Glycopyrrolate (Monograph)
Brand names: Bevespi Aerosphere (combination), Cuvposa, Lonhala Magnair, Robinul, Seebri Neohaler, Utibron Neohaler (combination)
Drug class: Antimuscarinics/Antispasmodics
VA class: AU350
CAS number: 596-51-0
Introduction
Antimuscarinic; a synthetic quaternary ammonium compound.
Uses for Glycopyrrolate
COPD
Glycopyrrolate oral inhalation powder or solution: Maintenance treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema.
Glycopyrrolate/formoterol fixed combination oral inhalation aerosol: Maintenance treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema.
Glycopyrrolate/indacaterol fixed combination oral inhalation powder: Maintenance treatment of airflow obstruction in patients with COPD, including chronic bronchitis and/or emphysema.
Not indicated for treatment of acute bronchospasm.
Not indicated for treatment of asthma; safety and efficacy not established.
Drooling
Glycopyrrolate oral solution: Symptomatic management of chronic severe drooling in pediatric patients with neurologic conditions (e.g., cerebral palsy) associated with problematic drooling.
Peptic Ulcer Disease
Used orally or parenterally as an adjunct in the treatment of peptic ulcer disease; however, no conclusive data that it aids in healing, decreases rate of recurrence, or prevents complications of peptic ulcers.
Parenteral route preferred as adjunct in the treatment of peptic ulcer disease when rapid anticholinergic effect desired or oral administration not tolerated.
With the advent of more effective therapies for the treatment of peptic ulcer disease, antimuscarinics have only limited usefulness in this condition.
Surgery
Used parenterally to inhibit salivation and excessive secretions of the respiratory tract (antisialogue). However, current surgical practice (e.g., using general anesthetics that do not stimulate salivary and tracheobronchial secretions) has reduced the need to control excessive respiratory secretions during surgery.
Used parenterally to prevent other cholinergic effects during surgery (e.g., cardiac arrhythmias, hypotension, bradycardia) secondary to visceral traction (resultant vagal stimulation), carotid sinus stimulation, or concomitant drugs (e.g., succinylcholine).
Used parenterally to block adverse muscarinic effects of anticholinesterase agents that are used after surgery to terminate curarization.
Ineffective for preventing acid-aspiration pneumonitis† [off-label] during surgery.
Glycopyrrolate Dosage and Administration
Administration
Oral Administration
Tablets: Administer orally 2 or 3 times daily.
Oral solution: Administer 3 times daily at least 1 hour before or 2 hours after meals. Must use an accurate measuring device to measure and administer oral solution.
IM Administration
Injection: May be administered undiluted. May administer in the same syringe with other compatible preoperative medications. (See Compatibility in Syringe under Stability.)
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Injection: May be administered undiluted. Administer by direct IV injection; alternatively, administer via the tubing of a running IV infusion of a compatible solution.
Oral Inhalation
Oral Inhalation Powder
Administer glycopyrrolate oral inhalation powder using a special oral inhalation device (Neohaler) that delivers powdered drug from capsules. Administer the inhalation powder twice daily at the same time each day.
Administer glycopyrrolate/indacaterol fixed combination oral inhalation powder using a special oral inhalation device (Neohaler) that delivers powdered drug from capsules. Administer the fixed-combination inhalation powder twice daily at the same time each day.
Glycopyrrolate and glycopyrrolate/indacaterol capsules for oral inhalation should not be taken orally (i.e., swallowed).
To use Neohaler device, remove cap, then open inhaler by holding the base firmly and tilting the mouthpiece. Peel away protective backing from a blister card containing glycopyrrolate or glycopyrrolate/indacaterol to expose one capsule. Do not push capsule through foil to remove it from the blister. With dry hands, remove capsule from blister; place capsule into capsule chamber of the device; do not place capsule into mouthpiece of device. Close inhaler fully until it clicks. Hold inhaler upright with the mouthpiece pointing upward; press both piercing buttons together firmly at the same time once (click will be heard), then release the piercing buttons fully. Piercing the capsule may produce very small pieces, which may pass into the mouth; pieces not expected to cause harm if swallowed or inhaled.
Exhale completely; do not exhale into mouthpiece of inhaler device. Hold inhaler horizontally (piercing buttons facing left and right); place mouthpiece in mouth, closing lips firmly around it. Inhale rapidly, but steadily and as deeply as possible, without pressing the piercing buttons. During inhalation, a whirring noise created by the capsule spinning around in the chamber will be heard; a sweet flavor also may be detected. Continue holding the breath for at least 5–10 seconds or as long as comfortably possible while removing inhaler from mouth, then exhale. Open inhaler to see if any powder remains in the capsule. If powder remains, close inhaler and repeat steps for inhaling the drug. Most patients empty the capsule with 1 or 2 inhalations. Coughing may occur soon after inhaling the dose; coughing is not a concern. After inhalation, open mouthpiece and tip the device to dispose of the used capsule, then close inhaler and replace cap. Do not leave used capsules in the device.
If whirring noise is not heard, capsule may be stuck in the capsule chamber. If this occurs, open inhaler and carefully loosen capsule by tapping base of the inhaler; do not press the piercing buttons. Then repeat steps to inhale the drug.
Routine cleaning of inhaler not necessary; if desired, may clean mouthpiece inside and outside with a clean, dry, lint-free cloth, or may use a clean, dry, soft brush to wipe inhaler and remove any powder residue. Keep inhaler dry.
Each capsule of glycopyrrolate oral inhalation powder (Seebri Neohaler) contains 15.6 mcg of glycopyrrolate. Actual amount of drug delivered to the lungs depends on factors such as the patient’s inspiratory flow rate and inspiratory time. Under standardized in vitro testing at a fixed flow rate of 90 L/minute for 1.3 seconds, Neohaler device delivered 13.1 mcg of glycopyrrolate from the 15.6-mcg capsule (equivalent to 12.5 mcg of glycopyrronium).
Each capsule of glycopyrrolate/indacaterol oral inhalation powder (Utibron Neohaler) contains 15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol. Actual amount of drug delivered to the lungs depends on factors such as the patient’s inspiratory flow rate and inspiratory time. Under standardized in vitro testing at a fixed flow rate of 90 L/minute for 1.3 seconds, the Neohaler device delivered 12.8 mcg of glycopyrrolate (equivalent to 12.5 mcg of glycopyrronium) and 20.8 mcg of indacaterol from the capsule containing 15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol.
Oral Inhalation Solution
Administer glycopyrrolate oral inhalation solution via nebulization using a special oral inhalation device (Magnair nebulizer system). Administer the inhalation solution twice daily at the same time each day.
Glycopyrrolate solution for oral inhalation should not be taken orally (i.e., swallowed) and should not be injected.
Assemble Magnair nebulizer system according to manufacturer's instructions for use and ensure it is working properly.
Immediately prior to use, open the foil pouch; remove and separate the 2 single-dose vials; return one vial to the foil pouch and store in the nebulizer carrying bag. Insert vial to be used into bottom of medication cap until it clicks. Place medication cap with vial on top of handset body (with aerosol head already inserted) and turn in a clockwise direction until a click is heard; avoid touching the part of handset body that pierces the vial. Line up notch in medication cap with blue line on handset body.
To administer the dose, insert mouthpiece, press controller on/off button, and breathe normally through the mouthpiece. Avoid tilting handset, loosening or removing medication cap, or unclasping the handset body until treatment is complete. At the end of treatment (2–3 minutes), a beep will sound and controller will shut off automatically.
Follow manufacturer's instructions for cleaning handset after each treatment.
Each single-dose vial of glycopyrrolate oral inhalation solution (Lonhala Magnair) contains 25 mcg of glycopyrrolate in 1 mL of solution. Actual amount of drug delivered to the lungs depends on patient factors. Under standardized in vitro testing, the Magnair device delivered approximately 14.2 mcg of glycopyrrolate (equivalent to 11.4 mcg of glycopyrronium) from the mouthpiece.
Oral Inhalation Aerosol
Administer glycopyrrolate/formoterol fixed combination using a special oral inhalation device (Aerosphere) that delivers a metered-dose spray. Administer the oral inhalation aerosol as 2 inhalations twice daily (morning and evening).
Before first use, ensure that inhaler device (Bevespi Aerosphere) is at room temperature. Remove inhaler from foil pouch.
Shake well before each inhalation. Prime inhaler before first use. Remove cap from mouthpiece. Hold inhaler in upright position away from face. To release spray from the mouthpiece, press down firmly on center of dose indicator until canister stops moving in actuator; soft click may be heard. Repeat 3 more times, shaking well before each spray. Repeat priming process (using only 2 sprays rather than 4) if inhaler is not used for >7 days.
Before first use, ensure that pointer on dose indicator is pointing to the right of the 120 or 30 inhalation mark in the dose indicator display window for the 120- or 28-inhalation canister, respectively. Color in the display window will change to red when there are only 20 or 10 sprays remaining in the inhaler for the 120- or 28-inhalation canister, respectively.
To administer a dose, remove cap from mouthpiece. Shake inhaler well before each use. Hold inhaler with mouthpiece pointing toward face; exhale through mouth as fully and as comfortably as possible. Close lips around mouthpiece and tilt head back, keeping tongue below mouthpiece. While inhaling slowly and deeply, press down on center of dose indicator until canister stops moving in actuator and spray is released, then stop pressing. After inhaling, remove mouthpiece and hold breath as long as comfortably possible, up to 10 seconds, then breathe out gently. Repeat process for second inhalation. Replace cap on mouthpiece immediately after use.
Clean inhaler once weekly to avoid drug buildup, which can block spray through the mouthpiece. To clean inhaler, first remove canister from actuator; do not clean canister or allow it to get wet. Remove cap from mouthpiece. Rinse actuator under warm water for about 30 seconds. Turn actuator upside down; rinse actuator again through mouthpiece for about 30 seconds. Shake as much water off mouthpiece as possible. Check the actuator and mouthpiece; if any drug buildup remains, repeat rinsing procedure. Allow the actuator to dry overnight. Do not put canister back into the actuator while wet. When the actuator is dry, gently press canister down into it; do not press too hard on canister since this may cause drug release. Prime inhaler after each cleaning by shaking well and releasing 2 sprays into the air away from face.
After priming of the oral aerosol inhaler containing glycopyrrolate/formoterol (Bevespi Aerosphere), each actuation of the inhaler delivers 10.4 mcg of glycopyrrolate (equivalent to 8.3 mcg of glycopyrronium) and 5.5 mcg of formoterol fumarate from the valve. Dosage is expressed in terms of drug delivered from the actuator; each actuation of the inhaler delivers 9 mcg of glycopyrrolate (equivalent to 7.2 mcg of glycopyrronium) and 4.8 mcg of formoterol fumarate from the mouthpiece. Actual amount of drug delivered to the lungs depends on factors such as patient's coordination between actuation of the device and inspiration through the delivery system. The Bevespi Aerosphere inhalation aerosol delivers 28 or 120 metered sprays per 5.9- or 10.7-g canister, respectively.
Dosage
Pediatric Patients
Drooling
Oral (Solution)
Children and adolescents 3–16 years of age: Initial dosage of 0.02 mg/kg 3 times daily; may titrate in increments of 0.02 mg/kg every 5–7 days based on therapeutic response and tolerance.
Surgery
Preoperatively to Decrease Secretions and Block Cardiac Vagal Reflexes
IM0.004 mg/kg given 30–60 minutes prior to the anticipated time of induction of anesthesia or at the time other preanesthetic medications (e.g., opiates, sedatives) are administered.
Children 1 month to 2 years of age may require dose of up to 0.009 mg/kg.
Intraoperatively to Prevent Cholinergic Effects
IV0.004 mg/kg (maximum 0.1 mg); may repeat as needed at intervals of 2–3 minutes. However, intraoperative doses rarely are needed in children because of long duration of antimuscarinic effects of preoperative dose.
Muscarinic Blockade during Anticholinesterase Reversal of Curariform Neuromuscular Blockade
IV0.2 mg for each 1 mg of neostigmine methylsulfate or 5 mg of pyridostigmine bromide.
To minimize the appearance of adverse cardiac effects, administer glycopyrrolate simultaneously (e.g., mixed in the same syringe) with the anticholinesterase agent.
If bradycardia is present, administer before the anticholinesterase agent to increase pulse to 80 bpm.
Adults
COPD
Glycopyrrolate
Oral Inhalation (Powder)15.6 mcg (contents of one capsule) twice daily.
Oral Inhalation (Solution)25 mcg (contents of one single-dose vial) twice daily.
Glycopyrrolate/Formoterol Fixed Combination
Oral Inhalation (Aerosol)18 mcg of glycopyrrolate and 9.6 mcg of formoterol fumarate (2 inhalations of a preparation containing 9 mcg of glycopyrrolate/4.8 mcg of formoterol fumarate) twice daily.
Glycopyrrolate/Indacaterol Fixed Combination:
Oral Inhalation (Powder)15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol (contents of one capsule) twice daily.
Peptic Ulcer Disease
Oral (Tablets)
Initially, 1 mg 3 times daily (morning, early afternoon, and bedtime); may increase bedtime dose to 2 mg if needed to control overnight symptoms.
Alternatively, 2 mg given 2 or 3 times daily at equally spaced intervals.
Maintenance dosage of 1 mg twice daily adequate in most adults.
Adjust dosage carefully according to individual requirements and response.
IV or IM
0.1 mg administered at 4-hour intervals 3 or 4 times daily.
0.2 mg may be given when a more profound antimuscarinic effect is desired.
Some patients may need only a single dose; patient response dictates frequency of administration, up to a maximum of 4 times daily.
Surgery
Preoperatively to Decrease Secretions and Block Cardiac Vagal Reflexes
IM0.004 mg/kg given 30–60 minutes prior to the anticipated time of induction of anesthesia or at the time other preanesthetic medications (e.g., opiates, sedatives) are administered.
Intraoperatively to Prevent Cholinergic Effects
IVUsual dose is 0.1 mg; may repeat as needed at intervals of 2–3 minutes.
Muscarinic Blockade during Anticholinesterase Reversal of Curariform Neuromuscular Blockade
IV0.2 mg for each 1 mg of neostigmine methylsulfate or 5 mg of pyridostigmine bromide.
To minimize the appearance of adverse cardiac effects, administer glycopyrrolate simultaneously (e.g., mixed in the same syringe) with the anticholinesterase agent.
If bradycardia is present, administer before the anticholinesterase agent to increase pulse to 80 bpm.
Prescribing Limits
Pediatric Patients
Drooling
Oral (Solution)
Maximum 0.1 mg/kg 3 times daily (≤1.5–3 mg per dose based upon weight).
Adults
COPD
Glycopyrrolate
Oral Inhalation (Powder)Maximum 15.6 mcg (contents of one capsule) twice daily.
Oral Inhalation (Solution)Maximum 25 mcg (contents of one single-dose vial) twice daily.
Glycopyrrolate/Formoterol Fixed Combination
Oral Inhalation (Aerosol)Maximum 18 mcg of glycopyrrolate and 9.6 mcg of formoterol fumarate twice daily.
Glycopyrrolate/Indacaterol Fixed Combination
Oral Inhalation (Powder)Maximum 15.6 mcg of glycopyrrolate and 27.5 mcg of indacaterol (contents of one capsule) twice daily.
Peptic Ulcer Disease
Oral (Tablets)
Maximum 8 mg daily.
IV or IM
Maximum 4 doses daily.
Special Populations
Hepatic Impairment
IM or IV: Manufacturer makes no dosage recommendations.
Oral (solution or tablets): Manufacturers make no dosage recommendations.
Oral inhalation (powder or solution): No dosage adjustment needed for hepatic impairment.
Renal Impairment
IM or IV: Dosage reduction may be necessary. (See Renal Impairment under Cautions.)
Oral inhalation (powder or solution): No dosage adjustment needed in patients with mild to moderate renal impairment. (See Renal Impairment under Cautions.)
Geriatric Patients
IM or IV: Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Oral inhalation (powder or solution): No dosage adjustment needed.
Cautions for Glycopyrrolate
Contraindications
- Oral, IM, IV, and Oral Inhalation:
-
Known hypersensitivity to glycopyrrolate or any ingredient in the formulation.
- Oral Therapy and Prolonged Parenteral Therapy (e.g., for Treatment of Peptic Ulcer)
-
Angle-closure glaucoma.
-
Obstructive uropathy (e.g., bladder neck obstruction secondary to prostatic hypertrophy).
-
Obstructive GI disease (e.g., pyloroduodenal stenosis, achalasia).
-
Paralytic ileus.
-
Intestinal atony (especially in geriatric and debilitated patients).
-
Severe ulcerative colitis.
-
Toxic megacolon complicating ulcerative colitis.
-
Acute hemorrhage when cardiovascular status is unstable.
-
Myasthenia gravis (unless used to reduce adverse muscarinic effects of an anticholinesterase agent such as neostigmine).
-
Oral solution: Concomitant use of solid dosage forms of potassium chloride.
- Oral Inhalation
-
Glycopyrrolate/indacaterol and glycopyrrolate/formoterol fixed combinations: Patients with asthma without concomitant use of a long-term asthma controller therapy.
Warnings/Precautions
Warnings
Overdosage
Avoid overdosage. Potential risk of curariform neuromuscular blockade resulting in muscle weakness or paralysis with overdosage.
Thermoregulatory Effects
Presence of fever, exposure to high environmental temperatures, and/or physical exertion may result in heat prostration due to decreased sweating, particularly in children and geriatric patients.
CNS Effects
Risk of drowsiness. Performance of activities requiring mental alertness (e.g., operating machinery, driving a motor vehicle) may be impaired.
Intestinal Obstruction
Extreme caution in patients with diarrhea (especially in those with ileostomy or colostomy) because diarrhea may be an early sign of intestinal obstruction.
Oral solution: Monitor for constipation, especially during first 4–5 days of therapy or after a dosage increase. Intestinal pseudo-obstruction reported; may present as abdominal distension, pain, nausea, or vomiting.
Major Toxicities
Cardiovascular Effects
Caution in cardiac arrhythmias (including tachyarrhythmia), CHF, or CAD since antimuscarinics block vagal inhibition of the SA nodal pacemaker. Investigate cause of tachycardia before administering glycopyrrolate injection, since an increase in heart rate may occur.
GI Disorders
Extreme caution in known or suspected GI infections because of decreased GI motility and retention of causative organism and/or toxins.
Extreme caution in mild to moderate ulcerative colitis; large doses may suppress intestinal motility, resulting in paralytic ileus and toxic megacolon.
Caution in gastric ulcer because of delayed gastric emptying and possible antral stenosis.
Caution in esophageal reflux and hiatal hernia because of decreased gastric motility and lower esophageal sphincter pressure leading to gastric retention and reflux aggravation.
GU Disorders
Extreme caution in patients with partial obstructive uropathy or prostatic hypertrophy because of decreased tone and amplitude of contractions of ureters and bladder and resultant urinary retention. (See Contraindications under Cautions.)
Oral inhalation (powder or solution): Use with caution in patients with urinary retention. Be alert for signs and symptoms of urinary retention, especially in patients with prostatic hyperplasia or bladder neck obstruction.
General Precautions
Use of Fixed Combinations
When used in fixed combination with formoterol or indacaterol, consider cautions, precautions, contraindications, and interactions associated with formoterol or indacaterol.
Deterioration of COPD and Acute Episodes
Oral inhalation: Do not initiate in patients with acutely deteriorating COPD, which may be life-threatening.
Do not use orally inhaled glycopyrrolate for relief of acute symptoms of COPD. Not studied in patients with acute symptoms; do not use extra doses of the drug in such situations. Use a short-acting, inhaled β2-agonist as needed for acute symptoms.
Failure to respond to a previously effective dosage of orally inhaled glycopyrrolate or to a supplemental short-acting, inhaled β2-agonist (e.g., increased need for additional short-acting, inhaled β2-agonists) may indicate substantially worsening COPD. Immediately reevaluate patient and treatment regimen. Do not use extra or increased dosages of the drug in such situations.
Paradoxical Bronchospasm
Oral inhalation: Possible acute, life-threatening paradoxical bronchospasm. If paradoxical bronchospasm occurs, treat with a short-acting, inhaled β2-agonist; immediately discontinue therapy and institute alternative therapy.
Sensitivity Reactions
Oral inhalation: Immediate hypersensitivity reactions (e.g., angioedema) may occur. If hypersensitivity reactions (especially angioedema, urticaria, rash) occurs, discontinue the drug immediately and consider alternative therapy. Use glycopyrrolate and glycopyrrolate/indacaterol oral inhalation powder with caution in patients with severe hypersensitivity to milk proteins.
Neuropathy
Caution in patients with autonomic neuropathy.
Down Syndrome, Spastic Paralysis, and Brain Damage
Increased sensitivity to antimuscarinic effects (e.g., mydriasis, positive chronotropic effect).
Hypertension
Caution in hypertensive patients.
Hyperthyroidism
Caution in hyperthyroid patients.
Ophthalmic Effects
Blurred vision or sensitivity of the eyes to light may occur.
Oral inhalation: Use with caution in patients with narrow-angle glaucoma. Be alert for signs and symptoms of acute narrow-angle glaucoma.
Specific Populations
Pregnancy
IM or IV: Category B. Use during pregnancy only if clearly needed.
Oral: No controlled studies to date to establish safety during pregnancy; weigh potential benefits against risks.
Oral inhalation: Category C. No adequate and well-controlled studies in pregnant women; use during pregnancy only if potential benefits outweigh risks.
Lactation
Not known whether glycopyrrolate is distributed into milk, affects milk production, or affects the breast-fed infant. Distribution of drug and its metabolites into milk reported in rats.
Like other anticholinergics, may suppress lactation.
Use caution in nursing women. Consider benefits of breast-feeding and importance of the drug to the woman along with potential adverse effects to the breast-fed infant from the drug or from the underlying maternal condition.
Oral inhalation: Discontinue nursing or the drug.
Pediatric Use
Oral (solution): Safety and efficacy not established in pediatric patients <3 years of age.
Oral (tablets), IM, or IV: Manufacturers state safety and efficacy not established in pediatric patients (including safety and efficacy for treatment of peptic ulcer disease in pediatric patients). Use with caution; infants and young children may be more susceptible to antimuscarinic effects. Patients with Down syndrome and children with spastic paralysis or brain damage may be hypersensitive to antimuscarinic effects (e.g., mydriasis, positive chronotropic effect).
Oral inhalation: Manufacturers state safety and efficacy not established in pediatric patients.
IV: Dysrhythmias reported in pediatric patients receiving IV glycopyrrolate preoperatively or during anesthesia.
IV: Large amounts of benzyl alcohol (i.e., 100–400 mg/kg daily) associated with toxicity in neonates; each mL of glycopyrrolate injection contains 9 mg of benzyl alcohol. Manufacturer does not recommend use in neonates; AAP states that the presence of small amounts of this preservative in a commercially available injection should not proscribe its use when indicated in neonates.
Geriatric Use
Oral, IM, or IV: Use with caution; possible increased susceptibility to the adverse effects of antimuscarinics.
Oral inhalation: No overall differences in safety and efficacy observed between patients ≥65 years of age and younger adults. No dosage adjustments needed.
Hepatic Impairment
Oral, IM, or IV: Use with caution.
Oral inhalation (powder or solution): No dosage adjustments needed in patients with mild to moderate hepatic impairment. Not studied in those with severe hepatic impairment.
Oral inhalation (aerosol): Monitor closely.
Renal Impairment
Oral, IM, or IV: Use with caution. Elimination may be severely impaired. Dosage reduction may be necessary.
Oral inhalation (powder or solution): Glycopyrrolate exposure may be increased in patients with severe renal impairment. Use in those with severe renal impairment or end-stage renal disease requiring dialysis only if expected benefits outweigh potential risks. No dosage adjustment needed in patients with mild to moderate renal impairment.
Oral inhalation (aerosol): Use in patients with severe renal impairment or end-stage renal disease requiring dialysis only if expected benefit outweighs potential risk.
Common Adverse Effects
Oral (tablets), IM, or IV: Xerostomia, decreased sweating, urinary hesitancy and retention, blurred vision, tachycardia, palpitations, dilatation of the pupil, cycloplegia, increased ocular tension, loss of taste, headaches, nervousness, mental confusion, drowsiness, weakness, dizziness, insomnia, nasal congestion, sinusitis, upper respiratory tract infection, constipation, nausea, vomiting, bloated feeling, impotence, allergic reaction, urticaria. Ocular and CNS effects are less common with glycopyrrolate than with tertiary amine antimuscarinics.
Oral (solution): Dry mouth, vomiting, constipation, flushing, nasal congestion.
Oral inhalation (powder): Upper respiratory tract infection, nasopharyngitis, urinary tract infection, sinusitis, oropharyngeal pain, diarrhea, nausea, upper abdominal pain, fatigue, bronchitis, pneumonia, rhinitis, nasal congestion, back pain, arthralgia, dyspnea, wheezing.
Oral inhalation (solution): Dyspnea, diarrhea, upper respiratory tract infection, peripheral edema, bronchitis, nasopharyngitis, pneumonia, sinusitis, urinary tract infection, back pain, headache, cough, oropharyngeal pain, hypertension.
Drug Interactions
Orally Administered Drugs
Potential pharmacokinetic interaction (altered GI absorption of various drugs); antimuscarinics may inhibit GI motility, delay gastric emptying, and prolong GI transit time.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β2-Adrenergic agonists |
Glycopyrrolate oral inhalation: No interactions reported |
|
|
Amantadine |
Possible additive anticholinergic effects |
Use concomitantly with caution; consider reducing dosage of glycopyrrolate |
|
Antacids |
Possible decreased absorption of antimuscarinic |
Administer oral glycopyrrolate at least 1 hour before antacids |
|
Antiarrhythmic agents (quinidine, disopyramide, procainamide) |
Possible additive anticholinergic effects |
Use concomitantly with caution |
|
Anticholinergic drugs |
Possible additive anticholinergic effects |
Glycopyrrolate oral inhalation: Avoid concomitant use with other anticholinergic-containing drugs |
|
Antidepressants, tricyclic |
Possible additive anticholinergic effects |
Use concomitantly with caution |
|
Antihistamines (meclizine) |
Possible additive anticholinergic effects |
Use concomitantly with caution |
|
Antiparkinsonian agents |
Possible additive anticholinergic effects |
Use concomitantly with caution |
|
Atenolol |
Possible increased bioavailability of atenolol |
May need to reduce atenolol dosage |
|
Cimetidine |
Possible increase in glycopyrrolate exposure |
|
|
Corticosteroids |
Possible increased IOP Glycopyrrolate oral inhalation: No interactions reported with oral or inhaled corticosteroids |
|
|
Digoxin |
Digoxin slow dissolution tablets: Possible increased concentrations and effects of digoxin |
Monitor for increased digoxin concentrations; consider alternative digoxin dosage forms (e.g., capsules, elixir) |
|
Haloperidol |
Possible decreased haloperidol concentrations; possible worsening of schizophrenic symptoms and development of tardive dyskinesia |
Closely monitor if concomitant use cannot be avoided |
|
Ketoconazole |
Possible decreased ketoconazole absorption |
If concomitant therapy is necessary, give antimuscarinic at least 2 hours after ketoconazole |
|
Levodopa |
Possible increased gastric metabolism of levodopa and decreased levodopa absorption in the small intestine |
Toxicity may result from increased levodopa absorption if antimuscarinic is discontinued without a concomitant reduction in levodopa dosage Consider increasing levodopa dosage when glycopyrrolate therapy initiated |
|
Meperidine |
Possible additive anticholinergic effects |
Use concomitantly with caution |
|
Metformin |
Possible increase in metformin concentrations and effects |
Monitor clinical response to metformin and reduce dosage if needed |
|
Methylxanthines |
Glycopyrrolate oral inhalation: No interactions reported |
|
|
Phenothiazines |
Possible additive anticholinergic effects |
Use concomitantly with caution |
|
Potassium chloride |
Glycopyrrolate may potentiate potassium chloride’s local GI mucosal effects Glycopyrrolate oral solution: Passage of potassium chloride tablets through the GI tract may be arrested or delayed |
Use glycopyrrolate cautiously with potassium chloride preparations (especially wax-matrix preparations); monitor carefully for evidence of GI mucosal lesions Glycopyrrolate oral solution: Concomitant use with solid oral dosage forms of potassium chloride contraindicated |
|
Skeletal muscle relaxants |
Possible additive anticholinergic effects |
Use concomitantly with caution |
Glycopyrrolate Pharmacokinetics
Absorption
Bioavailability
Incompletely absorbed from the GI tract.
Following oral administration of glycopyrrolate tablets in children, mean absolute bioavailability was low (about 3%) and variable (range: 1–13%).
Following oral administration of glycopyrrolate solution, mean time to peak concentrations is about 3 hours.
Rapidly absorbed following IM injection.
Following oral inhalation of glycopyrrolate powder via the Neohaler device, drug is rapidly absorbed with peak plasma concentrations at 5 minutes. Absolute bioavailability of about 40%; 90% of systemic exposure resulting from lung absorption and 10% from GI absorption. Steady-state concentrations achieved within 1 week following repeated once-daily inhalation; no evidence of changes in pharmacokinetics over time. Linear pharmacokinetics observed following inhalation of 31.2–249.6 mcg daily.
Following oral inhalation of glycopyrrolate solution via the Magnair nebulizer system, drug is rapidly absorbed with peak plasma concentrations occurring within 20 minutes. Steady-state concentrations achieved within 1 week of treatment initiation; 2- to 3-fold accumulation of systemic drug exposure observed at steady state following twice-daily dosing.
Onset
Following IV administration, onset of action generally occurs within 1 minute.
Following IM injection, effects are evident within 15–30 minutes and peak within 30–45 minutes.
Duration
Following oral administration, anticholinergic effects may persist for up to 8–12 hours.
Following parenteral administration, vagal blocking effects persist for 2–3 hours and the antisialogue effects persist up to 7 hours.
Effect of Food
Oral solution: Administration with a high-fat meal decreases absorption.
Distribution
Extent
Rapidly distributed throughout the body with highest concentrations in the stomach and intestine following IV administration in animals.
Distributed into bile.
Does not readily cross lipid membranes; does not readily cross the blood-brain barrier or penetrate the eye.
Glycopyrrolate crosses the placenta to a limited extent; not known whether distributed into milk.
Plasma Protein Binding
38–41% at concentrations of 1–10 ng/mL in vitro.
Elimination
Metabolism
Small amounts are metabolized to one or more metabolites.
Orally inhaled glycopyrrolate: In vitro studies show hydroxylation resulting in a variety of mono- and bis-hydroxylated metabolites and direct hydrolysis resulting in formation of a carboxylic acid derivative (M9).
Multiple CYP isoenzymes appear to contribute to oxidative biotransformation of glycopyrrolate; hydrolysis to M9 likely catalyzed by members from the cholinesterase family presystemically and/or via first- pass metabolism from the swallowed dose fraction of orally inhaled drug.
Elimination Route
Excreted principally as unchanged drug in feces via biliary excretion and in urine. In adults, approximately 65–80% of an IV dose eliminated in urine as unchanged drug.
Following repeated oral inhalation, glucuronide and/or sulfate conjugates found in urine, accounting for about 3% of inhaled dose.
Renal elimination of parent drug accounts for about 60–70% of systemically available glycopyrrolate following oral inhalation; active tubular secretion contributes to renal clearance. Most nonrenal clearance believed to result from metabolism, with biliary clearance contributing a small role.
Half-life
IV: About 50 minutes in adults, 19–99 minutes in children, and 22–130 minutes in infants.
IM: About 33–75 minutes.
Oral solution: About 3 hours.
Oral inhalation powder: 33–53 hours.
Special Populations
In patients undergoing renal transplantation, half-life of IV glycopyrrolate is prolonged to 47 minutes compared with 19 minutes in healthy individuals.
Systemic exposure increased in patients with renal failure.
Oral inhalation powder: Systemic exposure increased by 1.4-fold in patients with mild to moderate renal failure and 2.2-fold in those with severe renal impairment and end-stage renal disease.
Oral inhalation solution: Effects of renal impairment on pharmacokinetics not studied to date.
Pharmacokinetics not evaluated in patients with hepatic impairment.
Oral inhalation powder: Age, body weight, race, gender, or smoking status did not produce clinically relevant effects on systemic drug exposure.
Oral inhalation solution: Age, body weight, or race did not produce clinically relevant effects on systemic drug exposure.
Stability
Storage
Oral Inhalation
Aerosol
Glycopyrrolate/formoterol: 20–25°C (may be exposed to 15–30°C). Discard 3 months after foil pouch opened or when dose indicator reads “0”, whichever comes first.
Powder
Glycopyrrolate and glycopyrrolate/indacaterol: 25°C (may be exposed to 15–30°C).
Keep dry-powder capsules in the foil-sealed blisters until immediately before use. Remove one capsule immediately before use. Discard capsules if opened and exposed to air (i.e., not used immediately).
Solution
Glycopyrrolate: 20–25°C.
Store single-dose vials in protective foil pouch. After opening pouch, return unused vials to pouch for storage; discard any vials not used within 7 days of opening pouch. Discard vials containing solution that is not colorless.
Oral
Solution
20–25°C (may be exposed to 15–30°C).
Tablets
20–25°C in tight containers (may be exposed to 15–30°C).
Parenteral
Injection
20–25°C.
Compatibility
Parenteral
Solution Compatibility
If the pH of the admixture is >6, rapid ester hydrolysis of glycopyrrolate generally occurs.
|
Compatible |
|---|
|
Dextrose 5% in sodium chloride 0.45% |
|
Dextrose 5 or 10% in water |
|
Ringer’s injection |
|
Sodium chloride 0.9% |
|
Incompatible |
|
Ringer’s injection, lactated |
Drug Compatibility
Generally incompatible with drugs that have a pH >6. If the pH of the admixture is >6, rapid ester hydrolysis of glycopyrrolate generally occurs.
|
Compatible |
|---|
|
Buprenorphine HCl with haloperidol lactate |
|
Incompatible |
|
Methylprednisolone sodium succinate |
|
Compatible |
|---|
|
Propofol |
|
Palonosetron HCl |
|
Compatible |
|---|
|
Atropine sulfate |
|
Buprenorphine HCl with haloperidol lactate |
|
Butorphanol tartrate |
|
Chlorpromazine HCl |
|
Codeine phosphate |
|
Diphenhydramine HCl |
|
Droperidol |
|
Fentanyl citrate |
|
Hydromorphone HCl |
|
Hydroxyzine HCl |
|
Levorphanol tartrate |
|
Lidocaine HCl |
|
Meperidine HCl |
|
Midazolam HCl |
|
Morphine sulfate |
|
Nalbuphine HCl |
|
Neostigmine methylsulfate |
|
Ondansetron HCl |
|
Oxymorphone HCl |
|
Physostigmine salicylate |
|
Procaine HCl (no longer commercially available in US) |
|
Prochlorperazine edisylate |
|
Promethazine HCl |
|
Pyridostigmine bromide |
|
Ranitidine HCl |
|
Scopolamine HBr |
|
Trimethobenzamide HCl |
|
Incompatible |
|
Chloramphenicol sodium succinate |
|
Dexamethasone sodium phosphate |
|
Diazepam |
|
Dimenhydrinate |
|
Methohexital sodium |
|
Pentazocine lactate |
|
Pentobarbital sodium |
|
Secobarbital sodium |
|
Sodium bicarbonate |
|
Thiopental sodium (no longer commercially available in US) |
Actions
-
Glycopyrrolate competitively inhibits acetylcholine or other cholinergic stimuli at autonomic effectors innervated by postganglionic cholinergic nerves and, to a lesser extent, on smooth muscles that lack cholinergic innervation.
-
At usual doses, principally antagonizes cholinergic stimuli at muscarinic receptors and has little or no effect on cholinergic stimuli at nicotinic receptors.
-
At high doses, may produce substantial ganglionic blockade with resultant adverse effects (e.g., impotence, postural hypotension); in overdosage, may cause curariform neuromuscular blockade.
-
Antimuscarinics also referred to as anticholinergics (cholinergic blocking agents), but this term is appropriate only when it describes the antagonism of cholinergic stimuli at any cholinergic receptor, whether muscarinic or nicotinic.
-
Also referred to as parasympatholytics since the antagonized functions principally are under the parasympathetic division of the nervous system.
-
Receptors at various sites are not equally sensitive to inhibition of muscarinic effects. Relative sensitivity of physiologic functions (proceeding from the most sensitive) is as follows: secretions of the salivary, bronchial, and sweat glands; pupillary dilation; ocular accommodation, and heart rate; contraction of the detrusor muscle of the bladder and smooth muscle of the GI tract; and gastric secretion and motility. Doses used to decrease gastric secretions are likely to cause dryness of the mouth (xerostomia) and interfere with visual accommodation, and possibly cause difficulty in urinating.
-
Competitively and reversibly inhibits the actions of acetylcholine and other cholinergic stimuli at M3 receptors in the smooth muscle of the respiratory tract resulting in bronchodilation.
Advice to Patients
-
A copy of the manufacturer's patient information (medication guide) and instructions for use must be provided to all patients each time glycopyrrolate for oral inhalation (alone or in fixed combination with formoterol or indacaterol) is dispensed. Importance of instructing patients to read the patient information and instructions for use prior to initiation of therapy and each time the prescription is refilled.
-
Importance of understanding proper storage, preparation, and inhalation techniques, including use of the drug-specific oral inhalation device.
-
When using glycopyrrolate or glycopyrrolate/indacaterol dry-powder capsules for oral inhalation, importance of advising patients not to swallow the capsules or to use them with any capsule inhaler other than the Neohaler device. Importance of advising patients to use the new inhaler handset provided with each new prescription.
-
Importance of adherence to oral inhalation dosing schedules, including not altering the dose or frequency of use of such drugs, unless otherwise instructed by a clinician.
-
Advise patients that if an oral inhalation dose of glycopyrrolate alone or in fixed combination with formoterol or indacaterol is missed, the next dose should be taken at the regularly scheduled time; importance of not using more than one capsule or vial at a time or more than 2 capsules or vials in one day or using inhaler more frequently than recommended.
-
Advise patients that oral inhalation therapy with glycopyrrolate alone or in fixed combination with formoterol or indacaterol does not relieve acute COPD symptoms; importance of not using extra doses for such symptoms.
-
Importance of all patients being provided with and instructed in the use of a short-acting, inhaled β2-adrenergic agonist (e.g., albuterol) for treatment of acute COPD symptoms.
-
When initiating oral inhalation therapy with glycopyrrolate in fixed combination with formoterol or indacaterol, importance of discontinuing regular use of short-acting, inhaled β2-agonists and using them only to relieve acute symptoms.
-
Importance of contacting a clinician immediately if symptoms worsen or the short-acting, inhaled β2-agonist becomes less effective or more inhalations than usual are required to relieve symptoms.
-
Importance of patients not discontinuing oral inhalation therapy without medical supervision, since symptoms may recur after discontinuance.
-
Advise patients of the risk of paradoxical bronchospasm with use of oral inhalation therapy. If paradoxical bronchospasm occurs, discontinue the drug.
-
When oral inhalation therapy with glycopyrrolate in fixed combination with formoterol or indacaterol is used, importance of informing patients of important cautionary information about formoterol or indacaterol.
-
When glycopyrrolate oral solution is used, important of administering the oral solution at least 1 hour before or 2 hours after meals. Importance of using an accurate measuring device to administer the oral solution.
-
Importance of not increasing the dosage of glycopyrrolate oral solution without contacting a clinician.
-
Advise patients or caregivers that if troublesome adverse effects develop following a dosage increase of glycopyrrolate oral solution, importance of returning to the previous dosage and contacting a clinician.
-
Advise patients that urinary hesitancy or retention may occur; importance of contacting a clinician immediately if signs or symptoms of urinary retention (e.g., difficulty passing urine, painful urination) occur.
-
Advise patients that dry mouth or sensitivity of eyes to light may occur.
-
Importance of contacting a clinician immediately if signs or symptoms of acute narrow-angle glaucoma (e.g., eye pain or discomfort, blurred vision, visual halos or colored images in association with red eyes from conjunctival congestion or corneal edema) occur.
-
Importance of advising patients that constipation, vomiting, or flushing of the skin or face may occur. If constipation occurs in a patient receiving glycopyrrolate oral solution, importance of discontinuing the drug and contacting a clinician.
-
Importance of advising patients that if rash, hives, or allergic reaction occurs during therapy with glycopyrrolate oral solution, discontinue the drug and contact a clinician.
-
Risk of hyperthermia and heat prostration; importance of advising patients to avoid exposure to high environmental temperatures and avoid use when febrile.
-
Risk of dizziness, drowsiness, or blurred vision; importance of advising patients to avoid activities requiring mental alertness and/or visual acuity (e.g., driving, operating machinery, hazardous work) until effects on individual are known.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
0.2 mg/mL |
Cuvposa |
Merz |
|
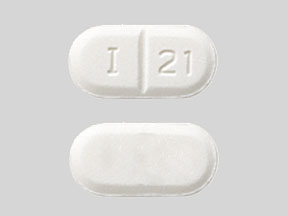
Tablets |
1 mg* |
Glycopyrrolate Tablets |
||
|
Robinul (scored) |
Shionogi |
|||
|
2 mg* |
Glycopyrrolate Tablets |
|||
|
Robinul Forte (scored) |
Shionogi |
|||
|
Oral Inhalation |
Powder, for inhalation (contained in capsules) |
15.6 mcg |
Seebri Neohaler |
Sunovion |
|
Solution, for nebulization |
25 mcg/mL |
Lonhala Magnair |
Sunovion |
|
|
Parenteral |
Injection |
0.2 mg/mL* |
Robinul |
West-ward |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral Inhalation |
Aerosol |
9 mcg with Formoterol Fumarate 4.8 mcg per metered spray |
Bevespi Aerosphere (with hydrofluoroalkane propellant) |
AstraZeneca |
|
Powder, for inhalation (contained in capsules) |
15.6 mcg with Indacaterol 27.5 mcg |
Utibron Neohaler |
Sunovion |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions December 2, 2012. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about glycopyrrolate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (18)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: anticholinergic bronchodilators
- Breastfeeding
Patient resources
Professional resources
- Glycopyrrolate Injection prescribing information
- Glycopyrrolate Oral Solution (FDA)
- Glycopyrrolate Tablets (FDA)
Other brands
Robinul, Cuvposa, Seebri Neohaler, Dartisla ODT, ... +2 more