Celecoxib / tramadol Side Effects
Medically reviewed by Drugs.com. Last updated on Jan 26, 2024.
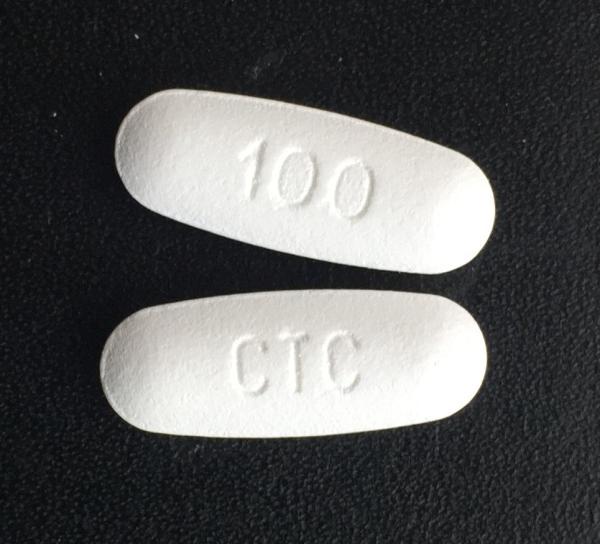
Applies to celecoxib / tramadol: oral tablet.
Warning
Oral route (Tablet)
Addiction, Abuse, and MisuseCelecoxib/traMADol exposes patients and other users to the risk of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing celecoxib/traMADol and monitor all patients regularly for the development of these behaviors and conditions.Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to healthcare providers. Healthcare providers are strongly encouraged to: complete a REMS-compliant education program, counsel patients and/or caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products, emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist, and consider other tools to improve patient, household, and community safety.Life-Threatening Respiratory DepressionSerious, life-threatening, or fatal respiratory depression may occur with use of celecoxib/traMADol. Monitor for respiratory depression, especially during initiation of celecoxib/traMADol.Accidental IngestionAccidental ingestion of even one dose celecoxib/traMADol, especially by children, can be fatal.Cardiovascular Thrombotic EventsNonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction, and stroke, which can be fatal. This risk may occur early in the treatment and may increase with duration of use.Celecoxib/traMADol is contraindicated in the setting of coronary artery bypass graft (CABG) surgery.Gastrointestinal Bleeding, Ulceration, and PerforationNSAIDs cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients and patients with a prior history of peptic ulcer disease and/or GI bleeding are at greater risk for serious (GI) events.Ultra-Rapid Metabolism of TraMADol and Other Risk Factors for Life-Threatening Respiratory Depression in ChildrenLife-threatening respiratory depression and death have occurred in children who received traMADol. Some of the reported cases followed tonsillectomy and/or adenoidectomy; in at lease one case, the child had evidence of being an ultra-rapid metabolizer of traMADol due to a CYP2D6 polymorphism. Celecoxib/traMADol is contraindicated in children younger than 12 years of age an in children younger than 18 years of age following tonsillectomy and/or adenoidectomy. Avoid use of celecoxib/traMADol in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of traMADol.Neonatal Opioid Withdrawal SyndromeProlonged use of celecoxib/traMADol during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.Interactions with Drugs Affecting Cytochrome P450 IsoenzymesThe effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with traMADol are complex. Use of cytochrome P450 P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with celecoxib/traMADol requires careful consideration of the effects on the parent drug, traMADol, and the active metabolite, M1.Risks from Concomitant Use with Benzodiazepines or Other CNS DepressantsConcomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death.Reserve concomitant prescribing of celecoxib/traMADol and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate.Limit treatment to the minimum duration.Follow patients for signs and symptoms of respiratory depression and sedation.
Serious side effects
Along with its needed effects, celecoxib / tramadol may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking celecoxib / tramadol:
Incidence not known
- Agitation
- anxiety
- bigger, dilated, or enlarged pupils (black part of eye)
- black, tarry stools
- blistering, peeling, or loosening of the skin
- bloating of the stomach
- bloody or cloudy urine
- blurred vision
- chest pain, discomfort, or tightness
- chills
- cold sweats
- coma
- confusion
- confusion as to time, place, or person
- constricted, pinpoint, or small pupils (black part of eye)
- cool, pale skin
- cough or hoarseness
- dark urine
- darkening of the skin
- depression
- diarrhea
- difficulty in speaking
- difficulty swallowing
- dizziness
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fainting
- fast heartbeat
- fever
- greatly decreased frequency of urination or amount of urine
- hallucinations
- headache, sudden or severe
- heartburn
- hives, itching, skin rash
- holding false beliefs that cannot be changed by fact
- increased hunger
- increased sensitivity of the eyes to light
- increased thirst
- indigestion
- irregular or slow heart rate
- joint or muscle pain
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- light-colored stools
- loss of appetite
- loss of sense of smell or taste
- lower back or side pain
- mental depression
- muscle pain or cramps
- nausea
- nervousness
- nightmares
- numbness or tingling in the hands, feet, or lips
- overactive reflexes
- pain, redness, or swelling in the arm or leg
- painful or difficult urination
- pain or discomfort in the arms, jaw, back, or neck
- pale or blue lips, fingernails, or skin
- poor coordination
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- red irritated eyes
- red skin lesions, often with a purple center
- seizures
- shakiness
- shivering
- slurred speech
- sore throat
- sores, ulcers, or white spots on the lips or in the mouth
- stiff neck or back
- stomach cramps or pain
- sweating
- swelling of the face, ankles, or hands
- swelling of the feet or lower legs
- swollen glands
- talking or acting with excitement you cannot control
- trouble breathing
- twitching
- unpleasant breath odor
- unusual bleeding or bruising
- unusual excitement, nervousness, or restlessness
- unusual or incomplete body or facial movements
- unusual tiredness or weakness
- vomiting
- vomiting of blood or material that looks like coffee grounds
- weakness or heaviness of the legs
- weight gain
- yellow eyes or skin
Get emergency help immediately if any of the following symptoms of overdose occur while taking celecoxib / tramadol:
Symptoms of overdose
- Black, tarry stools
- dark urine
- depression
- disorientation
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- drowsiness to profound coma
- fever
- headache
- irregular, fast or slow, or shallow breathing
- lightheadedness
- loss of appetite
- mood or other mental changes
- nausea
- pale or blue lips, fingernails, or skin
- seeing, hearing, or feeling things that are not there
- stomach pain
- trouble sleeping
- unpleasant breath odor
- unusual drowsiness, dullness, tiredness, weakness, or feeling of sluggishness
- vomiting of blood
- yellow eyes or skin
For Healthcare Professionals
Applies to celecoxib / tramadol: oral tablet.
General
In a post-bunionectomy acute pain trial, patients received this combination drug (200 mg every 12 hours), celecoxib (100 mg every 12 hours), tramadol (50 mg every 6 hours), or placebo orally for 48 hours. The most common side effects reported with this combination drug were nausea, vomiting, dizziness, headache, and somnolence. Discontinuation due to side effects occurred in 1.6% of patients treated with this combination drug (3 out of 183); the side effects that led to discontinuation included nausea and pruritus/rash.[Ref]
Gastrointestinal
Very common (10% or more): Nausea (30.1%), vomiting (15.8%)
Celecoxib:
-Very common (10% or more): Nausea (16.5%)
-Common (1% to 10%): Vomiting
-Frequency not reported: Serious gastrointestinal adverse events (including inflammation, bleeding, ulceration, perforation of the esophagus/stomach/small intestine/large intestine)
Tramadol:
-Very common (10% or more): Nausea (37.7%), vomiting (16.4%)
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
-Frequency not reported: Serious upper gastrointestinal adverse events (including ulcers, gross bleeding, perforation), complicated symptomatic ulcer[Ref]
Nervous system
Very common (10% or more): Dizziness (16.9%), headache (11.5%)
Common (1% to 10%): Somnolence
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Aseptic meningitis, ageusia, anosmia, fatal intracranial hemorrhage, movement disorder, speech disorder
Celecoxib:
-Very common (10% or more): Headache (11%)
-Common (1% to 10%): Dizziness, somnolence
-Frequency not reported: Stroke
Tramadol:
-Very common (10% or more): Dizziness (18.6%), headache (18%)
-Common (1% to 10%): Somnolence
-Frequency not reported: Sedation, serotonin syndrome, seizures
Opioids:
-Postmarketing reports: Serotonin syndrome[Ref]
Serotonin syndrome has been reported during concomitant use of opioids (including tramadol) with serotonergic drugs.[Ref]
Metabolic
Common (1% to 10%): Decreased appetite
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Hypoglycemia, hyponatremia
Celecoxib:
-Uncommon (0.1% to 1%): Decreased appetite
Tramadol:
-Common (1% to 10%): Decreased appetite
-Postmarketing reports: Hypoglycemia, hyponatremia
NSAIDs:
-Frequency not reported: Fluid retention, increased serum potassium level (including hyperkalemia)[Ref]
Cases of tramadol-associated hypoglycemia have been reported, some resulted in hospitalization. In most cases, patients had predisposing risk factors (including diabetes, renal insufficiency) or were elderly.
Hyponatremia (serum sodium less than 135 mmol/L) has been reported with the use of tramadol; many cases were severe (sodium level less than 120 mmol/L). Most cases of hyponatremia occurred in females older than 65 years and within the first week of therapy.[Ref]
Respiratory
Serious, life-threatening, or fatal respiratory depression has been reported with opioid use, even when used as recommended.[Ref]
Opioids:
Frequency not reported: Respiratory depression, sleep-related breathing disorders (including central sleep apnea, sleep-related hypoxemia)[Ref]
Other
Tramadol:
-Frequency not reported: Death, overdose, withdrawal syndrome
Celecoxib:
-Common (1% to 10%): Peripheral edema
NSAIDs:
-Frequency not reported: Edema[Ref]
Hepatic
In controlled clinical trials of celecoxib, borderline elevations (at least 1.2 times and less than 3 times the upper limit of normal) of liver associated enzymes were reported in 6% of patients taking celecoxib and 5% of patients taking placebo; notable elevations of ALT and AST were reported in about 0.2% of patients taking celecoxib and 0.3% of patients taking placebo.[Ref]
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Liver necrosis, hepatitis, jaundice, hepatic failure
Celecoxib:
-Common (1% to 10%): Elevated liver associated enzymes
-Uncommon (0.1% to 1%): Elevated ALT, elevated AST
NSAIDs:
-Frequency not reported: Elevated ALT, elevated AST, severe hepatic injury (including fulminant hepatitis)[Ref]
Hematologic
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Agranulocytosis, aplastic anemia, pancytopenia, leukopenia
Celecoxib:
-Uncommon (0.1% to 1%): Anemia
NSAIDs:
-Frequency not reported: Anemia[Ref]
Cardiovascular
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Vasculitis, deep venous thrombosis
Celecoxib:
-Frequency not reported: Cardiovascular death (including hemorrhagic death), myocardial infarction
Tramadol:
-Postmarketing reports: QT prolongation, torsade de pointes[Ref]
Cases of QT prolongation and/or torsade de pointes have been reported with tramadol use. Many of these cases were reported in patients taking another drug labeled for QT prolongation, in patients with a risk factor for QT prolongation (e.g., hypokalemia), or in the overdose setting.[Ref]
Dermatologic
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Angioedema
Celecoxib:
-Frequency not reported: Serious skin reactions (including erythema multiforme, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms [DRESS], acute generalized exanthematous pustulosis)
NSAIDs:
-Frequency not reported: DRESS (including fatal or life-threatening cases)[Ref]
Hypersensitivity
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Anaphylactoid reaction
Celecoxib:
-Frequency not reported: Anaphylactic reactions
Tramadol:
-Frequency not reported: Anaphylactic reactions, other allergic reactions (including pruritus, hives, bronchospasm, angioedema, toxic epidermal necrolysis, Stevens-Johnson syndrome)[Ref]
Ocular
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Miosis, mydriasis[Ref]
Psychiatric
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Delirium[Ref]
Renal
Celecoxib- or Tramadol-Containing Products:
-Postmarketing reports: Interstitial nephritis
NSAIDs:
-Frequency not reported: Renal papillary necrosis, other renal injury[Ref]
Endocrine
Tramadol:
-Postmarketing reports: Syndrome of inappropriate antidiuretic hormone secretion (SIADH)
Opioids:
-Postmarketing reports: Adrenal insufficiency, androgen deficiency[Ref]
Cases of SIADH have been reported in patients taking tramadol, most often in females older than 65 years, and within the first week of therapy.
Cases of adrenal insufficiency have been reported with opioid use, more often when used beyond 1 month. Cases of androgen deficiency have occurred with chronic opioid use.[Ref]
More about celecoxib / tramadol
- Check interactions
- Compare alternatives
- Reviews (1)
- Dosage information
- During pregnancy
- Drug class: narcotic analgesic combinations
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
References
1. Product Information. Seglentis (celecoxib-tramadol). Kowa Pharmaceuticals America (formerly ProEthic). 2022.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.