%): Stomatitis, gastric ulcer, diverticulitis, gastrointestinal (GI) perforations
Frequency not reported: Gastroenteritis, diverticulitis complications (including generalized purulent peritonitis, lower GI perforation, fistula, abscess), epigastric discomfort
Postmarketing reports: Pancreatitis[Ref]
Genitourinary
Common (1% to 10%): Urinary tract infection
Hematologic
Very common (10% or more): Bleeding events
Common (1% to 10%): Leukopenia, neutropenia, thrombocytopenia, decreased neutrophil counts, decreased platelet counts, serious bleeding
Postmarketing reports: Hypofibrinogenemia, pancytopenia[Ref]
Hepatic
Increased ALT and AST greater than the upper limit of normal (ULN) to 3 times ULN (3 x ULN) were reported in up to 48% and up to 41% of patients, respectively. Increased ALT and AST greater than 3 to 5 x ULN were reported in up to 5% and up to 2% of patients, respectively. Increased ALT and AST greater than 5 x ULN were reported in up to 1.5% and up to 0.7% of patients, respectively.
ALT or AST at least 5 x ULN occurred in 11.7% of patients who received this drug for coronavirus disease 2019 (COVID-19).[Ref]
Very common (10% or more): Increased ALT (up to 48%), increased AST (up to 41%)
Common (1% to 10%): Increased hepatic transaminases, increased total bilirubin, hepatic events
Frequency not reported: Drug-induced hepatitis with hyperbilirubinemia
Postmarketing reports: Drug-induced liver injury, hepatitis, hepatic failure, jaundice[Ref]
Hypersensitivity
Common (1% to 10%): Hypersensitivity reactions (including anaphylaxis)
Uncommon (0.1% to 1%): Anaphylactic reactions
Frequency not reported: Anaphylactoid reactions
Postmarketing reports: Fatal anaphylaxis[Ref]
Immunologic
Common (1% to 10%): Anti-drug antibodies, neutralizing antibodies
Frequency not reported: Macrophage activation syndrome[Ref]
Local
Very common (10% or more): Injection site reactions (including erythema, pruritus, pain, hematoma)
Frequency not reported: Injection site swelling[Ref]
Metabolic
Very common (10% or more): Hypercholesterolemia
Common (1% to 10%): Hypokalemia
Uncommon (0.1% to 1%): Hypertriglyceridemia[Ref]
Musculoskeletal
Common (1% to 10%): Back pain
Frequency not reported: Bacterial arthritis, arthralgia[Ref]
Nervous system
Common (1% to 10%): Headache, dizziness, stroke[Ref]
Ocular
Common (1% to 10%): Conjunctivitis[Ref]
Oncologic
Uncommon (0.1% to 1%): Malignancies[Ref]
Other
Very common (10% or more): Increased low-density lipoprotein (LDL) cholesterol (up to 47%), infection (up to 30.3%), increased total cholesterol (up to 25%), serious infection (up to 18.6%)
Common (1% to 10%): Peripheral edema, herpes zoster, increased weight, infusion-related reactions
Uncommon (0.1% to 1%): Opportunistic infections
Frequency not reported: Sepsis, increased lipid parameters (total cholesterol, LDL cholesterol, high-density lipoprotein cholesterol, triglycerides), active tuberculosis[Ref]
Psychiatric
Common (1% to 10%): Anxiety, insomnia[Ref]
Renal
Uncommon (0.1% to 1%): Nephrolithiasis[Ref]
Respiratory
Very common (10% or more): Upper respiratory tract infection
Common (1% to 10%): Cough, dyspnea, nasopharyngitis, bronchitis, pneumonia
Frequency not reported: Invasive pulmonary infections (including candidiasis, aspergillosis, coccidioidomycosis, pneumocystis jirovecii)
Postmarketing reports: Interstitial lung disease (including pneumonitis, pulmonary fibrosis; some fatal outcomes)[Ref]
Frequently asked questions
- What are the new drugs for rheumatoid arthritis (RA)?
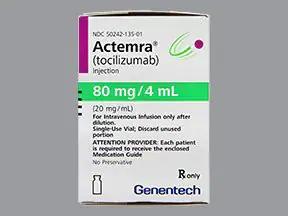
- What is Actemra used to treat?
- How many biosimilars have been approved in the United States?
- Is tocilizumab (Actemra) effective for treating COVID-19?
More about tocilizumab
- Check interactions
- Compare alternatives
- Reviews (52)
- Side effects
- Dosage information
- During pregnancy
- Drug class: interleukin inhibitors
- Breastfeeding
- En español
Patient resources
- Tocilizumab drug information
- Tocilizumab (Advanced Reading)
- Tocilizumab-bavi (Advanced Reading)
- Tocilizumab (Intravenous)
- Tocilizumab Prefilled Syringes
Other brands
Professional resources
Other brands
Related treatment guides
References
1. Product Information. Actemra (tocilizumab). Genentech. 2022;SUPPL-138/SUPPL-49.
2. Product Information. Actemra (tocilizumab). Roche Products Pty Ltd. 2022;Actemra 20220902.
3. Product Information. RoActemra (tocilizumab). Roche Products Ltd. 2022.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.