Proquin XR Side Effects
Generic name: ciprofloxacin
Medically reviewed by Drugs.com. Last updated on Mar 20, 2024.
Note: This document provides detailed information about Proquin XR Side Effects associated with ciprofloxacin. Some dosage forms listed on this page may not apply specifically to the brand name Proquin XR.
Applies to ciprofloxacin: oral powder for suspension, oral tablet.
Other dosage forms:
Important warnings
This medicine can cause some serious health issues
Oral route (tablet; tablet, extended release; suspension)
Fluoroquinolones, including ciprofloxacin, are associated with disabling and potentially irreversible serious adverse reactions that have occurred together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects.
Discontinue ciprofloxacin and avoid use of fluoroquinolones in patients with these serious adverse reactions.
Reserve use of ciprofloxacin for patients with no alternative treatment options for an uncomplicated UTI.
Fluoroquinolones, including ciprofloxacin, may exacerbate muscle weakness in persons with myasthenia gravis.
Avoid in patients with known history of myasthenia gravis.
Oral route (suspension; tablet, extended release; tablet)
Fluoroquinolones, including ciprofloxacin, are associated with disabling and potentially irreversible serious adverse reactions that have occurred together, including tendinitis and tendon rupture, peripheral neuropathy, and CNS effects.
Discontinue ciprofloxacin and avoid use of fluoroquinolones in patients with these serious adverse reactions.
Reserve use of ciprofloxacin for patients with no alternative treatment options for an acute exacerbation of chronic bronchitis or acute sinusitis.
Fluoroquinolones, including ciprofloxacin hydrochloride, may exacerbate muscle weakness in persons with myasthenia gravis.
Avoid in patients with known history of myasthenia gravis.
Serious side effects of Proquin XR
Along with its needed effects, ciprofloxacin (the active ingredient contained in Proquin XR) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking ciprofloxacin:
More common
- diarrhea
Rare
- bloody or black, tarry stools
- burning, crawling, itching, numbness, prickling, "pins and needles", or tingling feelings
- changes in skin color
- changes in urination
- chest pain, discomfort, tightness, or heaviness
- chills
- clumsiness or unsteadiness
- confusion
- continuing ringing or buzzing or other unexplained noise in the ears
- coughing or spitting up blood
- dizziness, fainting, or lightheadedness when getting up suddenly from a lying or sitting position
- fast, irregular, pounding, or racing heartbeat or pulse
- fever
- headache, severe and throbbing
- hearing loss
- hives or welts, skin rash
- joint stiffness
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- light-colored stools
- muscle pain or stiffness
- nausea
- nightmares
- numbness of the hands
- pain in the joints
- pain or discomfort in the arms, jaw, back, or neck
- painful, red lumps under the skin, mostly on the legs
- pounding in the ears
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- redness of the face, neck, arms, and occasionally, upper chest
- seizures
- severe stomach pain, cramping, or burning
- shakiness in the legs, arms, hands, or feet
- swelling of the face, feet, or lower legs
- swollen, painful, or tender lymph glands in the neck, armpit, or groin
- thick, white vaginal discharge with no odor or with a mild odor
- unsteadiness, trembling, or other problems with muscle control or coordination
- unusual drowsiness, dullness, tiredness, weakness, or feeling of sluggishness
- vomiting
- white patches in the mouth or on the tongue
- yellow eyes or skin
Incidence not known
- blistering, peeling, or loosening of the skin
- bluish-colored lips, fingernails, or palms
- bone pain
- diarrhea, watery and severe, which may also be bloody
- difficulty with breathing, chewing, or talking
- double vision
- excessive muscle tone
- feeling of discomfort
- feeling, seeing, or hearing things that are not there
- increased sensitivity of the skin to sunlight
- increased sensitivity to pain or touch
- irregular or slow heart rate
- loss of sense of smell
- mood changes
- nosebleeds
- rapid heart rate
- red skin lesions, often with a purple center
- seeing, hearing, or feeling things that are not there
- sensation of skin burning
- severe sunburn
- sores, ulcers, or white spots on the lips or in the mouth
- uncontrolled eye movements
- unusual bleeding or bruising
- unusual excitement, nervousness, or restlessness
- vaginal yeast infection
Other side effects of Proquin XR
Some side effects of ciprofloxacin may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
- runny or stuffy nose
- sneezing
For healthcare professionals
Applies to ciprofloxacin: intravenous solution, oral powder for reconstitution, oral tablet, oral tablet extended release.
General
The most common side effects (from clinical trials of all formulations, doses, durations of therapy, and indications) were nausea, diarrhea, abnormal liver function tests, vomiting, and rash. The most common side effects reported with the IV formulation were nausea, diarrhea, vomiting, injection and infusion site reactions, rash, and increased transaminases (transient).[Ref]
Gastrointestinal
- Common (1% to 10%): Nausea, diarrhea, vomiting, dyspepsia
- Uncommon (0.1% to 1%): Abdominal pains/discomfort, gastrointestinal (GI) pains, flatulence
- Rare (0.01% to 0.1%): Elevated amylase, antibiotic-associated colitis, pancreatitis
- Frequency not reported: Clostridium difficile-associated diarrhea, constipation, GI bleeding, ileus, intestinal perforation, dry mouth, oral ulceration, epigastric pain, dysphagia, elevated lipase, painful oral mucosa, heartburn, acid reflux, aggravated irritable bowel syndrome, lower abdominal pain
- Postmarketing reports: GI candidiasis, oral candidiasis, pseudomembranous colitis[Ref]
Antibiotic-associated colitis with possible fatal outcome was reported very rarely.
The onset of pseudomembranous colitis symptoms has been reported during or after antimicrobial treatment.[Ref]
Dermatologic
- Common (1% to 10%): Rash
- Uncommon (0.1% to 1%): Pruritus, urticaria
- Rare (0.01% to 0.1%): Angioedema, photosensitivity reactions, sweating/hyperhidrosis, petechiae, blistering
- Very rare (less than 0.01%): Erythema multiforme, erythema nodosum, Stevens-Johnson syndrome (potentially life-threatening), toxic epidermal necrolysis (potentially life-threatening)
- Frequency not reported: Exfoliative dermatitis, purpura, burning, phototoxicity reaction, dry skin, maculopapular rash, skin disorder, vesiculobullous rash, erythema, hyperpigmentation, cutaneous candidiasis, bullous pemphigoid, vesicles, lobular panniculitis, photoinduced acute exanthematous pustulosis, drug reaction with eosinophilia and systemic symptoms (DRESS)
- Postmarketing reports: Acute generalized exanthematous pustulosis, fixed eruption[Ref]
Photosensitivity was seen most often when patients were exposed to intense sun (e.g., as when used to treat or prevent travelers' diarrhea).
A 27-year-old woman with mild systemic erythematosus developed toxic epidermal necrolysis (TEN) after starting a second oral course of this drug after a prior 5-day course. She developed a rash, high fever, and diarrhea after taking the 2nd dose and presented with diffuse rash, epidermal sloughing of 60% of the skin, desquamation of the lips, shock, and respiratory distress. She died on the 28th hospital day of TEN, right ventricular failure, and acute respiratory distress syndrome. As of 2003, 9 cases of TEN, including 5 fatalities, had been reported in the literature.
Erythema nodosum, Stevens-Johnson syndrome (potentially life-threatening), and TEN (potentially life-threatening) have also been reported during postmarketing experience.[Ref]
Nervous system
- Common (1% to 10%): Headache, dizziness/lightheadedness, central nervous system disturbance
- Uncommon (0.1% to 1%): Sleep disorders, taste disorders, seizures (including status epilepticus), dysesthesia, paresthesia, vertigo, hearing loss
- Rare (0.01% to 0.1%): Syncope, hypoesthesia, tremor, tinnitus, migraine, olfactory nerve disorders, smell disorders, hearing impaired
- Very rare (less than 0.01%): Disturbed coordination, intracranial hypertension, benign intracranial hypertension/pseudotumor cerebri, exacerbation of myasthenia gravis, hyperesthesia
- Frequency not reported: Unresponsiveness, ataxia, hypertonia, anosmia, nystagmus, taste perversion/bad taste, somnolence/drowsiness, incoordination, disturbance in attention, dyskinesia, myasthenia gravis, paresis, aseptic meningitis, cerebral thrombosis, grand mal convulsion, dysphasia, lethargy, sensory axonal polyneuropathy, sensorimotor axonal polyneuropathy
- Postmarketing reports: Taste loss, peripheral neuropathy (may be irreversible), polyneuropathy[Ref]
Seizures have been reported in 2 patients given this drug and foscarnet. The temporal association between the onset of seizures and drug administration suggests a possible drug interaction; causal relationship was not established in either case. Both drugs are individually epileptogenic; concurrent use may potentiate risk of seizures.
Cases of sensory or sensorimotor axonal polyneuropathy (affecting small and/or large axons) resulting in paresthesias, hypoesthesias, dysesthesias, and weakness have been reported.
One survey reported 11 cases of peripheral neuropathy associated with this drug. The severity ranged from mild and reversible to severe and persistent. In 1 case, a 44-year-old female developed numbness, allodynia, hypoesthesia, tremors, electrical and diffuse burning sensations, twitching, disorientation, visual impairment, nausea, temperature intolerance, rash, and palpitations; she remained disabled after 29 months.
Nystagmus, anosmia, hyperesthesia, hypoesthesia, hypertonia, intracranial hypertension, and exacerbation of myasthenia gravis have also been reported during postmarketing experience.[Ref]
Hematologic
- Common (1% to 10%): Eosinophilia
- Uncommon (0.1% to 1%): Thrombocytopenia, thrombocythemia
- Rare (0.01% to 0.1%): Leukopenia, anemia, neutropenia, leukocytosis, pancytopenia, bone marrow depression, abnormal prothrombin level
- Very rare (less than 0.01%): Hemolytic anemia, agranulocytosis
- Frequency not reported: Decreased hematocrit, decreased platelet counts, increased platelet counts, prolonged prothrombin time, decreased prothrombin, bleeding diathesis, decreased hemoglobin, decreased leukocyte count, increased atypical lymphocyte count, immature WBCs, increased blood monocytes, elevated sedimentation rate, elevated eosinophil counts, lymphadenopathy
- Postmarketing reports: Methemoglobinemia, increased INR, prothrombin time prolonged or decreased[Ref]
Pancytopenia (life-threatening or fatal outcome) and bone marrow depression (life-threatening) were reported very rarely; also reported during postmarketing experience.
Increased INR was reported in patients treated with vitamin K antagonists.[Ref]
Hepatic
- Common (1% to 10%): Abnormal liver function tests, increased transaminases
- Uncommon (0.1% to 1%): Elevated bilirubin, hepatic impairment, cholestatic icterus/cholestatic jaundice, jaundice
- Rare (0.01% to 0.1%): Hepatitis, liver necrosis
- Very rare (less than 0.01%): Hepatic failure
- Frequency not reported: Elevated AST, elevated ALT, elevated GGT[Ref]
Liver necrosis very rarely progressed to life-threatening hepatic failure. Liver necrosis and hepatic failure (including fatal cases) have also been reported during postmarketing experience.[Ref]
Psychiatric
- Common (1% to 10%): Restlessness
- Uncommon (0.1% to 1%): Psychomotor hyperactivity/agitation, confusion, disorientation, hallucinations
- Rare (0.01% to 0.1%): Anxiety reaction, abnormal dreams, depression, psychotic reactions
- Frequency not reported: Depersonalization, insomnia, manic reaction, nightmares, paranoia, phobia, toxic psychosis, nervousness, self-injurious behavior, suicidal ideations/thoughts, attempted suicide, completed suicide, catatonia, mania (including hypomania)
- Postmarketing reports: Delirium[Ref]
Depression and psychotic reactions (both potentially culminating in self-injurious behavior such as suicidal ideations/thoughts and attempted or completed suicide) have been reported.
Agitation, confusion, and toxic psychosis have also been reported during postmarketing experience.[Ref]
Genitourinary
- Common (1% to 10%): Vaginal candidiasis
- Rare (0.01% to 0.1%): Hematuria, crystalluria
- Frequency not reported: Albuminuria, cylindruria, frequent urination, hemorrhagic cystitis, vaginitis, dysmenorrhea, candiduria, polyuria, urethral bleeding, urinary retention, urinary tract infection, fungal vaginosis, bacterial vaginitis, dysuria, abnormal urine odor, female genital pruritus, vaginal infection, urinary frequency, micturition urgency, vaginal pruritus[Ref]
Crystalluria has been reported in patients with alkaline urine and did not necessarily lead to nephrotoxicity. At physiological urinary pH, the risk of crystalluria was considered minor.
Vaginal candidiasis has also been reported during postmarketing experience.[Ref]
Local
- Common (1% to 10%): Local IV site reactions, injection and infusion site reactions (e.g., phlebitis, thrombophlebitis)
- Frequency not reported: Injection site irritation and induration with IV infusion[Ref]
Local IV site reactions occurred more often if the infusion time was 30 minutes or less. These reactions have appeared as local skin reactions and resolved quickly when infusion was completed.
Injection site irritation and induration have been reported with IV infusion time 30 minutes or less (instead of the recommended 1 hour) or when a small vein in the back of the hand was used.[Ref]
Musculoskeletal
- Uncommon (0.1% to 1%): Musculoskeletal pain (e.g., extremity pain, back pain, chest pain), arthralgia
- Rare (0.01% to 0.1%): Myalgia, arthritis, increased muscle tone and cramping, tendon rupture (mainly Achilles tendon)
- Very rare (less than 0.01%): Tendinitis, muscular weakness
- Frequency not reported: Arthropathy (including suspected reversible cases), joint stiffness, elevated serum creatine phosphokinase, abnormal joint exam, joint sprains, arthrosis, bone pain, decreased range of motion in a joint (knee, elbow, ankle, hip, wrist, shoulder), jaw pain, neck pain, gout flare-up, joint swelling, muscle spasms, night cramps, knee inflammation
- Postmarketing reports: Myoclonus, myasthenia, twitching[Ref]
Arthropathy has primarily been a concern in pediatric patients; however, at least 1 case was described in an adult cystic fibrosis patient receiving this drug. Although cystic fibrosis arthropathy and hypertrophic pulmonary osteoarthropathy typically occur in 7% to 8% of cystic fibrosis adults and adolescents, the arthropathy exhibited in this patient did not resemble either. Several elements in its presentation strongly supported the diagnosis of ciprofloxacin-induced arthropathy, such as: a consistent time of onset with other reported cases of suspected quinolone-induced arthropathy (usually 3 weeks after starting therapy); a lack of history of arthralgia in the patient; reoccurrence upon rechallenge; and resolution of symptoms upon discontinuation of therapy (usually 2 weeks after therapy stopped).
Tendinitis with subsequent tendon rupture has been documented in numerous case reports. One patient with chronic renal failure developed bilateral Achilles tendon rupture after 4 days of ciprofloxacin (the active ingredient contained in Proquin XR) therapy. Although renal transplant patients and those with end-stage renal disease tend to have an increased risk of Achilles tendinitis and rupture over the general population, quinolone use has been shown to further increase that risk (12% in quinolone-treated patients versus 7% in nonquinolone-treated patients).
As of October 1994, 25 cases of Achilles tendon rupture had been reported to the US FDA. Some ruptures have also occurred in the hand or shoulder. Other risk factors identified included age and corticosteroid use.
There had been 23 reports of tendinitis submitted to the Australian Adverse Drug Reactions Committee (ADRAC) between 2006 and 2008, including reports of Achilles tendinitis, tendon rupture, and tendon pain and swelling. The reports were primarily in male patients (15 cases) older than 56 years who used this drug for 2 to 14 days. In 19 of the reported cases, a fluoroquinolone (generally ciprofloxacin) was the primary suspect; however, details of concomitant serious medical conditions were not documented in most of the reports.
Musculoskeletal side effects reported in pediatric patients included arthralgia, abnormal gait, abnormal joint exam, joint sprains, leg pain, back pain, arthrosis, bone pain, pain, myalgia, arm pain, and decreased range of motion in a joint (knee, elbow, ankle, hip, wrist, shoulder).
Myalgia, tendinitis, and tendon rupture have also been reported during postmarketing experience.[Ref]
Cardiovascular
- Uncommon (0.1% to 1%): Tachycardia, vasodilatation, hypotension
- Rare (0.01% to 0.1%): Vasculitis
- Frequency not reported: Angina pectoris, cardiopulmonary arrest, myocardial infarction, hypertension, palpitation, bradycardia, arrhythmia, atrial flutter, cardiac murmur, cardiovascular collapse, ventricular ectopy, ventricular bigeminy, abdominal aortic bruit, postural hypotension
- Postmarketing reports: QT prolongation/ECG QT prolonged, torsade de pointes, ventricular arrhythmia[Ref]
Torsade de pointes was reported mainly in patients with risk factors for QT prolongation.
Vasculitis has also been reported during postmarketing experience.[Ref]
Other
- Uncommon (0.1% to 1%): Candida infections, mycotic superinfections, pain, fever, malaise/feeling unwell, asthenia, edema
- Very rare (less than 0.01%): Gait disturbance/abnormal gait
- Frequency not reported: Irritability, flushing, thirst, elevated serum calcium, elevated serum potassium, elevated triglycerides, decreased serum albumin, decreased serum potassium, decreased total serum protein, elevated serum theophylline, serum phenytoin altered, chills, swelling, breast pain, achiness, weakness, fatigue, suprapubic pain, rigors, tenderness, fungal infection, increased body temperature
- Postmarketing reports: Elevated serum cholesterol[Ref]
Elevated serum theophylline has been reported in patients receiving theophylline concomitantly.
Gait disturbance and elevated serum potassium have also been reported during postmarketing experience.[Ref]
Metabolic
- Uncommon (0.1% to 1%): Elevated blood alkaline phosphatase, decreased appetite/anorexia, decreased food intake
- Rare (0.01% to 0.1%): Hyperglycemia, hypoglycemia
- Frequency not reported: Elevated LDH, elevated uric acid, elevated blood glucose, decreased uric acid, decreased blood glucose, acidosis, symptomatic hypoglycemia[Ref]
Quinolone class antibiotics have been associated with symptomatic hypoglycemia.[Ref]
Renal
- Uncommon (0.1% to 1%): Renal impairment, renal failure
- Rare (0.01% to 0.1%): Tubulointerstitial nephritis
- Frequency not reported: Elevated serum creatinine, renal calculi, elevated BUN, decreased BUN, abnormal kidney function, allergic interstitial nephritis, nephritis, myoglobin-associated acute kidney injury/failure[Ref]
Allergic interstitial nephritis resulting in nonoliguric renal failure has been described in numerous case reports. Several cases included symptoms of rash, fever, and arthralgia and were accompanied by eosinophilia and eosinophiluria. Cases of allergic interstitial nephritis often responded to short courses of corticosteroid therapy.[Ref]
Ocular
- Uncommon (0.1% to 1%): Visual disturbances (e.g., chromatopsia, diplopia, photopsia)
- Very rare (less than 0.01%): Visual color distortions
- Frequency not reported: Decreased visual acuity, blurred vision, cataracts, multiple punctate lenticular opacities, eye pain[Ref]
Quinolone class antibiotics have been associated with cataracts and multiple punctate lenticular opacities.[Ref]
Hypersensitivity
- Rare (0.01% to 0.1%): Allergic reactions, anaphylactic shock (life-threatening), allergic edema
- Very rare (less than 0.01%): Anaphylactic reaction, serum sickness-like reaction
- Frequency not reported: Anaphylactoid reactions, necrotizing vasculitis, cutaneous vasculitis[Ref]
Allergic reactions ranged from urticaria to anaphylactic reactions, including life-threatening anaphylactic shock.
At least 2 cases have been reported of patients developing a cutaneous vasculitis related to use of this drug. The vasculitis resolved without medical intervention after the drug was discontinued.
Serum sickness-like reaction and anaphylactic shock (life-threatening) have also been reported during postmarketing experience.[Ref]
Respiratory
- Rare (0.01% to 0.1%): Dyspnea (including asthmatic condition)
- Frequency not reported: Bronchospasm, hemoptysis, laryngeal edema, respiratory arrest, epistaxis, hiccough, pulmonary edema, pleural effusion, pulmonary embolism, respiratory distress, wheeze, cough, upper respiratory tract infection, pharyngitis, nasopharyngitis[Ref]
Endocrine
- Frequency not reported: Gynecomastia[Ref]
Immunologic
- Frequency not reported: Jarisch-Herxheimer reaction[Ref]
Oral ciprofloxacin has been associated with a case of Jarisch-Herxheimer reaction (characterized by hypotension, tachycardia, and disseminated intravascular coagulation) in a 14-year-old female with tickborne relapsing fever.[Ref]
References
1. Ball P (1986) "Ciprofloxacin: an overview of adverse experiences." J Antimicrob Chemother, 18, p. 187-93
2. Campoli-Richards DM, Monk JP, Price A, Benfield P, Todd PA, Ward A (1988) "Ciprofloxacin: a review of its antibacterial activity, pharmacokinetic properties and therapeutic use." Drugs, 35, p. 373-447
3. Norrby SR (1991) "Side-effects of quinolones: comparisons between quinolones and other antibiotics." Eur J Clin Microbiol Infect Dis, 10, p. 378-83
4. (2002) "Product Information. Cipro (ciprofloxacin)." Bayer
5. Heyd A, Haverstock D (2000) "Retrospective analysis of the safety profile of oral and intravenous ciprofloxacin in a geriatric population." Clin Ther, 22, p. 1239-50
6. (2001) "From the Centers for Disease Control and Prevention. Update: adverse events associated with anthrax prophylaxis among postal employees--New Jersey, New York City, and the District of Columbia metropolitan area, 2001." JAMA, 286, p. 2935-6
7. (2004) "Product Information. Cipro XR (ciprofloxacin)." Bayer Pharmaceutical Inc
8. Alexander RB, Propert KJ, Schaeffer AJ, et al. (2004) "Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial." Ann Intern Med, 141, p. 581-9
9. Ramakrishnan K, Scheid DC (2005) "Diagnosis and management of acute pyelonephritis in adults." Am Fam Physician, 71, p. 933-42
10. Fourcroy JL, Berner B, Chiang YK, Cramer M, Rowe L, Shore N (2005) "Efficacy and safety of a novel once-daily extended-release ciprofloxacin tablet formulation for treatment of uncomplicated urinary tract infection in women." Antimicrob Agents Chemother, 49, p. 4137-43
11. Kothur K, Singh M, Dayal D (2006) "Ciprofloxacin-induced anaphylactoid reaction." Eur J Pediatr, 165, p. 573-4
12. Cerner Multum, Inc. "UK Summary of Product Characteristics."
13. Cerner Multum, Inc. "Australian Product Information."
14. Juillerat P, Pittet V, Felley C, et al. (2007) "Drug safety in Crohn's disease therapy." Digestion, 76, p. 161-8
15. Schacht P, Arcieri G, Hullmann R (1989) "Safety of oral ciprofloxacin. An update based on clinical trial results." Am J Med, 87, s98-102
16. Harmon T, Burkhart G, Applebaum H (1992) "Perforated pseudomembranous colitis in the breast-fed infant." J Pediatr Surg, 27, p. 744-6
17. Bauwens JE, McFarland LV, Melcher SA (1997) "Recurrent clostridium difficile disease following ciprofloxacin use." Ann Pharmacother, 31, p. 1090
18. Overholser BR, Kays MB, Forrest A, Sowinski KM (2004) "Sex-related differences in the pharmacokinetics of oral ciprofloxacin." J Clin Pharmacol, 44, p. 1012-22
19. Bilton D, Henig N, Morrissey B, Gotfried M (2006) "Addition of Inhaled Tobramycin to Ciprofloxacin for Acute Exacerbations of Pseudomonas aeruginosa Infection in Adult Bronchiectasis." Chest, 130, p. 1503-10
20. Ferguson J, McEwen J, AlAjmi H, Purkins L, Colman PJ, Willavize SA (2000) "A comparison of the photosensitizing potential of trovafloxacin with that of other quinolones in healthy subjects." J Antimicrob Chemother, 45, p. 503-9
21. KimyaiAsadi A, Usman A, Nousari HC (2000) "Ciprofloxacin-induced bullous pemphigoid." J Am Acad Dermatol, 42, p. 847
22. Knoell KA, Lynch JM (2009) "Photoinduced acute exanthematous pustulosis caused by ciprofloxacin and sunlight exposure." Int J Dermatol, 48, p. 1141-3
23. Arcieri G, Griffith E, Gruenwaldt G, et al. (1988) "A survey of clinical experience with ciprofloxacin, a new quinolone antimicrobial." J Clin Pharmacol, 28, p. 179-89
24. Gasser TC, Ebert SC, Graversen PH, Madsen PO (1987) "Pharmacokinetic study of ciprofloxacin in patients with impaired renal function." Am J Med, 82, p. 139-41
25. Paton JH, Reeves DS (1988) "Fluoroquinolone antibiotics: microbiology, pharmacokinetics and clinical use." Drugs, 36, p. 193-228
26. Fleming LW, Phillips G, Stewart WK, Scott AC (1990) "Oral ciprofloxacin in the treatment of peritonitis in patients on continuous ambulatory peritoneal dialysis." J Antimicrob Chemother, 25, p. 441-8
27. McCue JD, Zandt JR (1991) "Acute psychoses associated with the use of ciprofloxacin and trimethoprim-sulfamethoxazole." Am J Med, 90, p. 528-9
28. Arcieri G, August R, Becker N, et al. (1986) "Clinical experience with ciprofloxacin in the USA." Eur J Clin Microbiol, 5, p. 220-5
29. Altes J, Gasco J, De Antonio J, Villalonga C (1989) "Ciprofloxacin and delirium." Ann Intern Med, 110, p. 170-1
30. Mumford CJ, Ginsberg L (1990) "Ciprofloxacin and myasthenia gravis." BMJ, 301, p. 818
31. McDermott JL, Gideonse N, Campbell JW (1991) "Acute delirium associated with ciprofloxacin administration in a hospitalized elderly patient." J Am Geriatr Soc, 39, p. 909-10
32. Slavich IL, Gleffe Rf, Haas EJ (1989) "Grand mal epileptic seizures during ciprofloxacin therapy." JAMA, 261, p. 558-9
33. Moore B, Safani M, Keesey J (1988) "Possible exacerbation of myasthenia gravis by ciprofloxacin." Lancet, Jan, p. 882
34. Semel JD, Allen N (1991) "Seizures in patients simultaneously receiving theophylline and imipenem or ciprofloxacin or metronidazole." South Med J, 84, p. 465-8
35. Maddix DS, Stefani A (1992) "Myasthenia gravis and ciprofloxacin." Ann Pharmacother, 26, p. 265-6
36. Karki SD, Bentley DW, Raghavan M (1990) "Seizure with ciprofloxacin and theophylline combined therapy." DICP, 24, p. 595-6
37. Schwartz MT, Calvert JF (1990) "Potential neurologic toxicity related to ciprofloxacin." Ann Pharmacother, 24, p. 138-40
38. Akhtar S, Ahmad H (1993) "Ciprofloxacin-induced catatonia." J Clin Psychiatry, 54, p. 115-6
39. Isaacson SH, Carr J, Rowan AJ (1993) "Ciprofloxacin-induced complex partial status epilepticus manifesting as an acute confusional state." Neurology, 43, p. 1619-21
40. Fanhavard P, Sanchorawala V, Oh J, Moser EM, Smith SP (1994) "Concurrent use of foscarnet and ciprofloxacin may increase the propensity for seizures." Ann Pharmacother, 28, p. 869-72
41. Rosolen A, Drigo P, Zanesco L (1994) "Acute hemiparesis associated with ciprofloxacin." BMJ, 309, p. 1411
42. Winrow AP, Supramaniam G (1990) "Benign intracranial hypertension after ciprofloxacin administration." Arch Dis Child, 65, p. 1165-6
43. Pastor P, Moitinho E, Elizalde I, Cirera I, Tolosa E (1996) "Reversible oral-facial dyskinesia in a patient receiving ciprofloxacin hydrochloride." J Neurol, 243, p. 616-7
44. Jay GT, Fitzgerald JM (1997) "Ciprofloxacin-induced delirium." Ann Pharmacother, 31, p. 252
45. Tattevin P, Messiaen T, Pras V, Ronco P, Biour M (1998) "Confusion and general seizures following ciprofloxacin administration." Nephrol Dialysis Transplant, 13, p. 2712-3
46. Kushner JM, Peckman HJ, Snyder CR (2001) "Seizures associated with fluoroquinolones." Ann Pharmacother, 35, p. 1194-8
47. Cohen JS (2001) "Peripheral neuropathy associated with fluoroquinolones." Ann Pharmacother, 35, p. 1540-7
48. Whyte CA, Shivdat-Nanhoe R, Kramer P (2008) "A Case of Amoxicillin-Induced Meningitis." Clin Infect Dis, 46, p. 642
49. Darwish T (2008) "Ciprofloxacin-induced seizures in a healthy patient." N Z Med J, 121, p. 104-5
50. Imrie K, Gold W, Salit I, Keating A (1993) "Ciprofloxacin-induced neutropenia and erythema multiforme." Am J Hematol, 43, p. 159-60
51. Dutta TK, Badhe BA (1999) "Ciprofloxacin-induced bone marrow depression." Postgrad Med J, 75, p. 571-3
52. Andrews PA, Robinson GT (1999) "Intravascular haemolysis and interstitial nephritis in association with ciprofloxacin." Nephron, 83, p. 359-60
53. Oh YR, Carr-Lopez SM, Probasco JM, Crawley PG (2003) "Levofloxacin-induced autoimmune hemolytic anemia." Ann Pharmacother, 37, p. 1010-3
54. Starr JA, Ragucci KR (2005) "Thrombocytopenia associated with intravenous ciprofloxacin." Pharmacotherapy, 25, p. 1030-4
55. Grasmick BK, Lehr VT, Sundareson AS (1992) "Fulminant hepatic failure possibly related to ciprofloxacin." Ann Pharmacother, 26, p. 636-9
56. Fuchs S, Simon Z, Brezis M (1994) "Fatal hepatic failure associated with ciprofloxacin." Lancet, 343, p. 738-9
57. Sherman O, Beizer JL (1994) "Possible ciprofloxacin-induced acute cholestatic jaundice." Ann Pharmacother, 28, p. 1162-4
58. Villenueuve JP, Davies C, Cote J (1995) "Suspected ciprofloxacin-induced hepatotoxicity." Ann Pharmacother, 29, p. 257-9
59. Labowitz JK, Silverman WB (1997) "Cholestatic jaundice induced by ciprofloxacin." Dig Dis Sci, 42, p. 192-4
60. Stratta P, Lazzarich E, Canavese C, Bozzola C, Monga G (2007) "Ciprofloxacin crystal nephropathy." Am J Kidney Dis, 50, p. 330-5
61. Samuelson WM, Pleasants RA, Whitaker MS (1993) "Arthropathy secondary to ciprofloxacin in an adult cystic fibrosis patient." Ann Pharmacother, 27, p. 302-3
62. Donck JB, Segaert MF, Vanrenterghem YF (1994) "Fluoroquinolones and achilles tendinopathy in renal transplant recipients." Transplantation, 58, p. 736-7
63. Alfaham M, Holt ME, Goodchild MC (1987) "Arthropathy in a patient with cystic fibrosis taking ciprofloxacin." Br Med J (Clin Res Ed), 295, p. 699
64. Zabraniecki L, Negrier I, Vergne P, Arnaud M, Bonnet C, Bertin P, Treves R (1996) "Fluoroquinolone induced tendinopathy: report of 6 cases." J Rheumatol, 23, p. 516-20
65. Mcgarvey WC, Singh D, Trevino SG (1996) "Partial achilles tendon ruptures associated with fluoroquinolone antibiotics: a case report and literature review." Foot Ankle Int, 17, p. 496-8
66. Carrasco JM, Garcia B, Andujar C, Garrote F, de Juana P, Bermejo T (1997) "Tendinitis associated with ciprofloxacin." Ann Pharmacother, 31, p. 120
67. Poon CCH, Sundaram NA (1997) "Spontaneous bilateral Achilles tendon rupture associated with ciprofloxacin." Med J Aust, 166, p. 665
68. Khaliq Y, Zhanel GG (2003) "Fluoroquinolone-Associated Tendinopathy: A Critical Review of the Literature." Clin Infect Dis, 36, p. 1404-1410
69. Adverse Drug Reactions Advisory Committee (ADRAC) and the Adverse Drug Reactions Unit of the TGA (2008) Australian Adverse Drug Reactions Bulletin. http://www.tga.gov.au/adr/aadrb/aadr0810.htm
70. Qian Q, Nasr SH, Akogyeram CO, Sethi S (2012) "Myoglobin-associated acute kidney injury in the setting of ciprofloxacin administration." Am J Kidney Dis, 59, p. 462-6
71. Atasoy H, Erdem G, Ceyhan M, Ecevit Z, Kanra G (1995) "Hypertension asociated with ciprofloxacin use in an infant." Ann Pharmacother, 29, p. 1049
72. Frothingham R (2001) "Rates of torsades de pointes associated with ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin." Pharmacotherapy, 21, p. 1468-72
73. Owens RC Jr, Ambrose PG (2002) "Torsades de pointes associated with fluoroquinolones." Pharmacotherapy, 22, 663-8; discussion 668-72
74. Berger RE (2005) "Rates of torsades de pointes associated with ciprofloxacin, ofloxacin, levofloxacin, gatifloxacin, and moxifloxacin." J Urol, 174, p. 165
75. Owens RC Jr, Nolin TD (2006) "Antimicrobial-Associated QT Interval Prolongation: Pointes of Interest." Clin Infect Dis, 43, p. 1603-1611
76. Nair MK, Patel K, Starer PJ (2008) "Ciprofloxacin-induced torsades de pointes in a methadone-dependent patient." Addiction, 103, p. 2062-4
77. Briasoulis A, Agarwal V, Pierce WJ (2011) "QT Prolongation and Torsade de Pointes Induced by Fluoroquinolones: Infrequent Side Effects from Commonly Used Medications." Cardiology, 120, p. 103-110
78. Lapi F, Wilchesky M, Kezouh A, Benisty JI, Ernst P, Suissa S (2012) "Fluoroquinolones and the risk of serious arrhythmia: a population-based study." Clin Infect Dis, 55, p. 1457-65
79. Lin G, Hays DP, Spillane L (2004) "Refractory hypoglycemia from ciprofloxacin and glyburide interaction." J Toxicol Clin Toxicol, 42, p. 295-7
80. Kelesidis T, Canseco E (2010) "Quinolone-induced hypoglycemia: a life-threatening but potentially reversible side effect." Am J Med, 123, e5-6
81. Thorsteinsson SB, Bergan T, Oddsdottir S, Rohwedder R, Holm R (1986) "Crystalluria and ciprofloxacin, influence of urinary pH and hydration." Chemotherapy, 32, p. 408-17
82. Hootkins R, Fenves AZ, Stephens MK (1989) "Acute renal failure secondary to oral ciprofloxacin therapy: a presentation of three cases and a review of the literature." Clin Nephrol, 32, p. 75-8
83. Allon M, Lopez EJ, Min KW (1990) "Acute renal failure due to ciprofloxacin." Arch Intern Med, 150, p. 2187-9
84. Rastogi S, Atkinson JLD, McCarthy JT (1990) "Allergic nephropathy associated with ciprofloxacin." Mayo Clin Proc, 65, p. 987-9
85. Helmink R, Benediktsson H (1990) "Ciprofloxacin-induced allergic interstitial nephritis." Nephron, 55, p. 432-3
86. Simpson J, Watson AR, Mellersh A, Nelson CS, Dodd K (1991) "Typhoid fever, ciprofloxacin, and renal failure." Arch Dis Child, 66, p. 1083-4
87. Gonski PN (1991) "Ciprofloxacin-induced renal failure in an elderly patient." Med J Aust, 154, p. 638-9
88. Rippelmeyer DJ, Synhavsky A (1988) "Ciprofloxacin and allergic interstitial nephritis." Ann Intern Med, 109, p. 170
89. Ying LS, Johnson CA (1989) "Ciprofloxacin-induced interstitial nephritis." Clin Pharm, 8, p. 518-21
90. Murray KM, Wilson MG (1990) "Suspected ciprofloxacin-induced interstitial nephritis." Ann Pharmacother, 24, p. 379-80
91. Hatton J, Haagensen D (1990) "Renal dysfunction associated with ciprofloxacin." Pharmacotherapy, 10, p. 337-40
92. Ortiz A, Plaza JJ, Egido J (1992) "Ciprofloxacin-associated tubulointerstitial nephritis with linear tubular basement membrane deposits." Nephron, 60, p. 248
93. Anand A (1993) "Ciprofloxacin nephrotoxicity." Arch Intern Med, 153, p. 2705-6
94. Lucena MI, Marquez M, Velasco JL, Andrade RJ (1995) "Acute renal failure attributable to ciprofloxacin in a patient with the acquired immunodeficiency syndrome." Arch Intern Med, 155, p. 114
95. Shih DJ, Korbet SM, Rydel JJ, Schwartz MM (1995) "Renal vasculitis associated with ciprofloxacin." Am J Kidney Dis, 26, p. 516-9
96. Choe U, Rothschild BM, Laitman L (1989) "Ciprofloxacin-induced vasculitis." N Engl J Med, 320, p. 257-8
97. Slama TG (1990) "Serum sickness-like illness associated with ciprofloxacin." Antimicrob Agents Chemother, 34, p. 904-5
98. Tomas S, Pedro-Botet J, Auget T (1991) "Ciprofloxacin and immunocomplex-mediated disease." J Intern Med, 230, p. 550-1
99. Stubbings J, Sheehan-Dare R, Walton S (1992) "Cutaneous vasculitis due to ciprofloxacin." BMJ, 305, p. 29
100. Tham TC, Allen G, Hayes D, et al. (1991) "Possible association between toxic epidermal necrolysis and ciprofloxacin." Lancet, 338, p. 522
101. Davis H, Mcgoodwin E, Reed TG (1989) "Anaphylactoid reactions reported after treatment with ciprofloxacin." Ann Intern Med, 111, p. 1041-3
102. Nedorost ST, Dijkstra JW, Handel DW (1989) "Drug-induced photosensitivity reaction." Arch Dermatol, 125, p. 433-4
103. Rodriguez E, Martinez JA, Torres M, Nubiiola A, Buges J (1990) "Lobular panniculitis associated with ciprofloxacin." Br Med J, 300, p. 1468
104. Peters B, Pinching AJ (1989) "Fatal anaphylaxis associated with ciprofloxacin in a patient with AIDS related complex." BMJ, 298, p. 605
105. Granowitz EV (1989) "Photosensitivity rash in a patient being treated with ciprofloxacin." J Infect Dis, 160, p. 910-1
106. Wurtz RM, Abrams D, Becker S, Jacobson MA, Mass MM, Marks SH (1989) "Anaphylactoid drug reactions to ciprofloxacin and rifampicin in HIV-infected patients." Lancet, 1, p. 955-6
107. Kennedy CA, Goetz MB, Mathisen GE (1990) "Ciprofloxacin-induced anaphylactoid reactions in patients infected with the human immunodeficiency virus." West J Med, 153, p. 563-4
108. Miller MS, Gaido F, Rourk MH Jr, Spock A (1991) "Anaphylactoid reactions to ciproflaxacin in cystic fibrosis patients." Pediatr Infect Dis J, 10, p. 164-5
109. Berger TG, Franklin N (1992) "Anaphylactoid reaction to ciprofloxacin in a patient infected with the human immunodeficiency virus." J Am Acad Dermatol, 26, p. 256-7
110. Win A, Evers ML, Chmel H (1994) "Stevens-johnson syndrome presumably induced by ciprofloxacin." Int J Dermatol, 33, p. 512-4
111. Roujeau JC, Kelly JP, Naldi L, et al. (1995) "Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis." N Engl J Med, 333, p. 1600-7
112. Lieu PK, Tok SC, Ismail NH, Chng HH (1997) "Ciproflaxin-induced cutaneous vasculitis." Allergy, 52, p. 593-4
113. Reano M, Vives R, Rodriguez J, Daroca P, Canto G, Fernandez J (1997) "Ciprofloxacin-induced vasculitis." Allergy, 52, p. 599-600
114. Ho DY, Song JC, Wang CC (2003) "Anaphylactoid reaction to ciprofloxacin." Ann Pharmacother, 37, p. 1018-23
115. Tierney BC, Martin SW, Franzke LH, et al. (2003) "Serious Adverse Events among Participants in the Centers for Disease Control and Prevention's Anthrax Vaccine and Antimicrobial Availability Program for Persons at Risk for Bioterrorism-Related Inhalational Anthrax." Clin Infect Dis, 37, p. 905-11
116. Hallgren J, Tengvall-Linder M, Persson M, Wahlgren CF (2003) "Stevens-Johnson syndrome associated with ciprofloxacin: A review of adverse cutaneous events reported in Sweden as associated with this drug." J Am Acad Dermatol, 49(5 Suppl), p. 267-9
117. Jongen-Lavrencic M, Schneeberger PM, van der Hoeven JG (2003) "Ciprofloxacin-induced toxic epidermal necrolysis in a patient with systemic lupus erythematosus." Infection, 31, p. 428-9
118. Maunz G, Conzett T, Zimmerli W (2009) "Cutaneous vasculitis associated with fluoroquinolones." Infection, 37, p. 466-8
Frequently asked questions
- How long does ciprofloxacin stay in your system when finished?
- How long does Cipro take to work?
- What is the best antibiotic to treat a sinus infection?
- What medications can affect your taste or smell?
- What antibiotics are used to treat UTI?
- Ciprofloxacin - can you crush Cipro 500 tablets and mix with food?
More about Proquin XR (ciprofloxacin)
- Check interactions
- Compare alternatives
- Reviews (1)
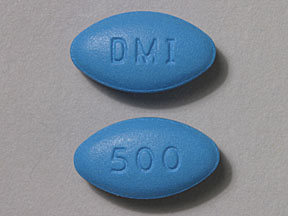
- Drug images
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Proquin XR side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.