Ritonavir (Monograph)
Brand name: Norvir
Drug class: HIV Protease Inhibitors
Warning
- Risk of Serious Adverse Reactions Due to Drug Interactions
-
Concomitant use with certain classes of drugs, including sedative hypnotics, antiarrhythmics, or ergot alkaloids may result in potentially serious and/or life-threatening events due to possible effects of ritonavir on hepatic metabolism of the drugs. Review medications taken by patient before prescribing ritonavir or when prescribing other drugs for a patient already receiving ritonavir.
Introduction
Antiretroviral; HIV protease inhibitor (PI).
Uses for Ritonavir
Treatment of HIV Infection
Treatment of HIV-1 infection in adults, adolescents, and pediatric patients >1 month of age; used in conjunction with other antiretrovirals.
Regimens containing full-dose ritonavir or ritonavir as the sole PI are no longer recommended for initial treatment because of high pill burden, GI intolerance, and metabolic toxicity.
Low-dose ritonavir is commonly used in conjunction with other PIs as a pharmacokinetic enhancer (booster) to decrease metabolism of and increase plasma concentrations of the other PI; consult guidelines for the most current information on recommended regimens. Selection of an initial antiretroviral regimen should be individualized based on factors such as virologic efficacy, toxicity, pill burden, dosing frequency, drug-drug interaction potential, resistance test results, comorbid conditions, access, and cost.
Postexposure Prophylaxis following Occupational Exposure to HIV (PEP)
Postexposure prophylaxis of HIV infection following occupational exposure† [off-label] (PEP) in health-care personnel and others exposed via percutaneous injury (e.g., needlestick, cut with sharp object) or mucous membrane or nonintact skin (e.g., chapped, abraded, dermatitis) contact with blood, tissue, or other body fluids that might contain HIV.
USPHS recommends 3-drug regimen of raltegravir in conjunction with emtricitabine and tenofovir disoproxil fumarate (tenofovir DF) as the preferred regimen for PEP following occupational exposures to HIV. Several alternative regimens that include an integrase strand transfer inhibitor (INSTI), nonnucleoside reverse transcriptase inhibitor (NNRTI), or PI and 2 nucleoside reverse transcriptase inhibitors (NRTIs) also recommended. Recommended alternatives to raltegravir (to be given in conjunction with 2 NRTIs) include ritonavir-boosted darunavir, etravirine, rilpivirine, ritonavir-boosted atazanavir, and lopinavir/ritonavir.
Management of occupational exposures to HIV is complex and evolving; consult infectious diseases specialist, clinician with expertise in administration of antiretroviral agents, and/or National Clinicians’ Postexposure Prophylaxis Hotline (PEPline at 888-448-4911) whenever possible. Do not delay initiation of PEP while waiting for expert consultation.
Postexposure Prophylaxis following Nonoccupational Exposure to HIV (nPEP)
Postexposure prophylaxis of HIV infection following nonoccupational exposure† [off-label] (nPEP) in individuals exposed to blood, genital secretions, or other potentially infectious body fluids that might contain HIV when the exposure represents a substantial risk for HIV transmission.
When nPEP indicated in adults and adolescents ≥13 years of age with normal renal function, CDC states preferred regimen is either raltegravir or dolutegravir used in conjunction with emtricitabine and tenofovir DF (given as emtricitabine/tenofovir DF; Truvada); alternative recommended in these patients is ritonavir-boosteddarunavir used in conjunction with emtricitabine/tenofovir DF (Truvada).
Consult infectious diseases specialist, clinician with expertise in administration of antiretroviral agents, and/or the National Clinicians’ Postexposure Prophylaxis Hotline (PEPline at 888-448-4911) if nPEP indicated in certain exposed individuals (e.g., pregnant women, children, those with medical conditions such as renal impairment) or if considering a regimen not included in CDC guidelines, source virus is known or likely to be resistant to antiretrovirals, or healthcare provider is inexperienced in prescribing antiretrovirals. Do not delay initiation of nPEP while waiting for expert consultation.
Ritonavir Dosage and Administration
General
Pretreatment Screening
-
Evaluate serum triglyceride and serum cholesterol concentrations prior to initiation of ritonavir therapy.
-
Ritonavir use has been associated with changes in serum AST, ALT, γ-glutamyltransferase (GGT), creatine phosphokinase (CPK), and uric acid. Perform appropriate laboratory tests prior to initiation of therapy.
Patient Monitoring
-
Consider monitoring for hyperglycemia, new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus in patients receiving ritonavir.
-
Monitor serum triglyceride and serum cholesterol concentrations at periodic intervals during ritonavir therapy.
-
Monitor appropriate laboratory tests (e.g., AST, ALT, GGT, CPK, uric acid) periodically after initiation of therapy, and when clinical signs and symptoms occur.
-
Clinical monitoring recommended when ritonavir is used concomitantly with drugs that prolong the PR interval (including calcium channel blockers, β-adrenergic blockers, digoxin, atazanavir), particularly with drugs metabolized by cytochrome P-450 (CYP) isoenzyme 3A.
Dispensing and Administration Precautions
-
The Institute for Safe Medication Practices (ISMP) list of error-prone abbreviations, symbols, and dose designations states that the use of abbreviations for antiretroviral medications (e.g., DOR, TAF, TDF) during the medication use process should be avoided as their use has been associated with serious medication errors.
Other General Considerations
-
Use with caution in patients with preexisting liver disease, liver enzyme abnormalities, or coinfection with hepatitis B virus (HBV) or hepatitis C virus (HCV). Consider more frequent testing of serum AST and ALT concentrations in these patients, especially during the first 3 months of therapy.
-
Use ritonavir with caution in patients with structural heart disease, cardiac conduction abnormalities, ischemic heart disease, and cardiomyopathies.
Administration
Ritonavir can be given orally as film-coated tablets or oral powder.
Must be given in combination with other antiretrovirals for treatment of HIV.
Oral Administration
Tablets
Administer orally with a meal. Swallow tablets whole; do not break, chew, or crush.
Oral Powder
Only indicated for use in pediatric patients.
Administer orally with a meal; may lessen bitter aftertaste of oral powder.
Only use for dosing increments of 100 mg; do not use for doses <100 mg or for dose increments between 100 mg intervals.
Mix oral powder with a soft food (e.g., applesauce, vanilla pudding) or liquid (e.g., water, chocolate milk, infant formula). After mixing, must be used within 2 hours; discard after this period.
May administer via feeding tube if mixed with water.
Dosage
Must be given in conjunction with other antiretrovirals. Low-dose ritonavir is used with certain PIs (atazanavir, darunavir, fosamprenavir) in ritonavir-boosted regimens.
If using full-dose ritonavir, initiate therapy using a dose escalation schedule to minimize nausea.
Pediatric Patients
Treatment of HIV Infection
Low-dose Ritonavir for Ritonavir-boosted PI Regimens
OralWhen low-dose ritonavir is used with another HIV PI as a pharmacokinetic enhancer (ritonavir-boosted PI), dosage of ritonavir varies and is specific to the drug combination in use.
Full-dose Ritonavir
Oral>1 month of age: Manufacturer recommends 250 mg/m2 twice daily initially; at 2- or 3-day intervals, increase in increments of 50 mg/m2 twice daily as tolerated up to 350–400 mg/m2 twice daily (not >600 mg twice daily).
If dosage of 400 mg/m2 twice daily not tolerated (due to adverse effects), highest dosage that is tolerated may be used for maintenance therapy in conjunction with other antiretrovirals; however, consider use of an alternative antiretroviral therapy.
Adults
Treatment of HIV Infection
Low-dose Ritonavir for Ritonavir-boosted PI Regimens
Oral100–400 mg daily.
Full-dose Ritonavir
OralInitially 300 mg twice daily; at 2- to 3-day intervals, increase dosage by 100 mg twice daily up to a dosage of 600 mg twice daily.
Special Populations
Hepatic Impairment
Dosage adjustments not necessary in patients with mild to moderate hepatic impairment (Child-Pugh class A or B); data not available for severe hepatic impairment (Child-Pugh class C).
Renal Impairment
Manufacturer states that clinically important decreases in ritonavir clearance not expected in renal impairment.
Geriatric Patients
Select dosage carefully; initiate therapy at the low end of the dosing range.
Cautions for Ritonavir
Contraindications
-
Known hypersensitivity (e.g., toxic epidermal necrolysis, Stevens-Johnson syndrome) to ritonavir or any ingredient in the formulation.
-
Concomitant use with drugs highly dependent on CYP3A for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening events (e.g., alfuzosin, amiodarone, cisapride, colchicine [in patients with hepatic or renal impairment], dronedarone, ergot alkaloids, flecainide, lomitapide, lovastatin, lurasidone, oral midazolam, pimozide, propafenone, quinidine, ranolazine, sildenafil used for treatment of pulmonary arterial hypertension [PAH], simvastatin, triazolam, voriconazole).
-
Concomitant use with drugs that are potent CYP3A inducers where significantly reduced ritonavir plasma concentrations may be associated with a potential loss of virologic response and possible development of resistance and cross-resistance (e.g., apalutamide, St. John's wort [Hypericum perforatum]).
Warnings/Precautions
Warnings
Risk of Serious Adverse Reactions Due to Drug Interactions
Concomitant use with certain drugs contraindicated because of risk of life-threatening adverse events, significant interaction, or loss of virologic activity (see Boxed Warning). Concomitant use with other drugs may require caution, dosage adjustments, and/or increased monitoring. When ritonavir-boosted PI regimens are used, the usual cautions, precautions, and contraindications associated with the other PI should be considered.
Other Warnings and Precautions
Hepatic Effects
Elevated hepatic aminotransferase concentrations >5 times ULN, clinical hepatitis, and jaundice reported; risk may be increased in patients with HBV or HCV coinfection.
Use with caution in patients with preexisting liver disease, liver enzyme abnormalities, or hepatitis; consider more frequent testing of serum AST and ALT concentrations in these patients, especially during the first 3 months of therapy.
Hepatic dysfunction (including some fatalities) reported. Generally has occurred in patients with advanced HIV infection and/or receiving multiple concomitant drugs.
Pancreatitis
Pancreatitis (sometimes fatal) with or without marked elevations in triglycerides has occurred.
Patients with advanced HIV disease may be at increased risk of elevated triglycerides and pancreatitis.
Consider pancreatitis in patients who develop abdominal pain, nausea, and vomiting or elevated serum amylase or lipase concentrations. Discontinue ritonavir if a diagnosis of pancreatitis is made.
Allergic Reactions/Hypersensitivity
Urticaria, mild skin eruptions, bronchospasm, and angioedema have occurred. Anaphylaxis, toxic epidermal necrolysis, and Stevens-Johnson syndrome reported rarely. Discontinue ritonavir if severe reactions occur.
PR Interval Prolongation
Prolongation of PR interval reported. Second- or third-degree AV block reported during postmarketing monitoring.
Use with caution in patients with structural heart disease, cardiac conduction abnormalities, ischemic heart disease, or cardiomyopathies; these individuals may be at increased risk for cardiac conduction abnormalities.
Caution advised if used with other drugs that prolong PR interval (e.g., some β-adrenergic blocking agents, some calcium-channel blockers, digoxin, atazanavir), especially drugs metabolized by CYP3A.
Lipid Disorders
Substantial increases in total serum cholesterol and triglyceride concentrations have occurred. Determine serum triglyceride and cholesterol concentrations prior to and periodically during therapy; manage lipid disorders as clinically appropriate.
Diabetes Mellitus/Hyperglycemia
Hyperglycemia, new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus reported with use of PIs; diabetic ketoacidosis has occurred. Monitor blood glucose and initiate or adjust dosage of oral hypoglycemic agent or insulin as needed.
Immune Reconstitution Syndrome
During initial treatment, patients who respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium complex [MAC], M. tuberculosis, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii]); this may necessitate further evaluation and treatment.
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome) have been reported to occur in the setting of immune reconstitution; the time to onset is more variable and can occur many months after initiation of antiretroviral therapy.
Fat Redistribution
Possible redistribution or accumulation of body fat, including central obesity, dorsocervical fat enlargement ("buffalo hump"), peripheral wasting, facial wasting, breast enlargement, and general cushingoid appearance; causal relationship not established.
Patients with Hemophilia
Spontaneous bleeding noted with PIs; causal relationship not established.
Caution in patients with hemophilia type A or B. Increased hemostatic (e.g., antihemophilic factor) therapy may be needed.
Resistance/Cross-resistance
Possibility of HIV resistant to ritonavir and possible cross-resistance to other PIs. Continued full-dose ritonavir therapy after loss of viral suppression may increase likelihood of cross-resistance to other PIs.
Laboratory Tests
Associated with alterations in certain laboratory tests (e.g., serum AST, ALT, γ-glutamyltransferase (GGT), CPK, uric acid). Perform appropriate clinical chemistry tests prior to and periodically after initiation of ritonavir, or when symptoms occur.
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry at 800-258-4263 or [Web].
Data from the registry indicate that birth defects occurred in 2.3% of live births following first trimester exposures and in 2.9% of live births following second/third trimester exposures; the birth defect rate among pregnant women in the US reference population is 2.7%.
Lactation
Limited data indicate that ritonavir is distributed into human milk.
The HHS perinatal HIV transmission guideline provides updated recommendations on infant feeding. The guideline states that patients with HIV should receive evidence-based, patient-centered counseling to support shared decision making about infant feeding. During counseling, patients should be informed that feeding with appropriate formula or pasteurized donor human milk from a milk bank eliminates the risk of postnatal HIV transmission to the infant. Additionally, achieving and maintaining viral suppression with antiretroviral therapy during pregnancy and postpartum reduces the risk of breastfeeding HIV transmission to <1%, but does not completely eliminate the risk. Replacement feeding with formula or banked pasteurized donor milk is recommended when patients with HIV are not on antiretroviral therapy and/or do not have a suppressed viral load during pregnancy (at a minimum throughout the third trimester), as well as at delivery.
Females and Males of Reproductive Potential
No evidence of effects on fertility when given to male or female rats at exposures equivalent to 40 and 60% of the human dosage, respectively. Because ritonavir may reduce the efficacy of combined hormonal contraceptives, advise patients to use an effective alternative contraceptive method or an additional barrier method of contraception.
Pediatric Use
Safety and efficacy established in infants >1 month of age.
Antiretroviral activity in children >1 month to 21 years of age similar to that in adults. Adverse effects in children >1 month to 21 years of age similar to those reported in adults; vomiting, diarrhea, skin rash/allergy reported in ≥2% of pediatric patients in clinical studies.
Geriatric Use
Insufficient experience in those ≥65 years of age to determine whether they respond differently than younger adults.
Select dosage with caution, usually starting at the lower end of the dosing range, because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Hepatic Impairment
Use with caution in patients with preexisting liver disease, liver enzyme abnormalities, or hepatitis; consider more frequent monitoring of AST and ALT, especially during the first 3 months.
There may be an increased risk for transaminase elevations in patients with underlying hepatitis B or C.
No dosage adjustment required for patients with mild (Child-Pugh Class A) or moderate hepatic impairment (Child-Pugh Class B). Not studied in those with severe hepatic impairment (Child-Pugh Class C); avoid use
Renal Impairment
Pharmacokinetics not evaluated in patients with renal impairment. Because ritonavir undergoes negligible renal excretion, reduced clearance in renal impairment not expected.
Common Adverse Effects
The most frequent adverse reactions occurring in ≥25% of patients receiving ritonavir alone or combined with other antiretrovirals include GI reactions (diarrhea, nausea, vomiting, upper and lower abdominal pain), neurologic disturbances (including paresthesia and oral paresthesia), rash, and fatigue/asthenia.
Drug Interactions
Metabolized by CYP3A and, to a lesser extent, by CYP2D6.
Strong inhibitor of CYP3A.
Induces CYP3A, CYP1A2, CYP2C9, CYP2C19, and CYP2B6; increases activity of glucuronosyl transferase.
When used concomitantly with other PIs (i.e., atazanavir, darunavir, fosamprenavir), consult the prescribing information for that PI, including important drug interaction information.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions likely with drugs that are inhibitors, inducers, or substrates of CYP3A4 or CYP2D6 with possible alteration in metabolism of ritonavir and/or other drug.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Alfuzosin |
Possible pharmacokinetic interaction; may result in hypotension |
Concomitant use contraindicated |
|
Antiarrhythmic agents (amiodarone, disopyramide, dronedarone, flecainide, systemic lidocaine, mexiletine, propafenone, quinidine) |
Possible increased antiarrhythmic agent concentrations; potential for serious or life-threatening effects (e.g., cardiac arrhythmias) |
Amiodarone, dronedarone, flecainide, propafenone, quinidine: Concomitant use contraindicated Disopyramide, mexiletine, systemic lidocaine: Use caution; monitor concentrations of the antiarrhythmic agent |
|
Anticancer agents (abemaciclib, apalutamide, dasatinib, encorafenib, fostamatinib, ibrutinib, ivosidenib, neratinib, nilotinib, venetoclax, vinblastine, vincristine) |
Abemaciclib, dasatinib, encorafenib, ibrutinib, ivosidenib, neratinib, nilotinib, venetoclax: Possible increased concentrations of the anticancer agent Apalutamide: Increased apalutamide concentrations; possible decreased ritonavir concentrations. Potential loss of virologic response and development of resistance to ritonavir and other PIs Fostamatinib: Increased concentrations of R406 (fostamatinib metabolite) and increases in dose-related adverse events (e.g., hepatoxicity, neutropenia) Vinblastine, vincristine: Possible increased concentrations of the vinca alkaloid |
Apalutamide: Concomitant use contraindicated due to potential loss of virologic response and development of resistance to other PIs Encorafenib, ivosidenib: Avoid concomitant use due to potential serious adverse events (e.g., QT prolongation); if concomitant use cannot be avoided, adjust ritonavir dosage as described in encorafenib prescribing information. If concomitant use with ivosidenib cannot be avoided, reduce ivosidenib dosage to 250 mg once daily. Dasatinib: May need to decrease dasatinib dosage or adjust dosing interval. Consult dasatinib prescribing information for dosage recommendations on concomitant use with strong CYP3A inhibitors Neratinib, ibrutinib, venetoclax: Avoid concomitant use Nilotinib: Dosage of nilotinib may need to be decreased or dosing interval adjusted. Consult nilotinib prescribing information for dosage recommendations on concomitant use with strong CYP3A inhibitors Fostamatinib: Monitor for toxicities from increased exposure (e.g., hepatotoxicity, neutropenia); reduced dosage of fostamatinib may be necessary Vinblastine, vincristine: Manufacturer of ritonavir recommends considering temporarily withholding ritonavir-containing antiretroviral regimens in patients who develop substantial hematologic or GI toxicity; alternatively, consider use of an antiretroviral regimen that does not include a CYP3A or P-gp inhibitor |
|
Anticoagulants, oral |
Rivaroxaban: Increased rivaroxaban concentrations and AUC; may increase bleeding risk Warfarin: Possible altered warfarin concentrations |
Rivaroxaban: Avoid concomitant use Warfarin: Monitor INR frequently during concomitant use |
|
Anticonvulsants |
Carbamazepine, clonazepam, ethosuximide: Possible increased anticonvulsant concentrations Divalproex, lamotrigine, phenytoin: Possible decreased anticonvulsant concentrations |
Carbamazepine, clonazepam, ethosuximide: Reduced anticonvulsant dosage may be necessary; monitor anticonvulsant concentrations Divalproex, lamotrigine, phenytoin: Increased anticonvulsant dosage may be needed; monitor anticonvulsant concentrations |
|
Antifungals, azoles |
Fluconazole: Ritonavir peak plasma concentrations and AUC increased by 15% or less Itraconazole: Potentially increased itraconazole and ritonavir concentrations Ketoconazole: Increased ritonavir and ketoconazole concentrations Voriconazole: Decreased voriconazole AUC (by 82% with ritonavir 400 mg twice daily |
Itraconazole: Avoid itraconazole dosages >200 mg daily Ketoconazole: Avoid ketoconazole dosages >200 mg daily Voriconazole: Concomitant use with ritonavir 400 mg twice daily contraindicated; potential loss of antifungal efficacy Voriconazole: Concomitant use with low-dose ritonavir (100 mg) not recommended unless benefit outweighs risk |
|
Antimycobacterials (bedaquiline, rifabutin, rifampin) |
Bedaquiline: Possible increased bedaquiline concentrations Rifabutin: Increased concentrations of rifabutin and its metabolite Rifampin: Decreased ritonavir concentrations may lead to loss of virologic response |
Bedaquiline: Use concomitantly with caution only if potential benefits outweigh risks Rifabutin: Reduce rifabutin dosage to 150 mg every other day or 150 mg 3 times weekly; further dosage reduction may be needed Rifampin: Concomitant use not recommended; use another antimycobacterial agent such as rifabutin |
|
Atazanavir |
Increased atazanavir concentrations Prolonged PR interval reported with both atazanavir and ritonavir |
Ritonavir dosage reduction necessary; consult the full prescribing information for atazanavir for recommendations on concomitant use of ritonavir Use concomitantly with caution and clinical monitoring |
|
Atovaquone |
Possible decreased atovaquone concentrations |
Clinical importance unknown; increased atovaquone dosage may be needed |
|
Avanafil |
Increased avanafil concentrations and AUC |
Do not use concomitantly; safe and effective avanafil dosage for concomitant use with ritonavir not established |
|
Benzodiazepines |
Oral midazolam or triazolam: Possible increased benzodiazepine concentrations; potential for prolonged or increased sedation or respiratory depression Clorazepate, diazepam, estazolam, flurazepam: Possible increased concentrations of the benzodiazepine Alprazolam: Decreased alprazolam clearance |
Oral midazolam or triazolam: Concomitant use contraindicated Parenteral midazolam: Must be administered in a closely monitored setting where respiratory depression and/or prolonged sedation can be managed; the manufacturer of ritonavir states that a reduced midazolam dosage should be considered, particularly if multiple doses administered Clorazepate, diazepam, estazolam, flurazepam: Reduced benzodiazepine dosage may be needed |
|
β-Adrenergic blocking agents (metoprolol, timolol) |
Possible increase in concentrations of the β-adrenergic blocking agent Adverse cardiac and neurologic effects reported with β-adrenergic blocking agents Impact on the PR interval with concomitant use of ritonavir not evaluated |
Monitor patient; caution advised; reduced dosage of the β-adrenergic blocking agent may be necessary |
|
Bosentan |
Possible increased bosentan concentrations |
In patients already receiving ritonavir for ≥10 days, initiate bosentan using dosage of 62.5 mg once daily or every other day based on individual tolerability In patients already receiving bosentan, discontinue bosentan for at least 36 hours prior to initiating ritonavir; after ≥10 days of ritonavir, resume bosentan using dosage of 62.5 mg once daily or every other day based on individual tolerability |
|
Calcium-channel blocking agents (diltiazem, nifedipine, verapamil) |
Possible increased concentrations of the calcium-channel blocking agent |
Monitor patient; caution advised; reduced dosage of the calcium-channel blocking agent may be necessary |
|
Cisapride |
Possible increased concentrations of cisapride; potential for serious or life-threatening reactions (e.g., cardiac arrhythmias) |
Concomitant use contraindicated |
|
Colchicine |
Possible increased colchicine concentrations |
Patients with renal or hepatic impairment: Concomitant use contraindicated Colchicine for treatment of gout flares in patients with normal renal and hepatic function: In those receiving ritonavir, use initial colchicine dose of 0.6 mg followed by 0.3 mg 1 hour later and repeat dose no earlier than 3 days later Colchicine for prophylaxis of gout flares in patients with normal renal and hepatic function: In those receiving ritonavir, decrease colchicine dosage to 0.3 mg once daily in those originally receiving 0.6 mg twice daily or decrease dosage to 0.3 mg once every other day in those originally receiving 0.6 mg once daily Colchicine for treatment of familial Mediterranean fever (FMF) in patients with normal renal and hepatic function: In those receiving ritonavir, use maximum colchicine dosage of 0.6 mg daily (may be given as 0.3 mg twice daily) |
|
Corticosteroids (betamethasone, beclomethasone, budesonide, ciclesonide, dexamethasone, fluticasone, methylprednisolone, prednisolone, prednisone, triamcinolone) |
Betamethasone, budesonide, ciclesonide, dexamethasone, fluticasone, methylprednisolone, mometasone, prednisone, triamcinolone (orally inhaled, intranasal, systemic, ophthalmic): Increased corticosteroid concentrations; Cushing’s syndrome and adrenal suppression reported when ritonavir used concomitantly with corticosteroids with significantly increased exposures due to strong CYP3A inhibitors |
Betamethasone, budesonide, ciclesonide, dexamethasone, fluticasone, methylprednisolone, mometasone, prednisone, triamcinolone (orally inhaled, intranasal, systemic, ophthalmic): Consider alternative corticosteroids that are less affected by concomitant strong CYP3A4 inhibitors (e.g., beclomethasone, prednisolone), particularly for long-term use |
|
Co-trimoxazole |
Decreased sulfamethoxazole exposure and increased trimethoprim exposure |
|
|
Darunavir |
Increased darunavir concentrations |
Ritonavir dosage reduction necessary; consult the full prescribing information for darunavir for recommendations on concomitant use of ritonavir |
|
Delavirdine |
Increased ritonavir concentrations |
Appropriate dosage for concomitant use with respect to safety and efficacy not established |
|
Didanosine |
Decreased didanosine concentrations and AUC; no effect on ritonavir concentrations In vitro evidence of additive antiretroviral effects |
|
|
Digoxin |
Increased digoxin concentrations Impact on PR interval with concomitant use of ritonavir not evaluated |
Caution advised; monitor serum digoxin concentrations |
|
Dronabinol |
Possible increased dronabinol concentrations |
Use concomitantly with caution; decreased dronabinol dosage may be needed |
|
Elagolix |
Possible increased elagolix concentrations and decreased ritonavir concentrations |
Limit the duration of concomitant elagolix 200 mg twice daily with ritonavir to ≤1 month to avoid risk of potential bone loss and transaminase elevations Limit the duration of concomitant elagolix 150 mg once daily with ritonavir to 6 months |
|
Ergot alkaloids (dihydroergotamine, ergotamine, methylergonovine) |
Possibility of pharmacokinetic interaction; potential for serious or life-threatening reactions (e.g., acute ergot toxicity) |
Concomitant use contraindicated |
|
Estrogens/Progestins |
Hormonal contraceptives: Decreased peak plasma concentrations of ethinyl estradiol with oral or transdermal contraceptive preparations |
Use alternative or additional contraceptive measures |
|
Fentanyl |
Possible increased fentanyl concentrations |
Carefully monitor for fentanyl therapeutic effects and adverse effects, including potentially fatal respiratory depression |
|
Fosamprenavir |
Increased amprenavir concentrations |
Ritonavir dosage reduction necessary; consult the full prescribing information for fosamprenavir for recommendations on concomitant use of ritonavir |
|
Glecaprevir/pibrentasvir |
Possible increased glecaprevir/pibrentasvir concentrations |
Concomitant use not recommended |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin, lovastatin, rosuvastatin, simvastatin: Decreased clearance and increased concentrations of the statin with potential for increased risk of statin-associated adverse effects, including myopathy and rhabdomyolysis |
Atorvastatin: Carefully titrate and use lowest necessary atorvastatin dosage with careful monitoring. If used concomitantly with aritonavir-boosted PI regimen, consult the PI prescribing information for recommendations Lovastatin: Concomitant use contraindicated Rosuvastatin: Carefully titrate and use lowest necessary rosuvastatin dosage with careful monitoring. If used concomitantly with a ritonavir-boosted PI regimen, consult the PI prescribing information for recommendations Simvastatin: Concomitant use contraindicated |
|
Immunosuppressive agents (cyclosporine, sirolimus, tacrolimus) |
Potential for increased concentrations of cyclosporine, sirolimus, or tacrolimus |
Monitor concentrations of the immunosuppressive agent |
|
Lomitapide |
Increased concentrations of lomitapide |
Concomitant use of moderate or strong CYP3A4 inhibitors, such as ritonavir, contraindicated |
|
Macrolides (clarithromycin) |
Clarithromycin: Increased AUC of ritonavir and clarithromycin; decreased AUC of 14-hydroxyclarithromycin |
Clarithromycin: Dosage adjustment not needed in patients with normal renal function; reduce clarithromycin dosage by 50% in patients with Clcr of 30–60 mL/minute and by 75% in patients with Clcr <30 mL/minute |
|
Maraviroc |
Increased maraviroc concentrations |
Consult maraviroc prescribing information for concomitant use with ritonavir and ritonavir-boosted PIs |
|
Meperidine |
Decreased meperidine concentration; increased normeperidine (meperidine metabolite) concentration |
Dosage increase and long-term concomitant use not recommended because normeperidine has analgesic and CNS stimulant activity (e.g., seizures) |
|
Methadone |
Decreased methadone concentrations and AUC |
Consider need to increase methadone dosage |
|
Methamphetamine |
Possible increased methamphetamine concentrations |
Use concomitantly with caution; decreased methamphetamine dosage may be needed |
|
Psychotherapeutic agents |
Lurasidone: Increased lurasidone concentrations expected; potential for serious or life-threatening reactions Pimozide: Increased pimozide concentrations expected; potential for serious or life-threatening reactions (e.g., cardiac arrhythmias) Quetiapine: Increased quetiapine concentrations expected Trazodone: Increased trazodone concentrations and AUC; adverse effects (nausea, dizziness, hypotension, syncope) reported with concomitant trazodone and ritonavir Bupropion: Possible decreased bupropion and hydroxybupropion (active metabolite) concentrations Other psychotherapeutics: Possible increased plasma concentrations of buspirone, nefazodone, perphenazine, risperidone, thioridazine Adverse cardiac and neurologic effects reported with nefazodone or trazodone |
Lurasidone: Concomitant use contraindicated Pimozide: Concomitant use contraindicated Quetiapine: Consider use of an alternative antiretroviral to avoid drug interaction. Refer to full quetiapine prescribing information for the initiation and titration of quetiapine; if initiating ritonavir in patients receiving quetiapine, reduce quetiapine to one-sixth of original dosage; monitor for efficacy and adverse effects of quetiapine Trazodone: Consider decreased trazodone dosage Bupropion: Monitor for response to bupropion Amitriptyline, nortriptyline: Consider decreased dosage when used concomitantly with ritonavir Other psychotherapeutics: Dosage reduction of the psychotherapeutic agent (buspirone, nefazodone, perphenazine, risperidone, thioridazine) may be necessary |
|
Quinine |
Possible increased quinine concentrations |
Decreased quinine dosage may be necessary |
|
Raltegravir |
Low-dose ritonavir (100 mg twice daily): Decreased raltegravir concentrations and AUC; data not available regarding concomitant use of raltegravir and higher ritonavir dosage, but raltegravir concentrations may be decreased |
|
|
Ranolazine |
Increased ranolazine concentrations; possibly serious or life-threatening adverse reactions |
Concomitant use contraindicated |
|
St. John’s wort (Hypericum perforatum) |
Decreased ritonavir concentrations; possible loss of virologic response and increased risk of ritonavir resistance |
Concomitant use contraindicated |
|
Salmeterol |
Increased salmeterol concentrations; may increase risk of QT interval prolongation, palpitations, or sinus tachycardia |
Concomitant use not recommended |
|
Selective serotonin-reuptake inhibitors (SSRIs) |
Concomitant use with some SSRIs (e.g., fluoxetine, paroxetine) may increase plasma concentrations of the SSRI Fluoxetine: Adverse cardiac and neurologic effects reported |
SSRI dosage may need to be reduced |
|
Tadalafil |
Increased tadalafil concentrations and increased risk of tadalafil-associated adverse effects (e.g., hypotension, visual disturbances, prolonged erection, syncope) |
Tadalafil (Adcirca) for treatment of PAH: In patients already receiving ritonavir for ≥1 week, use initial tadalafil dosage of 20 mg once daily and increase to 40 mg once daily based on individual tolerability Avoid use of tadalafil (Adcirca) for treatment of PAH during initiation of PI therapy; in a patient already receiving tadalafil (Adcirca) for treatment of PAH, discontinue tadalafil for at least 24 hours before starting ritonavir; tadalafil can be restarted after ≥1 week of ritonavir therapy using initial tadalafil dosage of 20 mg once daily and increasing dosage to 40 mg once daily based on individual tolerability Tadalafil for treatment of erectile dysfunction: Use caution and do not exceed a single dose of 10 mg in 72 hours; monitor for adverse effects |
|
Theophylline |
Decreased theophylline concentrations |
Increased theophylline dosage may be necessary; monitor theophylline concentrations |
|
Tramadol |
Decreased tramadol dosage may be needed |
|
|
Tricyclic antidepressants (amitriptyline, desipramine, nortriptyline) |
Concomitant use with some tricyclic antidepressants (e.g., amitriptyline, nortriptyline) expected to increase plasma concentrations of the antidepressant Desipramine: Increased desipramine concentrations |
Decreased tricyclic antidepressant dosage may be needed Desipramine: Decrease desipramine dosage and monitor desipramine concentrations |
|
Vardenafil |
Increased vardenafil concentrations and increased risk of vardenafil-associated adverse effects (e.g., hypotension, visual disturbances, prolonged erection) |
Use caution and initial vardenafil dose of 2.5 mg; do not exceed dosage of 2.5 mg once every 72 hours |
|
Zidovudine |
No effect on ritonavir pharmacokinetics; decreased zidovudine peak concentrations and AUC In vitro evidence of additive antiretroviral effects |
|
|
Zolpidem |
Possible increased zolpidem concentrations |
Use concomitantly with caution; decreased zolpidem dosage may be necessary |
Ritonavir Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations attained within 2 and 4 hours under fasting and non-fasting conditions, respectively.
Ritonavir tablets are not bioequivalent to ritonavir capsules (no longer marketed in US); similar AUC but higher peak plasma concentration with ritonavir tablets compared with capsules.
Administration with food delays time to peak plasma concentrations by 2 hours.
Compared with administration in the fasting state, extent of absorption was 21–23% lower when ritonavir tablets were administered with a moderate-fat or high-fat meal.
Compared with administration in the fasting state, extent of absorption was 23–49% lower when ritonavir oral powder was administered with a moderate-fat or high-fat meal.
Special Populations
Hepatic impairment: Decreased ritonavir concentrations in patients with moderate hepatic impairment compared with individuals with normal hepatic function.
Pediatric patients >2 years of age: Limited data indicate ritonavir dosages of 350–400 mg/m2 twice daily in those >2 years of age result in plasma concentrations comparable to those reported in adults receiving 600 mg of ritonavir twice daily.
Infants 1–24 months of age: Ritonavir trough concentrations in infants receiving 350–450 mg/m2 of ritonavir twice daily were lower than concentrations reported in adults receiving 600 mg of ritonavir twice daily. Higher ritonavir exposures not observed with 450 mg/m2 twice daily compared with 350 mg/m2 twice daily in these infants.
Distribution
Extent
Not fully characterized.
Low concentrations cross the placenta; has been detected in cord blood and neonatal hair.
Limited data indicate present in human milk.
Plasma Protein Binding
98–99%.
Special Populations
Mild to moderate hepatic impairment does not result in clinically important changes in protein binding.
Elimination
Metabolism
Metabolized by CYP3A and, to a lesser extent, by CYP2D6.
Elimination Route
Excreted principally in feces (86.4%) as unchanged drug (33.8%) and metabolites; 11.3% excreted in urine (3.5% as unchanged drug).
Dialysis unlikely to remove substantial amounts of ritonavir.
Half-life
3–5 hours.
Stability
Storage
Oral
Tablets
≤30°C; exposure to temperatures up to 50°C for 7 days permitted. Dispense in original container or USP equivalent tight container (≤60 mL); avoid prolonged exposure (>2 weeks) to high humidity outside such containers.
Oral Powder
≤30°C.
Actions and Spectrum
-
Active against HIV-1.
-
Inhibits replication of HIV by interfering with HIV protease.
-
HIV-1 with reduced susceptibility to ritonavir has been selected in vitro and emerged during therapy with the drug.
-
Varying degrees of cross-resistance occur among HIV PIs.
Advice to Patients
-
Advise patients and/or caregivers to read and follow directions for preparation of ritonavir oral powder.
-
Advise caregivers to update their healthcare provider when their child's weight changes so that their ritonavir dose may be adjusted as necessary.
-
Critical nature of compliance with HIV therapy and importance of remaining under the care of a clinician. Stress importance of taking as prescribed; do not alter or discontinue antiretroviral regimen without consulting clinician.
-
Stress importance of using in conjunction with other antiretrovirals—not for monotherapy.
-
Stress importance of taking ritonavir with a meal.
-
If a dose is missed, it should be taken as soon as it is remembered and the next dose taken at the regularly scheduled time; if a dose is skipped, the next dose should not be doubled.
-
Advise patients that ECG changes (PR prolongation) have occurred; stress importance of consulting clinician if dizziness, lightheadedness, abnormal heart beats, or loss of consciousness occurs.
-
Inform patients that pre-existing liver disease, including HBV or HCV infections, can worsen during use of ritonavir, therefore, liver function test monitoring is necessary during therapy. Advise patients to inform their healthcare providers if signs and symptoms of worsening liver dysfunction develop (e.g., loss of appetite, stomach pain, jaundice, skin itchiness).
-
Advise patients to notify their healthcare provider if signs and symptoms suggestive of pancreatitis develop (e.g., nausea, vomiting, stomach pain).
-
Advise patients to inform their healthcare provider if a rash develops during treatment.
-
Inform patients that redistribution/accumulation of body fat may occur, with as yet unknown long-term health effects.
-
Inform patients that hyperglycemia, new-onset diabetes mellitus, or exacerbation of preexisting diabetes mellitus can occur. Patients should promptly notify their healthcare provider if signs and symptoms of diabetes develop (e.g., urinating frequently, excessive thirst or hunger, or excessive weight loss and/or increased blood glucose).
-
Inform patients that cholesterol and triglyceride levels may increase with use of ritonavir.
-
Inform patients with hemophilia that increased bleeding may occur when protease inhibitors such as ritonavir are used.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements (e.g., St. John’s wort), and any concomitant illnesses.
-
Stress importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Inform patients that an antiretroviral pregnancy registry is available that monitors fetal outcomes of infants exposed to ritonavir. Providers can register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263. Inform patients using combined hormonal contraception to use an effective alternative contraceptive method or an additional barrier method during therapy with ritonavir because hormone levels may be decreased.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Powder |
100 mg |
Norvir |
AbbVie |
|
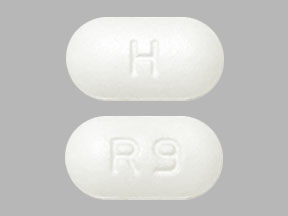
Tablets, film-coated |
100 mg* |
Ritonavir Tablets |
||
|
Norvir |
AbbVie |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Biktarvy
Biktarvy is a complete HIV-1 treatment in a once-a-day single tablet containing three antiviral ...
Descovy
Descovy is used to treat and prevent HIV infection in adults and adolescents. When used for HIV-1 ...
Cabenuva
Cabenuva (cabotegravir and rilpivirine) injections are a long-acting HIV treatment used to keep HIV ...
Truvada
Truvada is used to prevent HIV (HIV PrEP) or treat HIV-1 infection in combination with other HIV-1 ...
Atripla
Atripla prevents the human immunodeficiency virus (HIV) from reproducing in your body. Learn about ...
Complera
Complera (emtricitabine, rilpivirine, and tenofovir) is used to treat HIV infection. Includes ...
Stribild
Stribild (cobicistat, elvitegravir, emtricitabine and tenofovir) is used to treat HIV-1 infection ...
Epzicom
Epzicom is used to treat HIV, which causes the acquired immunodeficiency syndrome (AIDS). Learn ...
Emtricitabine
Emtricitabine is used for HIV Infection, nonoccupational exposure, occupational exposure
Frequently asked questions
More about ritonavir
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (3)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antiviral boosters
- Breastfeeding
- En español