PAZOPanib (Monograph)
Brand name: Votrient
Drug class: Antineoplastic Agents
- Kinase Inhibitors
- Receptor Tyrosine Kinase Inhibitors
- Tyrosine Kinase Inhibitors
VA class: AN900
Chemical name: 5-[[4-[(2,3-dimethyl-2H-indazol-6-yl)methylamino]-2-pyrimidinyl]amino]-2-methyl-benzenesulfonamide monohydrochloride
Molecular formula: C21H23N7O2S
CAS number: 635702-64-6
Introduction
Antineoplastic agent; an inhibitor of multiple receptor tyrosine kinases.
Uses for PAZOPanib
Renal Cell Carcinoma
Treatment of advanced renal cell carcinoma.
Guidelines generally recommend pazopanib as a first-line treatment option in patients with clear-cell metastatic renal cell carcinoma who cannot receive or tolerate immune-checkpoint inhibitors.
Soft Tissue Sarcoma
Treatment of advanced soft tissue sarcoma in adults who have received prior chemotherapy (designated an orphan drug by FDA for use in this condition).
Guidelines state that pazopanib is an option for the second or further line of treatment in non-adipogenic soft tissue sarcoma.
PAZOPanib Dosage and Administration
General
Pretreatment Screening
-
Blood pressure should be adequately controlled prior to initiating therapy. Do not initiate in patients with uncontrolled hypertension.
-
Assess ECG and electrolytes at baseline.
-
In patients at risk of cardiac dysfunction (including those previously treated with an anthracycline), assess left ventricular ejection fraction (LVEF) at baseline.
-
Perform thyroid function tests at baseline.
-
Perform urinalysis at baseline.
-
Verify pregnancy status of females of reproductive potential prior to initiation of therapy.
Patient Monitoring
-
Monitor liver function tests at weeks 3, 5, 7, and 9, and months 3 and 4, and then periodically thereafter as clinically indicated. Increase frequency of monitoring in patients who develop hepatotoxicity.
-
Monitor ECG and electrolytes as clinically indicated; correct hypokalemia, hypomagnesemia, and hypocalcemia as needed.
-
Monitor for signs and symptoms of congestive heart failure (CHF); in patients at risk of cardiac dysfunction (including those previously treated with an anthracycline), monitor LVEF periodically during therapy.
-
Monitor for signs and symptoms of venous thromboembolism (VTE), pulmonary embolism (PE), arterial thromboembolism, thrombotic microangiopathy, GI perforation/fistula, or interstitial lung disease/pneumonitis.
-
Monitor blood pressure as clinically indicated.
-
Monitor thyroid function during therapy as clinically indicated.
-
Perform urinalysis periodically during therapy; assess urine protein levels over a 24-hour period as clinically indicated.
-
Monitor for signs and symptoms of infection.
Dispensing and Administration Precautions
-
To avoid medication errors, the Institute for Safe Medication Practices (ISMP) recommends that prescribers communicate both the brand and generic names for pazopanib on the prescription order form.
Other General Considerations
-
Withhold pazopanib ≥7 days prior to scheduled surgery, and for ≥2 weeks following major surgery and until adequate wound healing has occurred.
Administration
Oral Administration
Administer orally without food (i.e., ≥1 hour before or 2 hours after a meal).
Swallow tablets whole and do not crush; crushing tablets increases rate of absorption and systemic exposure.
Concomitant use of pazopanib with drugs affecting gastric pH may result in decreased pazopanib exposure and should be avoided. If concomitant use with a drug affecting gastric pH cannot be avoided, consider a short-acting antacid rather than a proton-pump inhibitor or histamine H2-receptor antagonist; separate administration of a short-acting antacid and pazopanib by several hours.
Dosage
Available as pazopanib hydrochloride; dosage expressed in terms of pazopanib.
Adults
Renal Cell Carcinoma
Oral
800 mg once daily. Continue therapy for as long as the patient derives clinical benefit from the drug or until unacceptable toxicity occurs.
Soft Tissue Sarcoma
Oral
800 mg once daily. Continue therapy for as long as the patient derives clinical benefit from the drug or until unacceptable toxicity occurs.
Dosage Modification
Oral
If adverse reactions occur, temporary interruption of therapy, dosage reduction, and/or discontinuance of pazopanib may be necessary. If dosage modification is required, reduce the dosage of pazopanib as described in Table 1.
|
Dosage Reduction |
Renal Cell Carcinoma (Starting dosage = 800 mg once daily) |
Soft Tissue Sarcoma (Starting dosage = 800 mg once daily) |
|---|---|---|
|
First |
400 mg once daily |
600 mg once daily |
|
Second |
200 mg once daily |
400 mg once daily |
|
Third |
Permanently discontinue drug |
Permanently discontinue drug |
Hepatotoxicity
OralIf hepatotoxicity occurs, reduce pazopanib dosage, or interrupt or permanently discontinue therapy. (See Table 2.)
|
ALT and/or Bilirubin Concentrations |
Recommended Action |
|---|---|
|
Serum ALT concentration 3–8 times ULN |
Continue pazopanib; monitor liver function weekly until serum ALT concentration returns to grade 1 or baseline |
|
Serum ALT concentration >8 times ULN |
Interrupt therapy until serum ALT concentration returns to grade 1 or baseline; if benefit outweighs risk, reinitiate pazopanib at a reduced dosage of ≤400 mg once daily; following reinitiation, monitor liver function weekly for 8 weeks; if serum ALT concentration rises to >3 times ULN, discontinue pazopanib permanently |
|
Serum ALT concentration >3 times ULN and mild, indirect (unconjugated) hyperbilirubinemia in patients with Gilbert syndrome |
Manage per recommendations for patients with isolated ALT elevations |
|
Serum ALT concentration >3 times ULN and serum bilirubin concentration >2 times ULN |
Discontinue pazopanib permanently; monitor liver function until hepatotoxicity resolves |
Cardiac Dysfunction
OralIf symptomatic or grade 3 left ventricular systolic dysfunction occurs, withhold pazopanib until toxicity improves to grade 2 or less; therapy may be resumed based on clinical judgment.
If grade 4 left ventricular systolic dysfunction occurs, permanently discontinue pazopanib.
Hemorrhage
OralIf a grade 2 hemorrhagic event occurs, withhold pazopanib until toxicity improves to grade 1 or less; therapy may then be resumed at a reduced dosage (see Table 1).
If a grade 3 or 4 hemorrhagic event occurs, permanently discontinue pazopanib.
Thromboembolic Events
OralIf a grade 3 venous thromboembolic event (VTE) occurs, withhold pazopanib; therapy may be resumed at the same dosage after at least 1 week of appropriate therapy for the thromboembolic event.
If an arterial thromboembolic event or grade 4 VTE occurs, permanently discontinue pazopanib.
Thrombotic Microangiopathy
OralIf thrombotic microangiopathy occurs, permanently discontinue pazopanib.
GI Toxicity
OralIf GI perforation occurs, permanently discontinue pazopanib.
If grade 2 or 3 GI fistula occurs, withhold pazopanib; therapy may be resumed based on clinical judgment.
If grade 4 GI fistula occurs, permanently discontinue pazopanib.
Interstitial Lung Disease/Pneumonitis
OralIf interstitial lung disease or pneumonitis of any grade occurs, permanently discontinue pazopanib.
Posterior Reversible Encephalopathy Syndrome
OralIf posterior reversible encephalopathy syndrome of any grade occurs, permanently discontinue pazopanib.
Hypertension
OralIf grade 2 or 3 hypertension occurs, reduce the dosage of pazopanib (see Table 1) and initiate or adjust antihypertensive therapy. If hypertension remains grade 3 despite reducing the dosage of pazopanib and optimizing antihypertensive therapy, permanently discontinue pazopanib.
If grade 4 hypertension or hypertensive crisis occurs, permanently discontinue pazopanib.
Proteinuria
OralIf urine protein levels 3 grams or greater per 24 hours occurs, withhold pazopanib until urine protein levels improve to grade 1 or less; therapy may then be resumed at a reduced dosage (see Table 1). If urine protein levels over a 24-hour period do not improve or urine protein levels 3 grams or greater per 24 hours recurs despite reducing the dosage of pazopanib, permanently discontinue drug.
If nephrotic syndrome is confirmed, permanently discontinue pazopanib.
Concomitant Use with Drugs Affecting Hepatic Microsomal Enzymes
OralConcomitant use with potent inhibitors or inducers of CYP3A4 may alter plasma concentrations of pazopanib.
If concomitant use with a potent CYP3A4 inhibitor cannot be avoided, reduce pazopanib dosage to 400 mg once daily.
Avoid concomitant use with a potent CYP3A4 inducer.
Prescribing Limits
Adults
Renal Cell Carcinoma
Oral
Dosage <200 mg daily not recommended.
Soft Tissue Sarcoma
Oral
Dosage <400 mg daily not recommended.
Special Populations
Hepatic Impairment
Mild hepatic impairment (total bilirubin concentration not exceeding the ULN with ALT exceeding the ULN, or total serum bilirubin concentration ≤1.5 times the ULN with any level of ALT): No dosage adjustment required.
Moderate hepatic impairment (total bilirubin concentration >1.5 times but ≤3 times ULN and any concentration of ALT): Consider alternative therapy; however, if pazopanib is used, reduce dosage to 200 mg once daily.
Severe hepatic impairment (total bilirubin concentration >3 times ULN and any concentration of ALT): Avoid use.
Renal Impairment
Dosage adjustment not required.
Geriatric Patients
No specific dosage recommendations.
Related/similar drugs
Keytruda, Avastin, pembrolizumab, bevacizumab, nivolumab, doxorubicin, Adriamycin
Cautions for PAZOPanib
Contraindications
-
No known contraindications.
Warnings/Precautions
Warnings
Hepatic Effects
Severe or fatal hepatotoxicity, manifested as increases in concentrations of aminotransferases (ALT, AST) and bilirubin, reported. Most (92%) cases of aminotransferase elevations (of any grade) occurred during first 18 weeks of therapy.
Because pazopanib inhibits UGT1A1 (an enzyme that catalyzes the glucuronidation of bilirubin for elimination), mild elevations in indirect (unconjugated) bilirubin may occur in patients with deficient glucuronidation of bilirubin (i.e., Gilbert syndrome).
Concomitant use of pazopanib and simvastatin increases the risk of ALT elevations. If ALT elevations occur in a patient taking concomitant simvastatin, perform weekly liver function monitoring. Withhold pazopanib and resume at a reduced dosage, or permanently discontinue drug based on the severity of hepatotoxicity. Data are insufficient to assess risk of alternative statins administered concomitantly with pazopanib.
Perform liver function tests prior to initiation of therapy, during weeks 3, 5, 7, and 9 of therapy, at months 3 and 4, then periodically thereafter as clinically indicated.
If hepatotoxicity occurs, interrupt therapy, reduce dosage, or discontinue pazopanib permanently.
Other Warnings and Precautions
QT Interval Prolongation and Torsades de Pointes
Prolongation of QT interval and torsades de pointes reported.
Avoid concomitant administration of pazopanib and drugs that prolong the QT interval.
Monitor patients at significant risk for QT prolongation, (i.e., history of QT interval prolongation, concomitant use with antiarrhythmic agents or other drugs that cause prolongation of the QT interval, preexisting cardiac disease).
Monitor ECG and serum electrolytes (e.g., calcium, magnesium, potassium) prior to initiation of pazopanib and periodically during treatment. Correct hypokalemia, hypomagnesemia, and hypocalcemia prior to initiation of pazopanib and as necessary during therapy.
Cardiac Dysfunction
Cardiac dysfunction, including decreased LVEF and congestive heart failure, reported.
Monitor patients receiving pazopanib for signs and symptoms of congestive heart failure. Monitor LVEF in patients at risk of cardiac dysfunction (including those previously treated with an anthracycline) at baseline and periodically during therapy.
If cardiac dysfunction occurs, withhold or permanently discontinue pazopanib depending on the severity of the cardiac dysfunction.
Hemorrhage
Hemorrhage, sometimes severe or fatal, reported. Most common hemorrhagic events reported include hematuria, epistaxis, hemoptysis, oral, and anal/rectal hemorrhage; severe hemorrhagic events reported include pulmonary, peritoneal, GI, GU, and intracranial/subarachnoid hemorrhage.
Not evaluated in patients with history of hemoptysis or patients with cerebral or GI hemorrhage within the past 6 months.
If a hemorrhagic event occurs, withhold pazopanib and resume therapy at a reduced dosage or permanently discontinue pazopanib depending on the severity of the hemorrhagic event.
Thromboembolic Events
Arterial thromboembolic events (e.g., myocardial infarction/ischemia, cerebrovascular accident, TIA), sometimes severe or fatal, reported.
VTE, including venous thrombosis and fatal pulmonary embolism, reported.
Not evaluated in patients with history of an arterial thromboembolic event within the past 6 months.
Monitor for signs and symptoms of venous thromboembolism and pulmonary embolism during pazopanib therapy.
If venous thromboembolism or pulmonary embolism occurs, withhold pazopanib and resume at the same dosage or permanently discontinue depending on the severity of the thromboembolic event. If arterial thromboembolism occurs, permanently discontinue pazopanib.
Thrombotic Microangiopathy
Thrombotic microangiopathy, including thrombotic thrombocytopenic purpura and hemolytic uremic syndrome, reported in patients receiving pazopanib monotherapy or in combination with bevacizumab or topotecan. Pazopanib is not indicated for use in combination with other agents. Most thrombotic microangiopathy cases occurred within 90 days of pazopanib initiation, and all cases improved following pazopanib discontinuation.
Monitor patients receiving pazopanib for signs and symptoms of thrombotic microangiopathy.
If thrombotic microangiopathy occurs, permanently discontinue pazopanib.
GI Effects
GI perforation or fistula, sometimes fatal, reported.
Monitor for manifestations of GI perforation or fistula formation during therapy.
If GI fistula occurs, withhold pazopanib and resume based on clinical judgment or permanently discontinue pazopanib, depending on the severity of the fistula.
If GI perforation occurs, permanently discontinue pazopanib.
Interstitial Lung Disease/Pneumonitis
Interstitial lung disease/pneumonitis, which can be fatal, reported.
Monitor for pulmonary symptoms indicative of interstitial lung disease/pneumonitis.
If interstitial lung disease or pneumonitis occurs, permanently discontinue pazopanib.
Posterior Reversible Encephalopathy Syndrome
Posterior reversible encephalopathy syndrome, which can be fatal, reported. Symptoms of posterior reversible encephalopathy syndrome may include headache, seizure, lethargy, confusion, blindness, and other visual and neurologic disturbances. Mild to severe hypertension may also be present.
If symptoms of posterior reversible encephalopathy syndrome occur, confirm diagnosis with MRI.
If posterior reversible encephalopathy syndrome occurs, permanently discontinue pazopanib.
Hypertension
Hypertension (SBP ≥150 mm Hg or DBP ≥100 mm Hg) reported. Most (90%) cases occurred during first 18 weeks of therapy. Majority of cases were managed with antihypertensive therapy or by reduction in pazopanib dosage. Hypertensive crisis reported rarely.
Do not initiate pazopanib in patients with uncontrolled hypertension. Blood pressure should be adequately controlled prior to initiation of pazopanib.
Monitor BP and treat hypertension with standard antihypertensive therapy as needed. If hypertension persists despite use of antihypertensive therapy, reduce pazopanib dosage, or permanently discontinue drug depending on severity of hypertension.
Wound-healing Complications
Inhibitors of vascular endothelial growth factor (VEGF), including pazopanib, may impair wound healing; discontinue pazopanib ≥7 days prior to scheduled surgery. Withhold for ≥2 weeks following major surgery and until adequate wound healing has occurred.
Safety of resuming pazopanib therapy after resolution of wound healing complications not established.
Hypothyroidism
Hypothyroidism reported.
Monitor thyroid function at baseline and during therapy as clinically indicated. Manage hypothyroidism as appropriate.
Proteinuria
Proteinuria reported.
Perform urinalysis prior to initiation of pazopanib and periodically during therapy, with follow-up measurement of 24-hour urine protein as clinically indicated.
If proteinuria occurs, withhold pazopanib and resume at a reduced dosage or permanently discontinue drug, depending on the severity of proteinuria.
If nephrotic syndrome occurs, permanently discontinue pazopanib.
Tumor Lysis Syndrome
Tumor lysis syndrome, sometimes fatal, reported.
Monitor patients at risk of tumor lysis syndrome (e.g., those with rapidly growing tumors, high tumor burden, renal dysfunction, or dehydration) closely during pazopanib therapy; consider prophylactic therapy, and initiate treatment for tumor lysis syndrome as clinically indicated.
Infection
Serious, sometimes fatal, infections (with or without neutropenia) reported.
Monitor for signs and symptoms of infection. If serious infections occur, consider interruption or discontinuation of pazopanib.
Combination Therapy
Pazopanib is not indicated for use in combination with other agents. Clinical trials of pazopanib in combination with pemetrexed or lapatinib were terminated early due to increased toxicity and mortality. Fatal toxicities included pulmonary hemorrhage, GI hemorrhage, and sudden death.
Increased Toxicity in Developing Organs
Pazopanib may cause serious adverse effects on organ development in pediatric patients, particularly in those <2 years of age as demonstrated in animal studies. Pazopanib is not indicated for use in pediatric patients, as safety and efficacy in this patient population have not been established.
Based on its mechanism of action, pazopanib may have severe effects on organ growth and maturation during early postnatal development.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; maternal toxicity, teratogenicity, and abortifacient effects demonstrated in animals. Avoid pregnancy during therapy. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Advise females of reproductive potential to use effective contraception during pazopanib therapy and for ≥2 weeks after the final dose. Advise males with such female partners to use condoms during pazopanib therapy and for ≥2 weeks after the final dose.
Specific Populations
Pregnancy
Based on animal reproduction studies and its mechanism of action, pazopanib may cause fetal harm. There are no adequate and well-controlled studies in pregnant women.
Avoid pregnancy during therapy. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Lactation
Not known whether pazopanib or its metabolites are distributed into human milk. No data on effects of pazopanib or its metabolites on the breast-fed infant or milk production.
Because of the potential for serious adverse reactions to pazopanib in breast-fed infants, avoid breast-feeding during pazopanib therapy and for 2 weeks after the final dose of the drug.
Females and Males of Reproductive Potential
Prior to initiation of pazopanib therapy, verify pregnancy status of females of reproductive potential.
Advise females of reproductive potential to use effective contraception during pazopanib treatment and for ≥2 weeks after the last dose of pazopanib. Advise males with such female partners to used condoms during pazopanib treatment and for ≥2 weeks after the last dose of pazopanib.
May impair fertility in females and males of reproductive potential.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
May cause serious adverse effects on organ development in pediatric patients, particularly those <2 years of age.
Geriatric Use
No substantial differences in efficacy relative to younger patients. Patients >65 years of age may be at greater risk of grade 3 or 4 fatigue, hypertension, decreased appetite, ALT elevations, and AST elevations.
Hepatic Impairment
Mild hepatic impairment (total bilirubin concentration not exceeding the ULN with ALT exceeding the ULN, or total serum bilirubin concentration ≤1.5 times the ULN with any level of ALT) did not impact pharmacokinetics; no dosage reduction necessary.
Maximum tolerated dosage in patients with moderate hepatic impairment (total serum bilirubin concentration >1.5 times but ≤3 times ULN and any concentration of ALT ) was 200 mg once daily. Use is not recommended in patients with moderate hepatic impairment; however, if pazopanib is used in such patients, reduce dosage of drug. and also
Use in patients with severe hepatic impairment (total serum bilirubin concentration >3 times ULN with any level of ALT) not recommended.
Renal Impairment
Renal impairment unlikely to affect pharmacokinetics (e.g., exposure) of pazopanib; no dosage adjustment necessary in patients with renal impairment.
Pharmacokinetic profile not established in patients with severe renal impairment (Clcr <30 mL/minute) or in patients undergoing peritoneal dialysis or hemodialysis.
Pharmacogenomics
Pazopanib inhibits UGT1A1, an enzyme that catalyzes the glucuronidation of bilirubin for elimination. Patients who are homozygous for the UGT1A1*28 allele (characterized by a mutation in the promoter region of the UGT1A1 gene) have reduced expression of UGT1A1, which may manifest as mild hyperbilirubinemia (i.e., Gilbert syndrome). Mild elevations of indirect (unconjugated) bilirubin concentrations may occur in patients with Gilbert syndrome receiving pazopanib.
In a pooled pharmacogenetic analysis of data from 31 clinical studies evaluating pazopanib, ALT elevations exceeding 3 times the upper limit of normal (ULN) occurred in 32% of patients who were HLA-B*57:01 allele carriers and in 19% of noncarriers. ALT elevations exceeding 5 times the ULN occurred in 19% of HLA-B*57:01 allele carriers and in 10% of noncarriers.
Common Adverse Effects
Adverse effects reported in ≥20% of patients receiving pazopanib for renal cell carcinoma: Diarrhea, hypertension, hair color changes (depigmentation), nausea, anorexia, vomiting.
Adverse effects reported in ≥20% of patients receiving pazopanib for soft tissue sarcoma: Fatigue, diarrhea, nausea, decreased weight, hypertension, decreased appetite, vomiting, tumor pain, hair color changes, musculoskeletal pain, headache, dysgeusia, dyspnea, skin hypopigmentation.
Drug Interactions
Metabolized principally by CYP3A4 and, to a lesser extent, by CYP isoenzymes 1A2 and 2C8.
Weak inhibitor of CYP isoenzymes 3A4, 2C8, and 2D6, but has no effect on CYP isoenzymes 1A2, 2C9 and 2C19.
May induce and/or inhibit CYP3A4, and inhibit CYP isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, and 2E1.
Inhibits glucuronidation by UGT1A1; also inhibits organic anion transport protein (OATP) 1B1.
Substrate of P-glycoprotein (P-gp) and breast cancer resistant protein (BCRP).
Drugs and Foods Affecting Hepatic Microsomal Enzymes
CYP3A4 inhibitors: Pharmacokinetic interaction (increased peak plasma concentrations and AUC of pazopanib). Avoid concomitant use with a potent CYP3A4 inhibitor; if concomitant therapy cannot be avoided, reduce pazopanib dosage.
CYP3A4 inducers: Potential pharmacokinetic interaction (decreased plasma concentration of pazopanib). Avoid concomitant use; consider selecting an alternative agent with minimal or no enzyme induction potential. If long-term use of a potent CYP3A4 inducer is required, do not initiate pazopanib therapy.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP isoenzymes 3A4, 2D6, or 2C8: Pharmacokinetic interaction (increased exposure to substrate). Avoid concomitant use with substrates of CYP isoenzymes 3A4, 2D6, or 2C8 that have a narrow therapeutic index.
Substrates of CYP isoenzymes 1A2, 2C9, or 2C19: No clinically relevant pharmacokinetic interaction.
Drugs Affecting Efflux Transport Systems
Inhibitors of P-gp or BCRP: Potential pharmacokinetic interaction (increased concentrations of pazopanib). Avoid concomitant use of pazopanib and potent inhibitors of P-gp or BCRP. Consider selection of alternative agents with no or minimal potential to inhibit P-gp or BCRP.
Drugs Transported by Organic Anion Transport Protein (OATP)
Potential pharmacokinetic interaction (increased plasma concentration of drugs transported by OATP1B1).
Drugs Metabolized by Uridine Diphosphate-glucuronosyltransferase (UGT)
Potential pharmacokinetic interaction (increased plasma concentration of drugs metabolized by UGT1A1).
Drugs Affecting Gastric Acidity
Pharmacokinetic interaction (decreased exposure to pazopanib). Avoid concomitant use of pazopanib and drugs affecting gastric acidity. If concomitant administration of a drug affecting gastric acidity cannot be avoided, consider short-acting antacids rather than proton-pump inhibitors or a histamine H2-receptor antagonist. Administration of a short-acting antacid and pazopanib should be separated by several hours.
Drugs that Prolong the QT Interval
Risk of prolonged QT interval and torsades de pointes. Avoid concomitant use of pazopanib and drugs that prolong the QT interval.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Caffeine |
No clinically relevant pharmacokinetic interaction |
|
|
Dextromethorphan |
Increased urine concentrations of dextromethorphan and dextrorphan |
|
|
Esomeprazole |
Decreased exposure to pazopanib |
Avoid concomitant use If acid suppressant therapy is required, consider short-acting antacids rather than a proton-pump inhibitor or histamine H2-receptor antagonist; separate administration of short-acting antacids and pazopanib by several hours |
|
Grapefruit or grapefruit juice |
Possible increased plasma pazopanib concentrations |
Avoid concomitant use |
|
Ketoconazole |
Increased peak plasma concentrations and AUC of pazopanib following concomitant use with pazopanib |
Avoid concomitant use If concomitant use cannot be avoided, reduce pazopanib dosage to 400 mg once daily; further dosage reductions may be required if adverse effects occur |
|
Lapatinib |
Increased peak plasma concentrations and AUC of pazopanib |
|
|
Midazolam |
Increased peak plasma concentrations and AUC of midazolam |
|
|
Omeprazole |
No clinically relevant pharmacokinetic interaction |
|
|
Paclitaxel |
Increased peak plasma concentrations and AUC of paclitaxel |
|
|
Simvastatin |
Increased incidence of ALT elevations in clinical trials Data insufficient to assess risk of using other statins with pazopanib |
If ALT elevation develops, monitor liver function weekly; depending on severity of hepatotoxicity, withhold pazopanib and resume at a reduced dosage or permanently discontinue pazopanib therapy |
|
Warfarin |
No clinically relevant pharmacokinetic interaction |
PAZOPanib Pharmacokinetics
Absorption
Bioavailability
Incompletely absorbed from GI tract, with reported bioavailabilities of 14–39%.
Following oral administration, peak plasma concentrations are attained within 2–4 hours.
Administration of a single 400-mg crushed tablet increased peak plasma concentrations by twofold and AUC by 46% and decreased time to peak plasma concentrations by approximately 2 hours.
Food
Food increases peak plasma concentrations and AUC by approximately twofold.
Distribution
Extent
Not known whether pazopanib or its metabolites are distributed into human milk.
Plasma Protein Binding
>99%.
Elimination
Metabolism
Metabolized in the liver, principally by CYP3A4 and, to a lesser extent, by CYP1A2 and CYP2C8. Metabolites account for <10% of administered dose.
Elimination Route
Excreted principally in feces (approximately 82%) and, to a lesser extent, in urine (<4%).
Hemodialysis not expected to enhance elimination because pazopanib is highly bound to plasma proteins and is not substantially excreted renally.
Half-life
Approximately 31 hours.
Special Populations
Clcr (within the range of 30–150 mL/minute) does not substantially affect pazopanib clearance.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Actions
-
Inhibits multiple receptor tyrosine kinases (RTKs), which are involved in the initiation of various cascades of intracellular signaling events that lead to cell proliferation and/or influence processes critical to cell survival and tumor progression (e.g., angiogenesis, metastasis, inhibition of apoptosis), based on the respective kinase.
-
Inhibits signal transduction pathways involving multiple receptor tyrosine kinases, principally vascular endothelial growth factor receptors (i.e., VEGFR-1, VEGFR-2, VEGFR-3), platelet-derived growth factors (PDGFR-α, PDGFR-β), and stem cell factor receptor (i.e., c-kit).
-
Has modest inhibitory effects on fibroblast growth factor receptors (i.e., FGFR1, FGFR3), transmembrane glycoprotein receptor tyrosine kinase (c-Fms), leukocyte-specific protein tyrosine kinase (Lck), and interleukin-2 receptor inducible T-cell kinase (Itk).
-
Shown to inhibit angiogenesis in a mouse model and the growth of some human tumor xenografts in mice.
-
Appears to be as potent as sorafenib and sunitinib against VEGFR (i.e., VEGFR-1, VEGFR-2, VEGFR-3) and less potent than sunitinib against fms-like tyrosine kinase 3 (Flt-3). Differences in potencies against non-VEGF receptors may account for variabilities in non-VEGFR-related (“off-target”) adverse effects observed with pazopanib (e.g., hepatotoxicity, lower incidence of palmar-plantar erythrodysesthesia [hand-foot syndrome] and rash compared with sorafenib or sunitinib [based on indirect cross-study comparison], lower incidence of and less severe myelosuppression compared with sunitinib [based on indirect cross-study comparison]).
-
Inhibits UGT1A1, an enzyme that catalyzes the glucuronidation of bilirubin for elimination. Patients who are homozygous for the UGT1A1*28 allele (characterized by a mutation in the promoter region of the UGT1A1 gene) have reduced expression of UGT1A1, which may manifest as mild hyperbilirubinemia (i.e., Gilbert's syndrome). Mild elevations of indirect (unconjugated) bilirubin concentrations may occur in patients with Gilbert's syndrome receiving pazopanib.
Advice to Patients
-
Pazopanib medication guide should be provided to patient each time the drug is dispensed; importance of patient reading the medication guide prior to initiating pazopanib therapy and each time the prescription is refilled.
-
Importance of taking pazopanib without food (i.e., ≥1 hour before or 2 hours after a meal). Importance of swallowing tablets whole and not crushing the tablets. Avoid grapefruit or grapefruit juice while taking the drug.
-
If a dose is missed by <12 hours, take it as soon as it is remembered, and take the next dose at the regularly scheduled time. Do not take more than one dose at a time.
-
Risk of adverse hepatic effects and importance of periodic laboratory testing. Importance of immediately reporting any manifestations of hepatotoxicity (e.g., jaundice, unusual fatigue, unusual darkening of urine, nausea, vomiting, loss of appetite, right-upper quadrant pain, easy bruising).
-
Risk of QT prolongation and torsades de pointes. Advise patients to report any concomitant medications. Inform patients that ECG monitoring may be performed.
-
Risk of interstitial lung disease/pneumonitis. Importance of reporting any manifestations of interstitial lung disease or pneumonitis (e.g., persistent cough, dyspnea).
-
Risk of adverse cardiovascular effects. Importance of monitoring BP regularly during therapy. Importance of immediately reporting irregular or fast heart beat, fainting, or manifestations of a heart attack or stroke (e.g., chest pain or pressure; pain in arms, back, neck, or jaw; shortness of breath; numbness or weakness on one side of body; trouble talking; headache; dizziness).
-
Risk of bleeding. Importance of promptly informing clinicians of any unusual bleeding, bruising, or wounds that do not heal.
-
Risk of adverse GI effects (e.g., diarrhea, nausea, vomiting, GI perforation). Importance of understanding measures to manage mild diarrhea and of notifying clinician if moderate or severe diarrhea occurs. Importance of immediately reporting any manifestations of GI perforation (e.g., abdominal pain or swelling, vomiting blood, black sticky stools).
-
Risk of thromboembolic events. Importance of reporting any manifestations of thromboembolic events.
-
Risk of posterior reversible encephalopathy syndrome. Importance of reporting any manifestations of posterior reversible encephalopathy syndrome (e.g., headache, seizure, lethargy, confusion, blindness).
-
Risk of GI perforation or fistula. Importance of reporting any manifestations of GI perforation or fistula.
-
Risk of impaired wound healing. Importance of informing clinician of any scheduled surgical procedures.
-
Risk of hypothyroidism and proteinuria. Importance of thyroid function tests and urinanalysis during therapy.
-
Risk of tumor lysis syndrome. Importance of informing clinician of any manifestations of tumor lysis syndrome occur (e.g., abnormal heart rhythm, seizure, confusion, muscle cramps/spasms, decreased urine output).
-
Risk of infection. Importance of informing clinician of any manifestations of infection.
-
Risk of depigmentation of hair and skin.
-
Risk of impaired male or female fertility.
-
Importance of females informing clinicians if they are or plan to become pregnant or plan to breast-feed. Apprise patient of potential hazard to the fetus if used during pregnancy; females of reproductive potential should avoid becoming pregnant. Advise females of reproductive potential to use effective contraception during treatment and for at least 2 weeks after the last dose of pazopanib. Advise males with such female partners to use condoms during treatment and for at least 2 weeks after the last dose of pazopanib.
-
Advise women to inform their clinicians if they are or plan to breast-feed. Avoid breast-feeding during pazopanib treatment and for at least 2 weeks after the last dose of pazopanib.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses (e.g., cardiovascular disease, hepatic impairment).
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
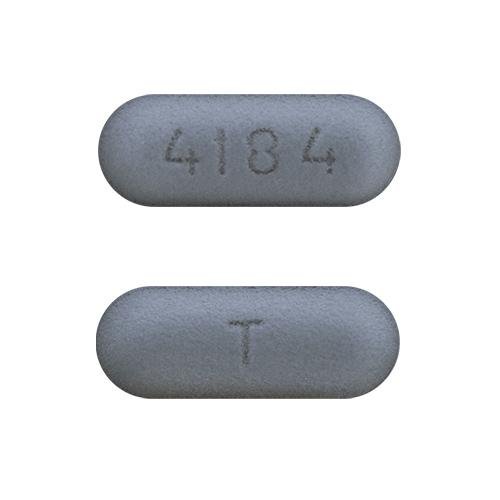
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
200 mg (of pazopanib) |
Votrient |
GlaxoSmithKline |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions March 30, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
- Does Votrient cure cancer or shrink tumors?
- How long does Votrient stay in your system?
- Is Votrient a chemotherapy treatment?
- Is Votrient immunotherapy?
More about pazopanib
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (92)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: VEGF/VEGFR inhibitors
- Breastfeeding
- En español