Abiraterone Acetate (Monograph)
Brand names: Zytiga, Yonsa
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; inhibitor of 17α-hydroxylase/C17,20-lyase (CYP17).
Uses for Abiraterone Acetate
Prostate Cancer
Conventional abiraterone: In combination with prednisone for the treatment of metastatic castration-resistant prostate cancer.
Micronized abiraterone: In combination with methylprednisolone for the treatment of metastatic castration-resistant prostate cancer. Efficacy determined based on studies evaluating conventional abiraterone.
Conventional abiraterone: In combination with prednisone for the treatment of high-risk metastatic castration-sensitive prostate cancer. Guidelines recommend androgen deprivation therapy combined with abiraterone, apalutamide, enzalutamide, or docetaxel for the treatment of metastatic noncastrate (hormone-sensitive) prostate cancer.
Abiraterone plus prednisolone and androgen deprivation therapy (ADT) for the treatment of nonmetastatic castration-sensitive prostate cancer † [off-label] has Level 2 (moderate strength/quality) evidence supporting its use. Currently available data include results from a multigroup, multistage platform design study with randomization and an open-label treatment approach. Based on these data, abiraterone plus prednisolone and ADT should be considered for men with nonmetastatic, castration-sensitive, locally advanced prostate cancer. Nonmetastatic patients with node-positive disease should also receive radiotherapy and those without lymph node involvement should have high-risk features as noted in the STAMPEDE trial in order to receive abiraterone combination therapy.
Abiraterone Acetate Dosage and Administration
General
Pretreatment Screening
-
Obtain baseline serum ALT, AST, and bilirubin concentrations.
-
Assess BP prior to initiation of abiraterone; BP must be controlled prior to initiation of the drug.
-
Assess serum potassium concentration; correct hypokalemia prior to initiation of the drug.
Patient Monitoring
-
Monitor serum ALT, AST, and bilirubin concentrations every 2 weeks for the first 3 months of therapy and monthly thereafter; in patients with preexisting moderate hepatic impairment, monitor serum ALT, AST, and bilirubin concentrations every week for the first month of therapy, every 2 weeks for the following 2 months of therapy, and then monthly thereafter.
-
In patients who develop hepatotoxicity during abiraterone therapy and resume treatment with the drug, serum ALT, AST, and bilirubin concentrations should be monitored at a minimum of every 2 weeks for the first 3 months and then monthly thereafter.
-
Monitor BP, serum potassium concentration, and fluid status monthly. More frequent monitoring may be necessary in patients with a history of cardiovascular disease or other cardiac-related comorbidities.
-
Monitor for signs and symptoms of adrenocortical insufficiency.
-
Monitor blood glucose concentrations in patients with diabetes mellitus.
Dispensing and Administration Precautions
-
Abiraterone acetate is commercially available as conventional tablets (Zytiga) and micronized tablets (Yonsa); these formulations are not interchangeable due to differences in dosage, indication, and food effects.
- Handling and Disposal
-
Females who are or may be pregnant should not handle abiraterone acetate tablets without protection (e.g., gloves).
Other General Considerations
-
Use concurrently with a gonadotropin-releasing hormone (GnRH) analog unless the patient has undergone bilateral orchiectomy.
Administration
Oral Administration
Conventional abiraterone: Administer orally once daily on an empty stomach; consume no food for at least 2 hours before or 1 hour after a dose.
Micronized abiraterone: Administer orally once daily with or without food.
Administer tablets whole with water; do not chew or crush.
Dosage
Available as abiraterone acetate; dosage expressed in terms of the salt.
Conventional and micronized formulations are not interchangeable.
Adults
Prostate Cancer
Metastatic Castration-resistant Prostate Cancer
Oral (Conventional Abiraterone)1 g once daily in combination with prednisone 5 mg orally twice daily.
Avoid concomitant use of potent CYP3A4 inducers; if concomitant use cannot be avoided, increase dosing frequency of abiraterone acetate from once daily to twice daily (e.g., from 1 g once daily to 1 g twice daily).
Oral (Micronized Abiraterone)500 mg once daily in combination with methylprednisolone 4 mg orally twice daily.
Avoid concomitant use of potent CYP3A4 inducers; if concomitant use cannot be avoided, increase dosing frequency of abiraterone acetate from once daily to twice daily (e.g., from 500 mg once daily to 500 mg twice daily).
Metastatic Castration-sensitive Prostate Cancer
Oral (Conventional Abiraterone)1 g once daily in combination with prednisone 5 mg orally once daily.
Avoid concomitant use of potent CYP3A4 inducers; if concomitant use cannot be avoided, increase dosing frequency of abiraterone acetate from once daily to twice daily (e.g., from 1 g once daily to 1 g twice daily).
Nonmetastatic Castration-sensitive Prostate Cancer
OralWhen abiraterone is used in combination with prednisolone and androgen deprivation therapy (ADT) for the treatment of nonmetastatic castration-sensitive prostate cancer† [off-label], the usual dosage administered in clinical studies is 1000 mg orally once daily.
Dosage Modification for Toxicity
Hepatic Toxicity
For ALT and/or AST elevations >5 times ULN or total bilirubin elevations >3 times ULN, interrupt dosing until liver function test results return to baseline or until ALT and AST return to ≤2.5 times ULN and total bilirubin returns to ≤1.5 times ULN, and then resume at a reduced dosage of 750 mg once daily (conventional abiraterone) or 375 mg once daily (micronized abiraterone).
If hepatic toxicity recurs on dosage of 750 mg once daily (conventional abiraterone) or 375 mg once daily (micronized abiraterone), interrupt dosing until liver function test results return to baseline or until ALT and AST return to ≤2.5 times ULN and total bilirubin returns to ≤1.5 times ULN, and then resume at a reduced dosage of 500 mg once daily (conventional abiraterone) or 250 mg once daily (micronized abiraterone).
If hepatic toxicity recurs on dosage of 500 mg once daily (conventional abiraterone) or 250 mg once daily (micronized abiraterone), discontinue abiraterone.
In patients reinitiating therapy, measure serum aminotransferases and bilirubin at least every 2 weeks for 3 months and then monthly thereafter.
For ALT elevations >3 times ULN with total bilirubin elevations >2 times ULN in the absence of biliary obstruction or other causes, permanently discontinue abiraterone.
Special Populations
Hepatic Impairment
Mild preexisting hepatic impairment (Child-Pugh class A): No dosage adjustment required.
Moderate preexisting hepatic impairment (Child-Pugh class B): 250 mg once daily (conventional abiraterone) or 125 mg once daily (micronized abiraterone). Monitor serum aminotransferases and bilirubin at baseline, every week for the first month of therapy, every 2 weeks during the second and third months, and then monthly thereafter. If elevations in ALT and/or AST to >5 times ULN or in total bilirubin to >3 times ULN occur, permanently discontinue abiraterone.
Severe preexisting hepatic impairment (Child-Pugh class C): Use not recommended.
Renal Impairment
No dosage adjustment required.
Geriatric Patients
No specific dosage recommendations.
Cautions for Abiraterone Acetate
Contraindications
-
No known contraindications.
Warnings/Precautions
Excessive Mineralocorticoid Activity
Mineralocorticoid excess occurs secondary to CYP17 blockade by abiraterone; commonly manifested as hypertension, hypokalemia, and fluid retention. Concomitant glucocorticoid administration may reduce severity and incidence of these adverse effects.
Monitor at least monthly for hypertension, hypokalemia, and fluid retention. Control BP and correct hypokalemia before and during treatment.
Closely monitor patients with a history of cardiovascular disease or underlying medical condition that might be compromised by increased BP, hypokalemia, or fluid retention (e.g., heart failure, recent MI, ventricular arrhythmia).
Safety not established in patients with left ventricular ejection fraction <50% or NYHA class II–IV heart failure.
Adrenocortical Insufficiency
Adrenocortical insufficiency reported following interruption of daily corticosteroid regimen and/or during periods of infection or stress.
Use with caution and monitor for manifestations of adrenocortical insufficiency, especially following corticosteroid dosage reduction or discontinuance or when patient is subjected to unusual stress. Consider possible need for increased corticosteroid dosage before, during, and after stressful situations.
Symptoms of mineralocorticoid excess may mask manifestations of adrenocortical insufficiency; perform appropriate tests to confirm diagnosis of adrenocortical insufficiency if clinically indicated.
Hepatic Toxicity
ALT or AST elevations of >5 times ULN reported in 6% of patients, generally during the initial 3 months of therapy. No fatalities reported in the principal efficacy studies. Fulminant hepatitis, acute liver failure, and death reported in postmarketing experience.
Elevations in liver function test results reported more frequently in patients with preexisting ALT or AST elevations than in patients with normal baseline values.
Monitor serum aminotransferase and bilirubin concentrations at baseline, every 2 weeks for the first 3 months of therapy, and then monthly thereafter. In patients with moderate preexisting hepatic impairment, monitor serum aminotransferase and bilirubin concentrations at baseline, every week for the first month of therapy, every 2 weeks during the second and third months, and then monthly thereafter.
More frequent monitoring is indicated if aminotransferase or bilirubin concentrations rise above pretreatment levels. Evaluate liver function tests promptly if manifestations suggestive of hepatotoxicity develop.
Treatment-related Mortality and Fractures
Increased mortality and fractures reported in patients with asymptomatic or mildly symptomatic castration-resistant prostate cancer metastatic to bone receiving abiraterone in combination with prednisone (or prednisolone) and radium Ra 223 dichloride; abiraterone is not currently FDA-labeled for use in combination with a corticosteroid and radium Ra 223 dichloride.
In a clinical trial, fractures (28.6 versus 11.4%) and death (38.5 versus 35.5%) occurred more frequently in patients receiving abiraterone in combination with prednisone (or prednisolone) and radium Ra 223 dichloride compared with those receiving abiraterone in combination with prednisone (or prednisolone). Treatment groups were unblinded based on recommendations of an independent data monitoring board.
Patients should not receive conventional abiraterone in combination with prednisone (or prednisolone) and radium Ra 223 dichloride or micronized abiraterone in combination with methylprednisolone and radium Ra 223 dichloride outside of a clinical trial.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm and potential loss of pregnancy. Safety and efficacy not established in females. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard and potential risk for loss of pregnancy.
Females who are or may be pregnant should not handle abiraterone acetate tablets without protection (e.g., gloves).
Males with female partners of reproductive potential should use effective methods of contraception during therapy and for 3 weeks following discontinuance of the drug.
Infertility
Based on animal studies, abiraterone may impair male fertility.
Hypoglycemia
May cause severe hypoglycemia in patients with preexisting diabetes mellitus receiving repaglinide or thiazolidinedione-containing medications (e.g., pioglitazone).
Monitor blood glucose concentrations in patients with diabetes mellitus during and after discontinuance of abiraterone therapy. Adjust antihyperglycemic drug therapy as indicated to decrease risk of hypoglycemia.
Specific Populations
Pregnancy
May cause fetal harm and potential loss of pregnancy.
Lactation
Not known whether distributed into milk, affects milk production, or affects breast-fed infants; safety and efficacy not established in females.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
No overall differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.
Hepatic Impairment
Systemic exposure may be increased and clearance may be decreased.
Dosage adjustment and careful monitoring of hepatic function required in patients with moderate hepatic impairment (Child-Pugh class B).
Not recommended in patients with severe hepatic impairment (Child-Pugh class C).
Renal Impairment
Pharmacokinetics not altered by end-stage renal disease requiring hemodialysis. No dosage adjustment necessary.
Common Adverse Effects
Conventional abiraterone in combination with prednisone (twice daily) in patients with metastatic castration-resistant prostate cancer (≥10%): Fatigue, joint swelling or discomfort, edema, muscle discomfort, constipation, diarrhea, hot flush, hypertension, cough, insomnia, contusion, upper respiratory tract infection, urinary tract infection, dyspnea, dyspepsia, nasopharyngitis, hematuria.
Laboratory abnormalities reported in ≥20% of patients receiving abiraterone acetate (conventional) in combination with prednisone (twice daily) and at an incidence ≥2% higher than that reported with placebo in patients with metastatic castration-resistant prostate cancer: Hypertriglyceridemia, hyperglycemia, elevated concentrations of aminotransferases (i.e., ALT, AST), lymphopenia, hypernatremia, hypokalemia, hypophosphatemia.
Adverse effects reported in men with metastatic castration-resistant prostate cancer who received micronized abiraterone acetate were generally similar to adverse effects reported in those who received conventional abiraterone acetate.
Conventional abiraterone in combination with prednisone (once daily) in patients with high-risk metastatic castration-sensitive prostate cancer (≥10%): Hypertension, hypokalemia, lymphopenia, elevated ALT and/or AST concentrations, hot flush.
Drug Interactions
Abiraterone is a potential inhibitor of CYP isoenzymes 1A2, 2D6, and 2C8 and, to a lesser extent, CYP isoenzymes 2C9, 2C19, and 3A4/5. Abiraterone is a substrate of CYP3A4 in vitro.
Neither abiraterone acetate nor abiraterone is a substrate of P-glycoprotein (P-gp) in vitro at clinically relevant concentrations; abiraterone acetate inhibits P-gp.
In vitro, abiraterone and its major metabolites are inhibitors of organic anion transport protein (OATP) 1B1.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP3A4 inhibitors: No clinically meaningful effect on systemic exposure of abiraterone.
Potent CYP3A4 inducers: Possible decreased serum concentrations of abiraterone. Avoid concomitant use; if concomitant use cannot be avoided, increase dosing frequency of abiraterone from once daily to twice daily (e.g., from 1 g once daily to 1 g twice daily [conventional tablets]; from 500 mg once daily to 500 mg twice daily [micronized tablets]). If potent CYP3A4 inducer is discontinued, resume prior dose and frequency of abiraterone.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP2D6: Possible increased serum concentrations of CYP2D6 substrate drug and possible toxicity. Avoid concomitant use of abiraterone and CYP2D6 substrates with a narrow therapeutic index. If concomitant use cannot be avoided, consider dosage reduction of the CYP2D6 substrate drug and use with caution.
Substrates of CYP2C8: Possible increased serum concentrations of CYP2C8 substrate drug and possible toxicity. If concomitant use of abiraterone and CYP2C8 substrates with a narrow therapeutic index is necessary, closely monitor for signs of toxicity of the CYP2C8 substrate drug.
Substrates of CYP1A2: Pharmacokinetic interaction not observed to date.
Specific Drugs
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Antimycobacterials, rifamycins (e.g., rifabutin, rifampin, rifapentine) |
Possible decreased abiraterone concentrations Rifampin: Decreased mean systemic exposure of abiraterone by 55% |
Avoid concomitant use If concomitant use cannot be avoided, increase dosing frequency of abiraterone from once daily to twice daily (e.g., from 1 g once daily to 1 g twice daily [conventional tablets]; from 500 mg once daily to 500 mg twice daily [micronized tablets]); resume prior dose and frequency when potent CYP3A4 inducer is discontinued |
|
Carbamazepine |
Possible decreased abiraterone concentrations |
Avoid concomitant use If concomitant use cannot be avoided, increase dosing frequency of abiraterone from once daily to twice daily (e.g., from 1 g once daily to 1 g twice daily [conventional tablets]; from 500 mg once daily to 500 mg twice daily [micronized tablets]); resume prior dose and frequency when potent CYP3A4 inducer is discontinued |
|
Dextromethorphan |
Increased peak concentrations and AUC of dextromethorphan |
|
|
Ketoconazole |
No clinically meaningful effect on systemic exposure of abiraterone |
|
|
Phenobarbital |
Possible decreased abiraterone concentrations |
Avoid concomitant use If concomitant use cannot be avoided, increase dosing frequency of abiraterone from once daily to twice daily (e.g., from 1 g once daily to 1 g twice daily [conventional tablets]; from 500 mg once daily to 500 mg twice daily [micronized tablets]); resume prior dose and frequency when potent CYP3A4 inducer is discontinued |
|
Phenytoin |
Possible decreased abiraterone concentrations |
Avoid concomitant use If concomitant use cannot be avoided, increase dosing frequency of abiraterone from once daily to twice daily (e.g., from 1 g once daily to 1 g twice daily [conventional tablets]; from 500 mg once daily to 500 mg twice daily [micronized tablets]); resume prior dose and frequency when potent CYP3A4 inducer is discontinued |
|
Repaglinide |
Increased systemic exposure to repaglinide; severe hypoglycemia reported |
If concomitant use with CYP2C8 substrates with a narrow therapeutic index is necessary, closely monitor for toxicity of the CYP2C8 substrate drug |
|
Thiazolidinedione-containing medications (e.g., pioglitazone) |
Increased systemic exposure to pioglitazone, a CYP2C8 substrate, by 46% Severe hypoglycemia reported |
If concomitant use with CYP2C8 substrates with a narrow therapeutic index is necessary, closely monitor for toxicity of the CYP2C8 substrate drug |
|
Theophylline |
No change in systemic exposure of single-dose theophylline |
|
|
Thioridazine |
Possible increased thioridazine concentrations |
Avoid concomitant use; if concomitant use cannot be avoided, consider thioridazine dosage reduction and use with caution |
Abiraterone Acetate Pharmacokinetics
Absorption
Bioavailability
Systemic exposure is dose proportional over a dose range of 250 mg to 1 g (conventional abiraterone) and 125 mg to 625 mg (micronized abiraterone); however, systemic exposure does not substantially increase when dose is doubled from 1 g to 2 g (conventional abiraterone).
Abiraterone acetate is a prodrug that is converted in vivo to abiraterone; peak plasma abiraterone concentrations are attained about 2 hours after abiraterone acetate dose.
Food
Food increases systemic exposure.
Oral administration of a single 1-g dose of abiraterone acetate (conventional) with a low-fat or high-fat meal increases abiraterone AUC by approximately fivefold or tenfold, respectively, and increases peak plasma concentrations by approximately sevenfold or 17-fold, respectively.
When a single dose of abiraterone acetate (conventional) is administered 2 hours after or 1 hour before a medium-fat meal, abiraterone AUC increases by approximately sevenfold or 1.6-fold, respectively.
Systemic exposure is similar following administration of abiraterone acetate (conventional) for 7 days with a low-fat meal or ≥2 hours after or 1 hour before a meal, but increases approximately twofold when administered with a high-fat meal.
Oral administration of a single 500-mg dose of abiraterone acetate (micronized) with a high-fat meal increases abiraterone AUC and peak plasma concentrations by approximately 4.4-fold and 6.5-fold, respectively.
Special Populations
In patients with mild (Child-Pugh class A) or moderate (Child-Pugh class B) hepatic impairment, AUC is increased 1.1- or 3.6-fold, respectively, compared with individuals with normal hepatic function.
In patients with severe hepatic impairment (Child-Pugh class C), AUC is increased approximately sevenfold and free fraction of the drug is increased twofold compared with individuals with normal hepatic function.
Distribution
Plasma Protein Binding
>99% (mainly albumin and α1-acid glycoprotein).
Special Populations
In patients with severe hepatic impairment (Child-Pugh class C), plasma protein binding of drug is decreased.
Elimination
Metabolism
Abiraterone acetate is hydrolyzed to abiraterone (active metabolite), most likely by esterases in non-CYP-dependent pathways. Further metabolized to 2 inactive sulfate conjugates, abiraterone sulfate (formed by SULT2A1, a sulfotransferase that catalyzes sulfate conjugation of dehydroepiandrosterone [DHEA] and other steroids) and N-oxide abiraterone sulfate (formed by CYP3A4 and SULT2A1).
Elimination Route
Excreted in feces (88%), mainly as abiraterone acetate (55%) and abiraterone (22%), and in urine (5%).
Half-life
Approximately 12 hours.
Special Populations
Mean half-life in patients with mild or moderate hepatic impairment is approximately 18 hours or 19 hours, respectively.
In patients with end-stage renal disease requiring hemodialysis, pharmacokinetic parameters were similar to those in individuals with normal renal function.
Stability
Storage
Oral
Tablets (conventional)
20–25°C (excursions permitted to 15–30°C).
Tablets (micronized)
20–25°C (excursions permitted to 15–30°C).
Actions
-
Abiraterone acetate is a prodrug of abiraterone, a potent, selective, and irreversible inhibitor of 17α-hydroxylase/C17,20-lyase (CYP17), an enzyme expressed in adrenal glands, testes, and prostate tumor. CYP17 inhibition results in suppression of androgen production.
-
17α-Hydroxylase catalyzes conversion of pregnenolone and progesterone to their 17α-hydroxy derivatives; C17,20-lyase catalyzes conversion of these 17α-hydroxy derivatives to DHEA and androstenedione, respectively. DHEA and androstenedione are androgenic precursors of testosterone.
-
Abiraterone is tenfold to 30-fold more potent than ketoconazole (a nonspecific CYP inhibitor and weak inhibitor of CYP17) in its inhibition of CYP17.
-
CYP17 inhibition can result in increased mineralocorticoid synthesis.
Advice to Patients
-
Inform patients that abiraterone acetate is available in different tablet formulations that are not interchangeable.
-
Importance of taking the corticosteroid as directed to minimize adverse effects of abiraterone. If a dose of abiraterone or the corticosteroid is missed, take the next dose at the regularly scheduled time; importance of advising clinician if more than one daily dose of abiraterone is missed.
-
For patients currently receiving gonadotropin-releasing hormone (GnRH) agonist therapy, importance of continuing this therapy during abiraterone therapy.
-
Risk of increased abiraterone exposure and adverse effects if the conventional formulation is taken with food. Advise patients to consume no food for at least 2 hours before or 1 hour after a dose of the conventional formulation.
-
Advise patients to swallow abiraterone acetate conventional or micronized tablets whole with water; do not crush or chew the tablets.
-
Risk of peripheral edema, hypertension, and hypokalemia (with potential to cause QT-interval prolongation or torsades de pointes). Importance of patients informing their clinician if dizziness, palpitations, tachycardia, feelings of faintness or lightheadedness, headache, confusion, leg pain, muscle weakness, or peripheral edema occurs.
-
Risk of adrenocortical insufficiency. Importance of patients informing their clinician if symptoms of adrenocortical insufficiency occur.
-
Risk of severe hepatotoxicity and importance of liver function test monitoring. Importance of patients immediately informing their clinician if jaundice, dark urine, or severe nausea or vomiting occurs.
-
Increased risk of treatment-related mortality and fractures in patients receiving abiraterone acetate in combination with a corticosteroids and radium Ra 223 dichloride. Use of abiraterone acetate in combination with a corticosteroid and radium Ra 223 dichloride is not recommended outside of a clinical trial.
-
Risk of severe hypoglycemia in patients with diabetes mellitus receiving concomitant abiraterone acetate and repaglinide or thiazolidinedione-containing medications. Importance of monitoring blood glucose concentrations and adjusting antihyperglycemic agents as necessary.
-
Advise patients that abiraterone may cause fetal harm and potential loss of pregnancy; it is not known whether the drug distributes into semen. Advise men to use an effective contraceptive method during sexual encounters with women of reproductive potential; these contraceptive measures are required during and for 3 weeks after discontinuance of abiraterone therapy. Advise patients that women who are or may become pregnant should not handle abiraterone acetate tablets without protection (e.g., gloves).
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
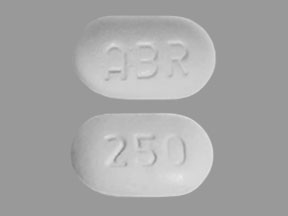
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
250 mg* |
Zytiga |
Janssen Biotech |
|
Abiraterone Acetate Tablets |
||||
|
Tablets, film-coated |
500 mg* |
Zytiga |
Janssen Biotech |
|
|
Abiraterone Acetate Film-coated Tablets |
||||
|
Tablets (micronized) |
125 mg |
Yonsa |
Sun Pharmaceutical Industries |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about abiraterone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (44)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- En español