Enbrel Side Effects
Generic name: etanercept
Note: This document contains side effect information about etanercept. Some dosage forms listed on this page may not apply to the brand name Enbrel.
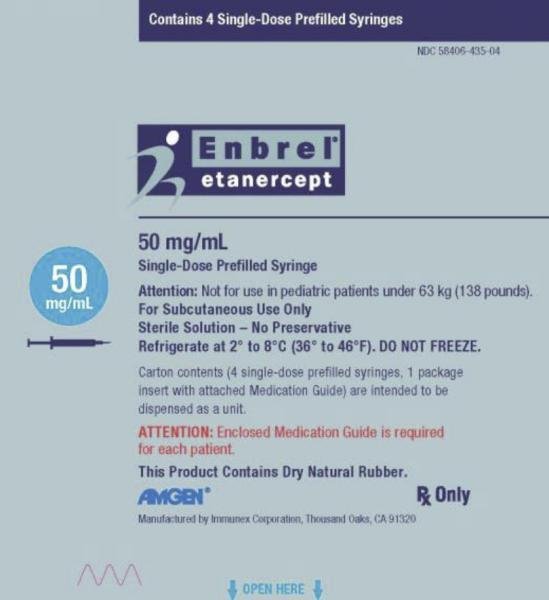
Applies to etanercept: subcutaneous solution.
Warning
Subcutaneous route (Solution; Powder for Solution)
Serious Infections: Patients treated with etanercept are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids. Etanercept should be discontinued if a patient develops a serious infection or sepsis.Reported Infections include: (1) Active tuberculosis, including reactivation of latent tuberculosis. Patients with tuberculosis have frequently presented with disseminated or extrapulmonary disease. Test patients for latent tuberculosis before etanercept use and during therapy. Initiate treatment for latent infection prior to etanercept use. (2) Invasive fungal infections, including histoplasmosis, coccidioidomycosis, candidiasis, aspergillosis, blastomycosis, and pneumocystosis. Patients with histoplasmosis or other invasive fungal infections may present with disseminated, rather than localized, disease. Antigen and antibody testing for histoplasmosis may be negative in some patients with active infection. Consider empiric anti-fungal therapy in patients at risk for invasive fungal infections who develop severe systemic illness. (3) Bacterial, viral, and other infections due to opportunistic pathogens, including Legionella and Listeria.The risks and benefits of treatment with etanercept should be carefully considered prior to initiating therapy in patients with chronic or recurrent infection. Monitor patients closely for the development of signs and symptoms of infection during and after treatment with etanercept, including the possible development of tuberculosis in patients who tested negative for latent tuberculosis infection prior to initiating therapy.Malignancies: Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with tumor necrosis factor (TNF) blockers, including etanercept.
Subcutaneous route (Solution)
Patients treated with etanercept products are at increased risk for infections, some progressing to serious infections leading to hospitalization or death. These infections have included bacterial sepsis, tuberculosis, invasive fungal and other opportunistic infections, including Legionella and Listeria. Evaluate for latent tuberculosis and treat if necessary prior to initiation of therapy. Discontinue etanercept-szzs if a serious infection or sepsis occurs during treatment. Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with tumor necrosis factor (TNF) blockers, including etanercept products.
Subcutaneous route (Solution)
Serious InfectionsIncreased risk of serious infections leading to hospitalization or death, including tuberculosis (TB), bacterial sepsis, invasive fungal infections (such as histoplasmosis), and infections due to other opportunistic pathogens.Etanercept-ykro should be discontinued if a patient develops a serious infection or sepsis during treatment.Perform test for latent TB; if positive, start treatment for TB prior to starting etanercept-ykro.Monitor all patients for active TB during treatment, even if initial latent TB test is negative.MalignanciesLymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with TNF blockers, including etanercept products.
Serious side effects of Enbrel
Along with its needed effects, etanercept (the active ingredient contained in Enbrel) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking etanercept:
More common
- Chills
- cough
- fever
- sneezing
- sore throat
Less common
- Chest tightness
- depression
- fast heartbeat
- frequent or painful urination
- itching, pain, redness, or swelling on the skin
- joint or muscle stiffness, tightness, or rigidity
- stomach discomfort or pain
Incidence not known
- Bladder pain
- blistering, peeling, or loosening of the skin
- bloody, black, or tarry stools
- blue-yellow color blindness
- blurred vision
- chest discomfort or pain
- cloudy or bloody urine
- confusion
- dark urine
- decreased urine output
- decreased vision
- diarrhea
- difficult, irregular, troubled, or labored breathing (or difficulty with breathing gets worse)
- difficulty with moving
- dilated neck veins
- double vision
- extreme fatigue
- eye pain
- feeling sad or empty
- fruit-like breath odor
- general feeling of discomfort, illness, or weakness
- generalized pain
- heartburn
- high blood pressure
- inability to move the arms, legs, or facial muscles
- indigestion
- irregular heartbeat
- joint or muscle pain
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- lightheadedness
- loss of consciousness
- muscle tenderness
- pain or discomfort in the arms, jaw, back, or neck
- pain, redness, or swelling in the arm or leg
- problems with bowel or bladder function
- red skin lesions, often with a purple center
- red, scaling, or crusted skin
- seizures
- severe and continuing nausea
- severe numbness, especially on one side of the face or body
- sores, ulcers, or white spots on the lips or in the mouth
- swelling of the face, fingers, feet, or lower legs
- tenderness
- trouble concentrating
- trouble sleeping
- unexplained weight loss
- unusual bleeding or bruising
- unusual tiredness or weakness
- vomiting of blood or material that looks like coffee grounds
- weight loss
- yellow eyes or skin
Other side effects of Enbrel
Some side effects of etanercept may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Loss of energy or weakness
- nausea
- pain or burning in the throat
- redness or itching, pain, or swelling at the injection site (under the skin)
- runny or stuffy nose
- stomach pain
- vomiting
Less common
- Bumps below the skin
- dry eyes
- dry mouth
- hair loss or thinning
- irritation or soreness of the mouth
- itching, redness, or tearing of the eye
- skin rash
Incidence not known
- Altered sense of taste
- burning, crawling, itching, numb, prickling, “pins and needles”, or tingling feelings
- feeling faint, dizzy, or lightheaded
- feeling of warmth or heat
- flushing or redness of the skin, especially on the face and neck
- loss of appetite
- sweating
- weight gain
For Healthcare Professionals
Applies to etanercept: subcutaneous kit, subcutaneous solution.
Respiratory
Very common (10% or more): Non-upper respiratory infection (38%), upper respiratory infection (29%), rhinitis (12%)
Common (1% to 10%): Pharyngitis, cough, respiratory disorder, sinusitis
Uncommon (0.1% to 1%): Interstitial lung disease (including pneumonitis and pulmonary fibrosis)[Ref]
Immunologic
Very common (10% or more): Infections (including upper respiratory tract infections, bronchitis, cystitis, skin infections)
Uncommon (0.1% to 1%): Serious infections (including pneumonia, cellulitis, septic arthritis, sepsis, parasitic infection)
Rare (less than 0.1%): Tuberculosis, opportunistic infections (including invasive fungal, protozoal, bacterial, atypical mycobacterial, viral infections, Legionella), subacute cutaneous lupus erythematosus, discoid lupus erythematosus, lupus-like syndrome
Frequency not reported: Listeria, hepatitis B reactivation
Postmarketing reports: Macrophage activation syndrome, systemic vasculitis, sarcoidosis[Ref]
Nervous system
Very common (10% or more): Headache (17%)
Common (1% to 10%): Dizziness
Rare (less than 0.1%): Seizures, CNS demyelinating events suggestive of multiple sclerosis or localized demyelinating conditions, such as optic neuritis and transverse myelitis
Very rare (less than 0.01%): Peripheral demyelinating events (including Guillain-Barre syndrome, chronic inflammatory demyelinating polyneuropathy, demyelinating polyneuropathy, multifocal motor neuropathy)
Postmarketing reports: Paresthesias[Ref]
Gastrointestinal
Common (1% to 10%): Abdominal pain, dyspepsia, diarrhea, nausea, vomiting, mouth ulcers, altered sense of taste, esophagitis, gastritis
Uncommon (0.1% to 1%): Dry mouth
Rare (less than 0.1%): Anorexia
Frequency not reported: Intestinal perforation
Postmarketing reports: Inflammatory bowel disease (IBD)[Ref]
Cardiovascular
Rare (less than 0.1%): Worsening of congestive heart failure
Postmarketing reports: Chest pain[Ref]
Dermatologic
Common (1% to 10%): Pruritus, rash
Uncommon (0.1% to 1%): Angioedema, urticaria, rash, psoriasiform rash, psoriasis (including new onset or worsening and pustular, primarily palms and soles)
Rare (less than 0.1%): Cutaneous vasculitis (including leukocytoclastic vasculitis), Stevens-Johnson syndrome, erythema multiforme
Very rare (less than 0.01%): Toxic epidermal necrolysis
Postmarketing reports: Angioedema[Ref]
Local
Very common (10% or more): Injection site reactions (including bleeding, bruising, erythema, itching, pain, swelling)[Ref]
Hematologic
Uncommon (0.1% to 1%): Thrombocytopenia
Rare (less than 0.1%): Anemia, leukopenia, neutropenia, pancytopenia
Very rare (less than 0.01%): Aplastic anemia
Postmarketing reports: Lymphadenopathy[Ref]
Ocular
Uncommon (0.1% to 1%): Uveitis, scleritis
Rare (less than 0.1%): Inflammation, dry eyes[Ref]
Hypersensitivity
Common (1% to 10%): Allergic reactions, autoantibody formation
Uncommon (0.1% to 1%): Systemic vasculitis (including anti-neutrophilic cytoplasmic antibody positive vasculitis)
Rare (less than 0.1%): Serious allergic/anaphylactic reactions (including angioedema, bronchospasm), sarcoidosis
Frequency not reported: Macrophage activation syndrome, worsening of symptoms of dermatomyositis[Ref]
Oncologic
Uncommon (0.1% to 1%): Non-melanoma skin cancers
Rare (less than 0.1%): Lymphoma, melanoma
Frequency not reported: Leukemia, Merkel cell carcinoma, leukemia[Ref]
Hepatic
Rare (less than 0.1%): Elevated liver enzymes, autoimmune hepatitis
Postmarketing reports: Hepatitis B reactivation[Ref]
Genitourinary
Frequency not reported: Urinary tract infection[Ref]
Renal
Renal side effects including pyelonephritis have been reported. At least one case of necrotizing crescentic glomerulonephritis has been reported, in addition to a case of proliferative lupus nephritis.
Other
Common (1% to 10%): Fever, asthenia[Ref]
General
The most commonly reported adverse reactions are injection site reactions (such as pain, swelling, itching, reddening and bleeding at the puncture site), infections (such as upper respiratory infections, bronchitis, bladder infections and skin infections), allergic reactions, development of autoantibodies, itching, and fever.[Ref]
Frequently asked questions
- Does perispinal etanercept work for stroke recovery?
- What are the new drugs for rheumatoid arthritis (RA)?
- What are biosimilar drugs?
- Which foods should be avoided while taking Enbrel?
- How long does it take for Enbrel (etanercept) to work?
- How long can Enbrel (etanercept) be left unrefrigerated?
- Can Enbrel (etanercept) be taken with antibiotics?
- Can you take Enbrel (etanercept) with a cold?
- What are the new drugs for plaque psoriasis?
More about Enbrel (etanercept)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (305)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Support group
- FDA approval history
- Drug class: antirheumatics
- Breastfeeding
Patient resources
- Enbrel drug information
- Enbrel SureClick
- Enbrel (Etanercept Prefilled Syringes)
- Enbrel (Etanercept Vials)
Other brands
Professional resources
Other brands
Related treatment guides
References
1. Product Information. Enbrel (etanercept). Wyeth-Ayerst Laboratories. 2001;PROD.
2. Cerner Multum, Inc. UK Summary of Product Characteristics.
3. Pharmaceutical Society of Australia. APPGuide online. Australian prescription products guide online. http://www.appco.com.au/appguide/default.asp 2006.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.