Anagrelide (Monograph)
Brand name: Agrylin
Drug class: Platelet-reducing Agents
VA class: BL400
Chemical name: 6,7-dichloro-1,5-dihydroimidazo[2,1-b]quinazolin-2(3H)-one monohydrochloride monohydrate
CAS number: 58579-51-4; 68475-42-3
Introduction
Platelet-reducing agent; imidazoquinazoline derivative.
Uses for Anagrelide
Thrombocythemia
Reduction of elevated platelet counts and associated risk of thromboembolic and hemorrhagic events in patients with thrombocythemia secondary to essential thrombocythemia (ET) and other myeloproliferative disorders. Has been designated an orphan drug by FDA for the treatment of ET.
Management of ET generally based on a risk-stratification approach. Treatment with a cytoreductive agent (e.g., anagrelide, hydroxyurea) usually reserved for patients at high risk (i.e., age >60 years, previous history of thrombosis, and/or platelet count ≥1,500,000/mm3) of developing thromboembolic and/or hemorrhagic complications. Some clinicians also recommend cytoreductive therapy in intermediate-risk ET patients (e.g., 40–60 years of age, platelet count >1,000,000/mm3, and cardiovascular risk factor [smoking, arterial hypertension, hypercholesterolemia, or diabetes mellitus] or familial thrombophilia).
Hydroxyurea (often combined with low-dose aspirin) generally considered drug of choice in high-risk patients with ET because of proven efficacy and infrequent acute toxicity. However, because of potential leukemogenic effects with hydroxyurea when used long term or sequentially with other cytotoxic drugs, anagrelide or interferon alfa suggested as alternative therapy in high-risk patients, particularly younger patients (<40–60 years of age), and in those who do not respond to or cannot tolerate hydroxyurea. Consider cautious use of low-dose aspirin concomitantly with anagrelide based on relative risks of thrombosis and arterial hemorrhage in individual patients. (See Specific Drugs or Foods under Interactions.)
Anagrelide Dosage and Administration
General
-
Initiate therapy under close supervision of a clinician.
-
Monitor platelet counts every 2 days for 1 week following initiation of therapy, then at least weekly thereafter until maintenance dosage established.
Administration
Oral Administration
Administer orally without regard to meals.
Dosage
Available as anagrelide hydrochloride; dosage expressed in terms of anagrelide.
Pediatric Patients
Thrombocythemia
Oral
Children and adolescents 7–14 years of age: Initially, 0.5 mg daily. Initial dosages up to 0.5 mg 4 times daily have been used.
Maintain initial dosage for ≥1 week, then adjust to lowest effective dosage that will maintain platelet counts <600,000/mm3 or ideally within normal range. Usual maintenance dosage is 1.5–3 mg daily.
Increase dosage by ≤0.5 mg daily in any 1-week period.
Continue therapy indefinitely if adequate response achieved.
Adults
Thrombocythemia
Oral
Initially, 0.5 mg 4 times daily or 1 mg twice daily recommended by manufacturer. Lower dosages (e.g., 0.5 mg twice daily) have been used and may improve tolerability.
Maintain initial dosage for ≥1 week, then adjust to lowest effective dosage that will maintain platelet counts <600,000/mm3 or ideally within normal range (e.g., 150,000–400,000/mm3). Usual maintenance dosage is 1.5–3 mg daily.
Increase dosage by ≤0.5 mg daily in any 1-week period.
Continue therapy indefinitely if adequate response achieved.
Prescribing Limits
Pediatric Patients
Thrombocythemia
Oral
Children and adolescents 7–14 years of age: Maximum 10 mg daily or 2.5 mg as a single dose.
Adults
Thrombocythemia
Oral
Maximum 10 mg daily or 2.5 mg as a single dose.
Special Populations
Hepatic Impairment
In patients with moderate hepatic impairment, reduce initial dosage to 0.5 mg daily and maintain for ≥1 week. Increase dosage by ≤0.5 mg daily in any 1-week period. (See Hepatic Impairment under Cautions.)
Contraindicated in severe hepatic impairment.
Renal Impairment
Dosage adjustment not required in patients with renal impairment.
Cautions for Anagrelide
Contraindications
Severe hepatic impairment.
Warnings/Precautions
Warnings
Cardiovascular Effects
Adverse cardiovascular effects (e.g., vasodilation, tachycardia, palpitations, edema, CHF) reported with usual dosages of anagrelide, including rare cases of sudden death. Assess risk versus benefits of therapy. Use with caution, if at all, in patients with known or suspected cardiovascular disease. Evaluate cardiac status prior to and during therapy. Consider reduced dosages. Some clinicians recommend immediate discontinuance of therapy if any evidence of cardiac dysfunction occurs.
Temporary decreases in BP reported, usually during treatment initiation; BP appears to normalize during maintenance therapy.
General Precautions
Laboratory Monitoring
Monitor CBCs, liver function tests, and renal function tests while platelet counts are being decreased, usually during first 2 weeks of therapy.
To assess response to therapy and prevent thrombocytopenia, monitor platelet counts every 2 days for first week of therapy, then at least weekly thereafter until maintenance dosage achieved.
Rebound Thrombocythemia
A rapid (e.g., within 4 days) increase in platelet count generally is observed when anagrelide is discontinued or interrupted. Continue treatment indefinitely (if adequate response achieved) to prevent rebound thrombocythemia.
Anemia
Decreases in hemoglobin and hematocrit (anemia) reported, usually with long-term use.
Bleeding Tendency
Concomitant use with aspirin may increase bleeding tendency. (See Specific Drugs and Foods under Interactions.) Use caution with such combined therapy. Some clinicians suggest that aspirin not be used concomitantly with anagrelide in patients with history of bleeding.
Renal Effects
Renal impairment reported in a few patients following treatment with anagrelide; most patients had preexisting renal impairment. Monitor renal function while platelet counts are being decreased.
Fetal/Neonatal Morbidity
Safety of use during pregnancy not established; embryotoxicity and fetotoxicity demonstrated in animals. Generally not recommended in pregnant women unless potential benefits outweigh possible risks to fetus. Women of childbearing potential should avoid pregnancy and use contraception during therapy.
Specific Populations
Pregnancy
Category C.
Lactation
Not known whether anagrelide is distributed into human milk. Discontinue nursing or drug because of potential risk in nursing infants.
Pediatric Use
Evaluated in a limited number of children and adolescents 7–14 years of age with thrombocythemia secondary to myeloproliferative disorders; preliminary data suggest no overall differences in dosage or adverse effects relative to adults.
Geriatric Use
Response in patients ≥65 years of age does not appear to differ from that in younger adults. Use with caution because of age-related decreases in hepatic, renal, and/or cardiac function.
Hepatic Impairment
Extensively metabolized in liver; possible increased systemic exposure to anagrelide in patients with hepatic impairment. (See Elimination: Special Populations, under Pharmacokinetics.)
Weigh risks of therapy against potential benefits in patients with mild to moderate hepatic impairment. Reduce dosage and carefully monitor for adverse cardiovascular effects or other manifestations of toxicity. (See Hepatic Impairment under Dosage and Administration and see Cardiovascular Effects under Cautions.)
Contraindicated in patients with severe hepatic impairment.
Renal Impairment
Closely monitor patients with known or suspected renal impairment for cardiovascular effects or other manifestations of toxicity.
Common Adverse Effects
Headache, palpitations, diarrhea, asthenia, edema, nausea, abdominal pain, dizziness, pain, dyspnea, flatulence, vomiting, fever, peripheral edema, rash, chest pain, anorexia, tachycardia, pharyngitis, malaise, cough, paresthesia, back pain, pruritus, dyspepsia.
Drug Interactions
Metabolized partially by CYP1A2; inhibits CYP1A2 to a limited extent.
Inhibits phosphodiesterase (PDE) type 3.
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors of CYP1A2: Potential pharmacokinetic interaction (decreased clearance of anagrelide).
Drugs Metabolized by Hepatic Microsomal Enzymes
CYP1A2 substrates: Potential pharmacokinetic interaction (decreased clearance of substrate).
Specific Drugs or Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Aspirin |
No clinically important interaction observed in vivo; however, potential for increased risk of bleeding due to additive platelet inhibition |
Use concomitantly with caution, considering individual risks of thrombosis and bleeding; carefully monitor for bleeding |
|
Digoxin |
Pharmacokinetic interaction unlikely |
|
|
Fluvoxamine |
Possible decreased clearance of anagrelide |
|
|
Grapefruit juice |
Possible decreased clearance of anagrelide |
|
|
Omeprazole |
Possible decreased clerance of anagrelide |
|
|
PDE type 3 inhibitors (e.g., amrinone, cilostazol, milrinone) |
Possible additive pharmacologic effects |
Use with caution |
|
Sucralfate |
Possible decreased absorption of anagrelide |
|
|
Theophylline |
Possible decreased clearance of theophylline |
|
|
Warfarin |
Pharmacokinetic interaction unlikely |
Anagrelide Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.
Following oral administration, peak plasma concentrations attained within 1–2 hours.
No evidence of drug accumulation following multiple dosing.
Onset
Platelet counts usually begin to decrease within 7–14 days. Complete response (e.g., platelet count ≤600,000/mm3) generally achieved within 4–12 weeks.
Food
Food decreases peak plasma concentrations by 14% and increases AUC by 20%; not clinically important.
Special Populations
In children and adolescents 7–14 years of age, AUC and peak plasma anagrelide concentrations lower than those in adults 16–86 years of age.
Distribution
Extent
Distributes extensively into large peripheral compartment.
Crosses placenta.
Elimination
Metabolism
Extensively metabolized in liver to at least 4 metabolites, including an active hydroxylated derivative (3-hydroxyanagrelide).
Undergoes first-pass metabolism by CYP1A2 to 3-hydroxyanagrelide.
Elimination Route
Excreted principally in urine as metabolites (>70%) and unchanged drug (<1%). Approximately 10% excreted in feces through bile.
Half-life
Anagrelide: Approximately 1.3 hours after a single 0.5-mg dose under fasting conditions.
3-Hydroxyanagrelide: Approximately 3 hours.
Special Populations
Systemic exposure increased eightfold in patients with moderate hepatic impairment compared with that in healthy individuals.
Severe renal impairment (Clcr <30 mL/minute) does not appear to affect pharmacokinetics of anagrelide.
Possible decreased clearance and prolonged half-life in geriatric patients.
Stability
Storage
Oral
Tablets
25°C in light-resistant container; may be exposed to 15–30°C.
Actions
-
Exact mechanism of action not fully elucidated; thought to reduce platelet counts in a dose-related manner by selectively inhibiting megakaryocyte maturation during postmitotic stage of development. Reduces size and ploidy of megakaryocytes, but does not appear to affect platelet function or bleeding time.
-
Acts selectively on megakaryocytes with minimal or no effect on other blood-cell precursors. Current data suggest no long-term leukemogenicity.
-
Inhibits phospholipase A2 and phosphodiesterase (PDE) type 3 activity in platelets; results in increased concentrations of cyclic adenosine monophosphate (cAMP). Such increases in cAMP may produce an anti-aggregating effect on platelets at dosages substantially higher than those required to cause thrombocytopenia.
-
Exerts positive inotropic and vasodilatory effects through inhibition of cAMP PDE type 3 in myocardium; such actions may result in adverse cardiovascular effects.
Advice to Patients
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Advise women of childbearing potential to avoid pregnancy and use effective contraception while taking anagrelide. If pregnancy occurs, apprise patient of potential risk to fetus.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses (e.g., liver disease).
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
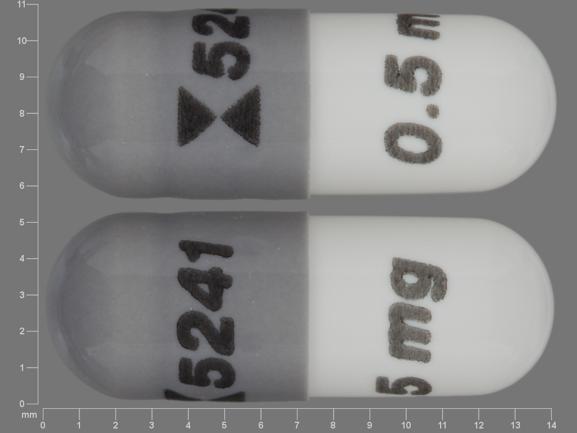
Oral |
Capsules |
0.5 mg (of anagrelide)* |
Agrylin |
Shire |
|
Anagrelide Hydrochloride Capsules |
Barr |
|||
|
1 mg (of anagrelide)* |
Agrylin |
Shire |
||
|
Anagrelide Hydrochloride Capsules |
Barr |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions September 1, 2008. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about anagrelide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (3)
- Drug images
- Latest FDA alerts (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous coagulation modifiers
- Breastfeeding
- En español