Moricizine Side Effects
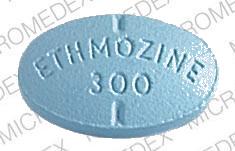
Applies to moricizine: oral tablet.
Important warnings
This medicine can cause some serious health issues
Oral route (tablet)
Considering the known proarrhythmic properties of moricizine and the lack of evidence of improved survival for any antiarrhythmic drug in patients without life-threatening arrhythmias, the use of moricizine, as well as other antiarrhythmic agents, should be reserved for patients with life-threatening ventricular arrhythmias.
Common side effects of moricizine
Some side effects of moricizine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- dizziness
Less common
Serious side effects of moricizine
Along with its needed effects, moricizine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking moricizine:
Less common
- chest pain
- fast or irregular heartbeat
- shortness of breath
- swelling of the feet or lower legs
Rare
- fever (sudden, high)
For healthcare professionals
Applies to moricizine: oral tablet.
General
Generally, cardiovascular effects have been reported most frequently. Noncardiac side effects occur in up to 45% of patients, usually in the first one or two weeks of therapy.[Ref]
Gastrointestinal
Gastrointestinal side effects occurred in up to 34% of patients, usually manifesting as nausea (10% to 34%), vomiting or diarrhea (2%), and abdominal discomfort (3%). Gastrointestinal effects were included in adverse reactions leading to discontinuation of therapy in 7% of patients. Anorexia, bitter taste, dysphagia, flatulence, and ileus have been reported.[Ref]
Nervous system
One case of increased parkinsonism has been reported. Moricizine is a phenothiazine derivative and suspected of exacerbating or inducing parkinsonian symptoms.[Ref]
Nervous system side effects have usually manifest as dose-related dizziness (15%) and headache (8%). Other nervous system side effects included hypoesthesias (4%), paresthesias (2%), anxiety (3%), fatigue (1%), and sleep disorders (2%). Tremor, abnormal gait and coordination, ataxia, dyskinesia, confusion, somnolence, agitation, seizure, coma, speech disorder, and loss of memory have been reported.[Ref]
Hematologic
Hematologic side effects have been rare, but have include thrombocytopenia.[Ref]
No evidence of bone marrow toxicity was present in the rare reports of thrombocytopenia. Patients were on other drugs with thrombocytopenia-associated potential.[Ref]
Hepatic
Hepatic side effects, such as transiently elevated liver function tests, have been reported.[Ref]
Genitourinary
Genitourinary side effects including urinary retention or frequency, incontinence, impotence and decreased libido occurred in less than 2% of patients.[Ref]
Genitourinary side effects may be related to the chemical similarity of moricizine to phenothiazines. Phenothiazines can cause urinary retention.[Ref]
Other
Drug fever, confirmed by rechallenge, has been reported in three patients. Hypothermia and temperature intolerance have occurred. Vertigo and tinnitus have been reported.[Ref]
Hypersensitivity
Hypersensitivity side effects such as rash, pruritus, urticaria, swelling of the lips and tongue and periorbital edema have been reported.[Ref]
Cardiovascular
Cardiovascular side effects have included exacerbation of old or induction of new atrial and ventricular arrhythmias (2% to 12%), heart failure (2%), hypotension (1%), and syncope (1%). Moricizine-induced arrhythmias may be lethal and more refractory to conversion to sinus rhythm than nondrug-induced arrhythmias. To reduce the proarrhythmic effect, it is recommended that the serum potassium, calcium, and magnesium concentrations be within normal limits prior to moricizine therapy.
Alteration in ventricular conduction, including new bundle branch patterns, has occurred in approximately 9.4% of patients. Second-degree heart block has occurred in patients without baseline conduction abnormalities (0.2%) as well as those with preexisting abnormalities (0.9%). Third-degree heartblock has been reported in 1.4% of patients with baseline conduction dysfunction.
Independent risk factors for the development of moricizine cardiotoxicity are advanced age, coronary artery disease, a history of myocardial infarction, low left ventricular ejection fraction (less than 0.40), and congestive heart failure.
Other cardiovascular effects have included hypertension, chest pain, congestive heart failure, myocardial infarction, vasodilation and thrombophlebitis.[Ref]
The multicenter Cardiac Arrhythmias Suppression Trial (CAST) failed to show improved survival during use of moricizine to treat asymptomatic or mildly asymptomatic premature ventricular depolarizations in patients with a recent history of myocardial infarction.
In a prospective study using maximal dosages of moricizine (mean 831 mg per day) in 31 patients with a history of sustained ventricular tachyarrhythmias (mean ejection fraction 0.39), a significant proarrhythmic effect and lack of efficacy were observed. Six of the 31 experienced ventricular proarrhythmias within four days. Of the remaining 25 patients, 24 underwent electrophysiologic testing and four were found to be noninducible (16% efficacy). Seven patients were discharged on moricizine therapy. One patient developed a ventricular proarrhythmia, one developed complete AV heart block, and two experienced recurrent ventricular tachycardia.[Ref]
Psychiatric
Psychiatric symptoms of depression, euphoria, and hallucinations have been reported.[Ref]
Ocular
Ocular side effects including nystagmus, diplopia, pain, and blurred vision have occurred.[Ref]
Respiratory
Respiratory side effects including pulmonary embolism, hyperventilation, apnea, asthma, pharyngitis, cough, and sinusitis have been reported.[Ref]
Dermatologic
Dermatologic symptoms of dry skin and rash have been reported.[Ref]
References
1. Morganroth J, Pratt CM (1989) "Prevalence and characteristics of proarrhythmia from moricizine (themozine)." Am J Cardiol, 63, p. 172-6
2. Damle R, Levine J, Matos J, et al. (1992) "Efficacy and risks of moricizine in inducible sustained ventricular tachycardia." Ann Intern Med, 116, p. 375-81
3. Clyne CA, Estes NA, Wang PJ (1992) "Moricizine." N Engl J Med, 327, p. 255-60
4. Podrid PJ, Beau SL (1990) "Antiarrhythmic drug therapy for congestive heart failure with focus on moricizine." Am J Cardiol, 65, d56-64
5. Kennedy HL (1990) "Noncardiac adverse effects and organ toxicity of moricizine during short- and long-term studies." Am J Cardiol, 65, d47-50
6. (2002) "Product Information. Ethmozine (moricizine)." DuPont Pharmaceuticals
7. Bhandari AK, Lerman R, Ehrlich S, Sager P, Leon C, Widerhorn J, Cannom DS (1993) "Electrophysiological evaluation of moricizine in patients with sustained ventricular tachyarrhythmias: low efficacy and high incidence of proarrhythmia." Pacing Clin Electrophysiol, 16, p. 1853-61
8. Peters RW, Mitchell LB, Brooks MM, Echt DS, Barker AH, Capone R, Liebson PR, Greene HL (1994) "Circadian pattern of arrhythmic death in patients receiving encainide, flecainide or moricizine in the cardiac arrhythmia suppression trial (CAST)." J Am Coll Cardiol, 23, p. 283-9
9. Roden DM (1994) "Risks and benefits of antiarrhythmic therapy." N Engl J Med, 331, p. 785-91
10. Anderson JL, Platia EV, Hallstrom A, Henthorn RW, Buckingham TA, Carlson MD, Carson PE (1994) "Interaction of baseline characteristics with the hazard of encainide, flecainide, and moricizine therapy in patients with myocardial infarction: a possible explanation for increased mortality in the cardiac arrhythmia suppression trial (CAST)." Circulation, 90, p. 2843-52
11. Pratt CM, Wierman A, Seals AA, et al. (1986) "Efficacy and safety of moricizine in patients with ventricular tachycardis: results of a placebo-controlled prospective long-term clinical trial." Circulation, 73, p. 718-26
More about moricizine
- Check interactions
- Compare alternatives
- Reviews (1)
- Dosage information
- During pregnancy
- Drug class: group I antiarrhythmics
Professional resources
Other brands
Related treatment guides
Further information
Moricizine side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.