Venlafaxine (Monograph)
Brand names: Effexor, Effexor XR
Drug class: Selective Serotonin- and Norepinephrine-reuptake Inhibitors
- Serotonin-reuptake Inhibitors
- SNRI
VA class: CN609
Molecular formula: C17H27NO2•ClH
CAS number: 99300-78-4
Warning
- Suicidality
-
Antidepressants may increase risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (18–24 years of age) with major depressive disorder and other psychiatric disorders; balance this risk with clinical need. Venlafaxine is not approved for use in pediatric patients. (See Pediatric Use under Cautions.)
-
In pooled data analyses, risk of suicidality was not increased in adults >24 years of age and apparently was reduced in adults ≥65 years of age with antidepressant therapy compared with placebo.
-
Depression and certain other psychiatric disorders are themselves associated with an increased risk of suicide.
-
Appropriately monitor and closely observe all patients who are started on venlafaxine therapy for clinical worsening, suicidality, or unusual changes in behavior; involve family members and/or caregivers in this process. (See Risk of Suicidality and Overdosage under Cautions.)
Introduction
A selective serotonin- and norepinephrine-reuptake inhibitor (SNRI); antidepressant and anxiolytic agent.
Uses for Venlafaxine
Major Depressive Disorder
Management of major depressive disorder.
Efficacy of extended-release capsules in hospital settings not established.
Generalized Anxiety Disorder
Management of generalized anxiety disorder.
Social Phobia
Management of social phobia (social anxiety disorder).
Panic Disorder
Management of panic disorder with or without agoraphobia.
Obesity
Not indicated for the management of exogenous obesity† [off-label] (either alone or in combination with weight loss agents such as phentermine), although weight loss reported in some patients receiving the drug for other disorders.
Vasomotor Symptoms
Management of vasomotor symptoms† [off-label] in women with breast cancer and in postmenopausal women; improved both frequency and severity of vasomotor symptoms (hot flushes [flashes]).
Related/similar drugs
Vraylar, gabapentin, acetaminophen, sertraline, trazodone, tramadol, duloxetine
Venlafaxine Dosage and Administration
General
-
Allow at least 2 weeks to elapse between discontinuance of an MAO inhibitor and initiation of venlafaxine and at least 1 week to elapse between discontinuance of venlafaxine and initiation of an MAO inhibitor.
-
Monitor for possible worsening of depression, suicidality, or unusual changes in behavior, especially at the beginning of therapy or during periods of dosage adjustments. (See Risk of Suicidality and Overdosage under Cautions.)
-
Avoid abrupt discontinuance. To avoid withdrawal reactions, taper dosage gradually. (See Risk of Suicidality and Overdosage and also see Withdrawal of Therapy under Cautions.)
-
Consider cautiously tapering dosage during third trimester of pregnancy prior to delivery. (See Pregnancy under Cautions.)
-
Sustained therapy may be required; use lowest effective dosage and periodically reassess need for continued therapy.
Administration
Oral Administration
Administer orally with food.
Administer conventional tablets twice or 3 times daily with food.
Administer extended-release capsules as a single daily dose with food at approximately the same time each day (morning or evening). Swallow extended-release capsules whole with fluid; do not divide, crush, chew, or place in water.
Alternatively, open capsule(s) and sprinkle on a small amount of applesauce; swallow immediately without chewing. After administration, the patient should drink a glass of water to ensure that the pellets are completely swallowed.
Dosage
Available as venlafaxine hydrochloride; dosage expressed in terms of venlafaxine.
Adults
Major Depressive Disorder
Oral
Initially, 75 mg daily administered in 2 or 3 divided doses as conventional tablets or as a single daily dose when using the extended-release capsules. Alternatively, an initial dosage of 37.5 mg daily as extended-release capsules for the first 4–7 days (followed by an increase to 75 mg daily) may be considered for some patients. If no improvement, dosage may be increased by increments of up to 75 mg daily at intervals of not less than 4 days up to a maximum dosage of 375 mg daily (usually administered in 3 divided doses) as conventional tablets or 225 mg daily as extended-release capsules.
No additional benefit demonstrated from dosages >225 mg daily as conventional tablets in clinical studies in moderately depressed outpatients, but patients with more severe depression responded to higher dosages (mean dosage of 350 mg daily).
If desired, conventional tablets may be switched to the extended-release capsules at the nearest equivalent daily venlafaxine dosage (e.g., change 37.5 mg administered twice daily as conventional tablets to 75-mg extended-release capsule administered once daily). Individualize dosage adjustments as necessary.
Optimum duration not established; may require several months of therapy or longer. Antidepressant efficacy demonstrated for up to 6 months with venlafaxine extended-release capsules and for up to 1 year with conventional tablets.
Periodically reassess need for continued therapy and appropriateness of dosage.
Generalized Anxiety Disorder
Oral
Initially, 75 mg once daily as extended-release capsules. In some patients, it may be desirable to initiate therapy with a dosage of 37.5 mg daily given for the first 4–7 days, followed by an increase to 75 mg daily. If no improvement, dosage may be increased in increments of up to 75 mg daily (up to a maximum dosage of 225 mg daily as extended-release capsules) at intervals of not less than 4 days.
Optimum duration not established; efficacy demonstrated in a 6-month clinical trial. Periodically reassess need for continued therapy.
Social Phobia
Oral
Initially, 75 mg once daily as extended-release capsules. In some patients, it may be desirable to initiate therapy with a dosage of 37.5 mg daily given for the first 4–7 days, followed by an increase to 75 mg daily. If no improvement, dosage may be increased in increments of up to 75 mg daily (up to a maximum dosage of 225 mg daily as extended-release capsules) at intervals of not less than 4 days.
Optimum duration not established; long-term efficacy (>12 weeks) not demonstrated. Periodically reassess need for continued therapy.
Panic Disorder
Oral
Initially, 37.5 mg once daily as extended-release capsules for 7 days. If no improvement, dosage may be increased in increments of up to 75 mg daily at intervals of not less than 7 days. In clinical trials, 37.5 mg once daily was given initially for 7 days, then 75 mg once daily for 7 days; thereafter, dosage was increased in increments of 75 mg daily every 7 days if necessary. Certain patients not responding to 75 mg once daily may benefit from dosage increases up to a maximum of approximately 225 mg daily.
Optimum duration not established; longer-term efficacy (>12 weeks) in prolonging time to relapse in responding patients demonstrated in a controlled trial. Periodically reassess need for continued therapy.
Vasomotor Symptoms† [off-label]
Oral
Optimum dosage for vasomotor symptoms† [off-label] in women with breast cancer and in postmenopausal women not established. Initially, some clinicians recommend 37.5 mg once daily as extended-release capsules; may increase as necessary to 75 mg once daily. 75 mg once daily as extended-release capsules appeared optimal in one study. Further dosage increases may not provide additional benefit but are potentially more toxic.
Prescribing Limits
Adults
Major Depressive Disorder
Oral
Maximum 375 mg daily (generally in 3 equally divided doses) as conventional tablets or 225 mg daily as extended-release capsules.
Generalized Anxiety Disorder
Oral
Maximum 225 mg daily as extended-release capsules.
Social Phobia
Oral
Maximum 225 mg daily as extended-release capsules.
Panic Disorder
Oral
Maximum 225 mg daily as extended-release capsules.
Special Populations
Hepatic Impairment
Oral
Extended-release capsules: Reduce initial dosage by 50% in patients with moderate hepatic impairment.
Conventional tablets: Reduce total daily dosage by 50% in patients with moderate hepatic impairment.
In patients with cirrhosis, may be desirable to individualize dosages. May be necessary to reduce dosage of conventional tablets by >50%.
Renal Impairment
Oral
When using conventional tablets or extended-release capsules, reduce total daily dosage by 25–50% in patients with mild-to-moderate renal impairment and by 50% in those undergoing hemodialysis. Withhold dosages until the dialysis period is complete (4 hours).
Cautions for Venlafaxine
Contraindications
-
Concurrent or recent (i.e., within 2 weeks) therapy with an MAO inhibitor. (See MAO Inhibitors under Cautions and see Interactions.)
-
Known hypersensitivity to venlafaxine or any ingredient in the formulation.
Warnings/Precautions
Warnings
Risk of Suicidality and Overdosage
Possible worsening of depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior in both adult and pediatric patients with major depressive disorder, whether or not they are taking antidepressants; may persist until clinically important remission occurs. However, suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide.
Venlafaxine overdosage may be associated with an increased risk of fatal outcome compared with SSRI overdosage but lower than that associated with tricyclic antidepressants. In epidemiologic studies, venlafaxine-treated patients had a higher preexisting burden of suicide risk factors than SSRI-treated patients. The extent to which the finding of an increased risk of fatal outcomes can be attributed to the toxicity of venlafaxine overdosage as opposed to other characteristics of these venlafaxine-treated patients is not clear.
Prescribe in smallest quantity consistent with good patient management to reduce risk of overdosage.
Appropriately monitor and closely observe patients receiving venlafaxine for any reason, particularly during initiation of therapy (i.e., the first few months) and during periods of dosage adjustments. (See Boxed Warning and also see Pediatric Use under Cautions.)
Anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and/or mania may be precursors to emerging suicidality. Consider changing or discontinuing therapy in patients whose depression is persistently worse or in those with emerging suicidality or symptoms that might be precursors to worsening depression or suicidality, particularly if severe, abrupt in onset, or not part of patient’s presenting symptoms. If decision is made to discontinue drug therapy, taper venlafaxine dosage as rapidly as is feasible but consider risks of abrupt discontinuance. (See Withdrawal of Therapy under Cautions.)
Observe these precautions for patients being treated for psychiatric (e.g., major depressive disorder, obsessive-compulsive disorder) or nonpsychiatric disorders.
Bipolar Disorder
May unmask bipolar disorder. (See Activation of Mania or Hypomania under Cautions.) Venlafaxine is not approved for use in treating bipolar depression.
Screen for risk of bipolar disorder by obtaining detailed psychiatric history (e.g., family history of suicide, bipolar disorder, depression) prior to initiating therapy.
MAO Inhibitors
Concomitant use with MAO inhibitors associated with serious, sometimes fatal reactions, including manifestations resembling serotonin syndrome (e.g., hyperthermia, rigidity, myoclonus, autonomic instability, mental status changes) or neuroleptic malignant syndrome. (See General under Dosage and Administration and see Specific Drugs under Interactions.)
Serotonin Syndrome
Potentially life-threatening serotonin syndrome reported during concurrent therapy with SSRIs or SNRIs and other serotonergic drugs (e.g., 5-HT1 receptor agonists [“triptans”]) or drugs that impair serotonin metabolism (e.g., MAO inhibitors). Symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile BP, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination), and/or GI symptoms (e.g., nausea, vomiting, diarrhea). (See Interactions.)
Sustained Hypertension
Sustained, dose-dependent hypertension (i.e., treatment-emergent increases in supine DBP ≥90 mm Hg and ≥10 mm Hg above baseline for 3 consecutive visits) reported; potential adverse consequences. Elevated blood pressure requiring immediate treatment also reported.
Control preexisting hypertension before initiating therapy and regularly monitor BP during therapy. If sustained increases in BP occur, consider venlafaxine dosage reduction or discontinuance.
General Precautions
Withdrawal of Therapy
Possibly severe withdrawal reactions (e.g., agitation, anorexia, anxiety, confusion, impaired coordination, diarrhea, dizziness, dry mouth, dysphoric mood, fasciculation, fatigue, headaches, hypomania, insomnia, nausea, nervousness, nightmares, sensory disturbances, somnolence, sweating, tremor, vertigo, vomiting); avoid abrupt discontinuance. Taper dosage gradually; monitor carefully.
If intolerable symptoms occur following dosage reduction or discontinuance, reinstitute previously prescribed dosage until symptoms abate, then resume more gradual dosage reductions.
CNS Effects
Possible anxiety, nervousness, or insomnia.
Weight Loss
Weight loss reported in adults and pediatric patients. (See Obesity under Uses.)
Anorexia
Anorexia reported in adults and pediatric patients. (See Obesity under Uses.)
Activation of Mania or Hypomania
Possible activation of mania and hypomania; use with caution in patients with a history of mania. (See Bipolar Disorder under Cautions.)
Hyponatremia or SIADH
Possible hyponatremia or SIADH; use with caution in patients who are volume-depleted, elderly, or taking diuretics.
Mydriasis
Mydriasis reported. Monitor patients with elevated intraocular pressure (IOP) or at risk of angle-closure glaucoma.
Seizures
Use with caution in patients with a history of seizures. Discontinue therapy in any patient who develops seizures.
Abnormal Bleeding
Possible increased risk of bleeding.
Elevated Serum Cholesterol Concentrations
Clinically relevant increases in serum cholesterol concentrations reported in some patients after ≥3 months of therapy.
Consider monitoring serum cholesterol concentrations during long-term treatment.
Interstitial Lung Disease and Eosinophilic Pneumonia
Interstitial lung disease and eosinophilic pneumonia reported rarely; signs and symptoms may include progressive dyspnea, cough, or chest discomfort. Promptly evaluate patients with these symptoms and consider discontinuance of venlafaxine therapy.
Concomitant Illnesses
Limited experience; use with caution in patients with altered metabolism or hemodynamics or conditions that could be compromised by increased heart rate (e.g., patients with hyperthyroidism, CHF, or recent MI), particularly with venlafaxine dosages >200 mg daily.
Cognitive/Physical Impairment
Risk of impaired mental alertness or physical coordination required for performing hazardous tasks (e.g., driving or operating machinery).
Electroconvulsive Therapy (ECT)
Effects of concomitant use with ECT have not been systematically evaluated.
Specific Populations
Pregnancy
Category C.
Possible complications, sometimes severe and requiring prolonged hospitalization, respiratory support, enteral nutrition, and other forms of supportive care in neonates exposed to venlafaxine and other SNRIs or SSRIs late in the third trimester; may arise immediately upon delivery.
Carefully consider the potential risks and benefits of treatment when used during the third trimester of pregnancy. Consider cautiously tapering dose during third trimester prior to delivery.
Lactation
Distributed into milk; discontinue nursing or the drug.
Pediatric Use
Safety and effectiveness not established in pediatric patients; efficacy of venlafaxine (administered as extended-release capsules) was not established in placebo-controlled clinical studies in pediatric patients with major depressive disorder or generalized anxiety disorder. Increased hostility, suicidality (e.g., suicidal ideation, self-harm), and abnormal/changed behavior reported in controlled studies of venlafaxine in children and adolescents 6–17 years of age; also possible adverse effects on weight, height, appetite, BP, and serum cholesterol concentrations.
Regular monitoring of height and weight is recommended when prescribed for unlabeled (off-label) uses in pediatric patients, particularly during long-term administration. Long-term safety of therapy with venlafaxine extended-release capsules (beyond 6 months) not systematically evaluated.
Blood pressure elevations considered clinically important observed in children and adolescents similar to those observed in adults; observe same precautions as in adults. (See Sustained Hypertension under Cautions.)
FDA warns that a greater risk of suicidal thinking or behavior (suicidality) occurred during first few months of antidepressant treatment (4%) compared with placebo (2%) in children and adolescents with major depressive disorder, obsessive-compulsive disorder (OCD), or other psychiatric disorders based on pooled analyses of 24 short-term, placebo-controlled trials of 9 antidepressant drugs (SSRIs and others). However, a more recent meta-analysis of 27 placebo-controlled trials of 9 antidepressants (SSRIs and others) in patients <19 years of age with major depressive disorder, OCD, or non-OCD anxiety disorders suggests that the benefits of antidepressant therapy in treating these conditions may outweigh the risks of suicidal behavior or suicidal ideation. No suicides occurred in these pediatric trials.
Carefully consider these findings when assessing potential benefits and risks of venlafaxine in a child or adolescent for any clinical use. (See Risk of Suicidality and Overdosage under Cautions.)
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out. (See Hyponatremia or SIADH under Cautions.)
In pooled data analyses, a reduced risk of suicidality was observed in adults ≥65 years of age with antidepressant therapy compared with placebo. (See Boxed Warning and also see Risk of Suicidality and Overdosage under Cautions.)
Hepatic Impairment
Decreased clearance; dosage adjustment recommended. (See Hepatic Impairment under Dosage and Administration.)
Renal Impairment
Decreased clearance; dosage adjustment recommended. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
With conventional tablets: anorexia, asthenia, constipation, dizziness, dry mouth, nausea, nervousness, somnolence, sweating.
With extended-release tablets: anorexia, asthenia, constipation, decreased sexual function (e.g., abnormal ejaculation, orgasmic dysfunction, impotence in men, decreased libido), dizziness, dry mouth, headache, insomnia, abnormal dreams, nervousness, tremor, nausea, vomiting, somnolence, sweating, abnormal vision.
Drug Interactions
Metabolized by CYP isoenzymes, principally by CYP2D6 to O-desmethylvenlafaxine (ODV), its major active metabolite. Also metabolized by CYP3A4. Relatively weak inhibitor of CYP2D6. Does not inhibit CYP1A2, CYP2C9, CYP2C19, or CYP3A4.
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors of CYP2D6 or 3A4: Potential pharmacokinetic interaction (increased plasma venlafaxine concentrations). Use caution if administered concomitantly with drugs that inhibit both CYP2D6 and 3A4.
Drugs Metabolized by Hepatic Microsomal Enzymes
Potential pharmacokinetic interaction (increased substrate plasma concentrations) with concomitant use of drugs that are metabolized by CYP2D6.
Drugs Associated with Serotonin Syndrome
Potential pharmacologic interaction (serotonin syndrome) with serotonergic agents. Avoid such use, or use with caution. (See Serotonin Syndrome under Cautions.)
Protein-bound Drugs
Pharmacokinetic interaction unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
No apparent additive cognitive or psychomotor effects; no effects on venlafaxine pharmacokinetics |
Avoidance of alcohol recommended |
|
Cimetidine |
Increased plasma venlafaxine concentrations, but no effect on ODV pharmacokinetics |
No dosage adjustment required for most patients; use with caution in geriatric patients and patients with hypertension or hepatic impairment |
|
CNS agents |
Potential additive CNS effects |
Use with caution |
|
Desipramine |
Increased plasma desipramine concentrations |
|
|
Diazepam |
Pharmacokinetic or pharmacologic interactions unlikely |
|
|
Diuretics |
Consider risk of hyponatremia |
|
|
5-HT1 receptor agonists (“triptans”) |
Potentially life-threatening serotonin syndrome |
Observe carefully if used concomitantly, particularly during treatment initiation, dosage increases, or when another serotonergic agent is initiated |
|
Haloperidol |
Increased plasma haloperidol concentrations |
|
|
Imipramine |
Pharmacokinetic interaction unlikely |
|
|
Indinavir |
Decreased plasma indinavir concentrations |
|
|
Ketoconazole |
Increased peak plasma concentrations and AUCs of venlafaxine and ODV |
|
|
Lithium |
Pharmacokinetic interaction unlikely, but potentially additive serotonergic effects |
Caution advised |
|
MAO inhibitors |
Potentially fatal serotonin syndrome |
Concomitant use contraindicated Allow at least 2 weeks to elapse between discontinuance of an MAO inhibitor and initiation of venlafaxine; allow at least 1 week to elapse between discontinuance of venlafaxine and initiation of an MAO inhibitor |
|
Risperidone |
Increased plasma risperidone concentrations |
|
|
Sibutramine |
Possible serotonin syndrome |
Use with caution |
|
SSRIs |
Potentially additive serotonergic effects |
Caution advised |
|
Tolbutamide |
No effect on tolbutamide pharmacokinetics |
|
|
Tramadol |
Possible serotonin syndrome |
Use with caution |
|
Tryptophan and other serotonin precursors |
Possible serotonin syndrome |
Concomitant use not recommended |
Venlafaxine Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.
Absolute bioavailability is about 45%.
Commercially available extended-release capsules provide a slower rate of absorption but the same extent of absorption compared with the conventional tablets.
Food
Food does not appear to affect GI absorption of venlafaxine or bioavailability of ODV, its major active metabolite.
Distribution
Extent
Distributed into milk.
Plasma Protein Binding
Venlafaxine: 27%.
ODV: Approximately 30%.
Elimination
Metabolism
Extensively metabolized in the liver via CYP2D6 to O-desmethylvenlafaxine (ODV), its major active metabolite; also metabolized to N, O-didesmethylvenlafaxine and other minor metabolites. Apparently metabolized by CYP3A4 to N-desmethylvenlafaxine, a minor, less active metabolite.
Elimination Route
Renal elimination of venlafaxine and its metabolites is the primary route of excretion.
Half-life
Elimination half-lives of venlafaxine and ODV are approximately 5 and 11 hours, respectively.
Special Populations
In cirrhotic patients, elimination half-lives of venlafaxine and ODV are prolonged by about 30–60% and clearance decreased by about 30–50% compared with values in healthy subjects. Patients with more severe cirrhosis had a more substantial decrease in venlafaxine clearance (about 90%).
In renally impaired patients (GFR=10–70 mL/min), elimination half-lives of venlafaxine and ODV are prolonged by about 40–50% and venlafaxine clearance was reduced by about 24% compared with values in healthy subjects. In dialysis patients, venlafaxine and ODV elimination half-lives were prolonged by about 142–180% and clearance was reduced by about 56–57%.
Stability
Storage
Oral
Extended-release Capsules and Conventional Tablets
20–25°C.
Actions
-
Mechanisms of antidepressant and anxiolytic actions are uncertain but appear to be associated with the potentiation of neurotransmitter activity in the CNS.
-
Venlafaxine and ODV are potent inhibitors of neuronal serotonin and norepinephrine reuptake and weak inhibitors of dopamine reuptake.
-
Possesses no significant affinity for muscarinic cholinergic, H1-histaminergic, or α1-adrenergic receptors.
-
Risk of suicidality; importance of patients, caregivers, and families being alert to and immediately reporting emergence of suicidality, worsening depression, or unusual changes in behavior, especially during the first few months of therapy or during periods of dosage adjustment. FDA recommends providing written patient information (medication guide) explaining risks of suicidality each time the drug is dispensed.
-
Importance of consulting a clinician if skin rash, urticaria (hives), or a related allergic phenomenon occurs.
-
Risk of concomitant use with alcohol.
-
Importance of avoiding some activities (e.g., operating machinery, driving a motor vehicle) until effects on the individual are known.
-
Importance of patients informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal products, as well as concomitant illnesses.
-
Importance of informing patients of risk of serotonin syndrome with concurrent use of venlafaxine and 5-HT1 receptor agonists (“triptans”) or other serotonergic agents. Importance of seeking immediate medical attention if symptoms of serotonin syndrome develop.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of patients informing clinicians if they have a history of glaucoma or increased intraocular pressure.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg (of venlafaxine)* |
Effexor (scored) |
Wyeth |
|
Venlafaxine Hydrochloride Tablets |
Teva |
|||
|
37.5 mg (of venlafaxine)* |
Effexor (scored) |
Wyeth |
||
|
Venlafaxine Hydrochloride Tablets |
Teva |
|||
|
50 mg (of venlafaxine)* |
Effexor (scored) |
Wyeth |
||
|
Venlafaxine Hydrochloride Tablets |
Teva |
|||
|
75 mg (of venlafaxine)* |
Effexor (scored) |
Wyeth |
||
|
Venlafaxine Hydrochloride Tablets |
Teva |
|||
|
100 mg (of venlafaxine)* |
Effexor (scored) |
Wyeth |
||
|
Venlafaxine Hydrochloride Tablets |
Teva |
|||
|
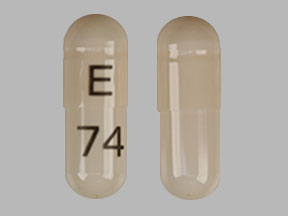
Capsules, extended-release |
37.5 mg (of venlafaxine) |
Effexor XR |
Wyeth |
|
|
75 mg (of venlafaxine) |
Effexor XR |
Wyeth |
||
|
150 mg (of venlafaxine) |
Effexor XR |
Wyeth |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions October 3, 2014. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
- How long do venlafaxine withdrawal symptoms last?
- SSRIs vs SNRIs - What's the difference between them?
More about venlafaxine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,765)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: serotonin-norepinephrine reuptake inhibitors
- Breastfeeding
- En español