Colesevelam (Monograph)
Brand name: WelChol
Drug class: Bile Acid Sequestrants
VA class: CV350
Chemical name: 2-Propen-1-amine polymer withN,N,N-trimethyl-6-(2-propenylamino)-1-hexanaminium chloride-(chloromethyl)oxirane and N-2-propenyl-1-decanamine hydrochloride
Molecular formula: (C3H7N)m(C3H5ClO)n(C12H27ClN2)o(C13H27N)p•xHCl
CAS number: 182815-44-7
Introduction
Antilipemic agent (bile acid sequestrant). Adjunct antidiabetic agent for type 2 diabetes mellitus.
Uses for Colesevelam
Primary Hypercholesterolemia
Adjunct to dietary therapy and exercise to decrease elevated serum LDL-cholesterol concentrations in the management of primary hypercholesterolemia (Frederickson type IIa).
May be used alone or combined with a hydroxymethylglutaryl-coenzyme A (HMG-CoA) reductase inhibitor (i.e., statin).
Effect of colesevelam (alone or in combination with a statin) on cardiovascular morbidity and mortality not established.
Safety and efficacy of colesevelam for management of Fredrickson type I, III, IV, and V dyslipidemias† [off-label] not established. (See Hypertriglyceridemia under Cautions.)
AHA/ACC cholesterol management guideline states that lifestyle modification is the foundation of cardiovascular risk reduction. If pharmacologic therapy is needed, statins are first-line drugs of choice because of their demonstrated benefits in reducing risk of atherosclerotic cardiovascular disease (ASCVD). The addition of a nonstatin drug (e.g., ezetimibe, bile acid sequestrants, PCSK9 inhibitor) may be considered in certain circumstances such as in patients with very severe elevations of LDL-cholesterol concentrations who are not achieving adequate LDL lowering with maximally tolerated statin therapy.
Diabetes Mellitus
Used in combination with metformin, sulfonylurea, or insulin monotherapy or in combinations with these and other oral antidiabetic agents as an adjunct to diet and exercise for the management of type 2 diabetes mellitus.
Safety and efficacy as monotherapy or in combination with a dipeptidyl peptidase-4 (DPP-4) inhibitor not established in type 2 diabetes mellitus; has not been studied extensively in combination with thiazolidinediones.
Not effective as sole therapy for type 1 diabetes mellitus or diabetic ketoacidosis.
Related/similar drugs
Ozempic, Rybelsus, atorvastatin, metformin, rosuvastatin, ezetimibe, simvastatin
Colesevelam Dosage and Administration
General
-
Institute standard lipid-lowering diet before initiation of colesevelam therapy; patient should remain on this diet during treatment with the drug.
Monitoring during Antilipemic Therapy
-
Monitor serum lipoprotein concentrations periodically.
-
Intensive control of hyperlipidemia warranted in addition to glycemic control in patients with diabetes mellitus.
Administration
Oral Administration
Administer orally once or twice daily with a liquid at mealtime.
May be administered simultaneously with a statin.
Drugs known to interact with colesevelam or drugs that have not been evaluated in formal drug interaction studies with colesevelam, especially those with a narrow therapeutic index, (see Interactions), should be administered at least 4 hours prior to colesevelam. Alternatively, monitor blood concentrations of the co-administered drug.
Dosage
Available as colesevelam hydrochloride; dosage expressed in terms of colesevelam.
Adults
Dyslipidemias
Primary Hypercholesterolemia
OralInitially, 1.875 g (3 tablets) twice daily or 3.75 g (6 tablets) once daily. May increase dosage to 4.375 g (7 tablets) daily depending on desired therapeutic effect.
Diabetes Mellitus
Oral: 1.875 g (3 tablets) twice daily or 3.75 g (6 tablets) once daily in combination with other antidiabetic agents (e.g., metformin, a sulfonylurea, insulin) in patients with type 2 diabetes mellitus.
Therapeutic response usually occurs following 4–6 weeks of treatment and reaches maximal or near maximal after 12–18 weeks of therapy.
Cautions for Colesevelam
Contraindications
-
Bowel obstruction.
-
Serum triglyceride concentrations exceeding 500 mg/dL.
-
History of hypertriglyceridemia-induced pancreatitis.
-
Known hypersensitivity to colesevelam or any ingredient in the formulation.
Warnings/Precautions
General Precautions
Hypertriglyceridemia
Increased serum triglyceride concentrations reported in patients with primary hypercholesterolemia or type 2 diabetes mellitus (particularly patients receiving concomitant insulin or sulfonylurea therapy). Severe hypertriglyceridemia can cause pancreatitis.
Not systematically studied in patients with triglyceride concentrations >300 mg/dL. Use with caution in patients with baseline triglyceride concentrations of 250–299 mg/dL; monitor lipoprotein concentrations periodically during therapy. Manufacturer recommends discontinuing therapy if serum triglyceride concentrations exceed 500 mg/dL or if hypertriglyceridemia-induced pancreatitis occurs.
Fat-soluble Vitamin Deficiency
Bile acid sequestrants may decrease absorption of fat-soluble vitamins A, D, E, and K. Effects of colesevelam on co-administered dietary or supplemental vitamin therapy, including such use in pregnant women, not established.
Hemorrhage from vitamin K deficiency reported in rats receiving relatively high doses (30 times the usual human dosage). Clinically important effects on absorption of fat-soluble vitamins not observed in clinical trials. Use caution in patients susceptible to vitamin K deficiency (e.g., concomitant warfarin therapy, malabsorption syndromes) or other fat-soluble vitamin deficiency. (See Interactions.)
GI Disorders
Large tablet size of colesevelam may cause dysphagia or esophageal obstruction; use caution in patients with dysphagia or swallowing disorders.
Not recommended in patients with gastroparesis, other GI motility disorders, or those who have undergone major GI tract surgery and who may be at risk for bowel obstruction.
Combination Therapy
When used in combination with metformin, a sulfonylurea, or insulin, consider the cautions, precautions, and contraindications associated with the concomitant agent(s).
Specific Populations
Pregnancy
Category B.
Requirements for vitamins and other nutrients increased during pregnancy. (See Fat-soluble Vitamin Deficiency under Cautions.)
Lactation
Colesevelam is not expected to distribute into milk.
Pediatric Use
Safety and efficacy not established in children <18 years of age. Not recommended in pediatric patients because of large tablet size.
Geriatric Use
No overall differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.
Renal Impairment
In patients with type 2 diabetes mellitus, no overall differences in safety or efficacy observed between patients with moderate renal insufficiency (Clcr <50 mL/minute) and those with mild renal insufficiency (Clcr ≥50 mL/minute).
Common Adverse Effects
Patients with primary hypercholesterolemia: Constipation, dyspepsia, nausea, accidental injury, asthenia, pharyngitis, flu-like syndrome, rhinitis, myalgia.
Patients with type 2 diabetes mellitus: Constipation, nasopharyngitis, dyspepsia, hypoglycemia, nausea, hypertension.
Drug Interactions
If administered with a drug with a narrow therapeutic index (i.e., alterations in blood concentrations associated with clinically important effect on efficacy and/or safety) that has not been evaluated in formal drug interaction studies, administer drug at least 4 hours prior to colesevelam, or consider monitoring drug concentrations.
Increased serum triglyceride concentrations observed in clinical studies with concomitant sulfonylurea or insulin therapy.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cephalexin |
Pharmacokinetic interaction unlikely |
|
|
Ciprofloxacin |
Pharmacokinetic interaction unlikely |
|
|
Digoxin |
Pharmacokinetic interaction unlikely |
|
|
Fat-soluble vitamins (i.e., vitamins A, D, E, K) |
Potential decreased absorption of fat-soluble vitamins A, D, E, K (see Fat-soluble Vitamin Deficiency under Cautions) |
Administer at least 4 hours prior to colesevelam |
|
Fenofibrate |
Additive effects in reducing total and LDL cholesterol |
|
|
HMG-CoA reductase inhibitors (statins) |
Additive antilipemic effects Lovastatin: Pharmacokinetic interaction unlikely |
Used to therapeutic advantage |
|
Glyburide |
Potential decreased peak plasma concentration and AUC of glyburide |
Administer at least 4 hours prior to colesevelam |
|
Metoprolol |
Pharmacokinetic interaction unlikely |
|
|
Quinidine |
Pharmacokinetic interaction unlikely |
|
|
Oral contraceptives (ethinyl estradiol combined with norethindrone) |
Decreased peak blood concentrations of ethinyl estradiol and norethindrone, decreased AUC of ethinyl estradiol |
Administer at least 4 hours prior to colesevelam |
|
Phenytoin |
Potential decreased blood phenytoin concentrations; potential for increased seizure activity |
Administer at least 4 hours prior to colesevelam |
|
Thyroid agents (e.g., levothyroxine) |
Increased TSH concentrations; decreased peak blood levothyroxine concentrations and AUC |
Administer at least 4 hours prior to colesevelam |
|
Valproic acid |
Pharmacokinetic interaction unlikely |
|
|
Verapamil (extended-release) |
Pharmacokinetic interaction unlikely |
|
|
Warfarin |
Potential reduced INR; pharmacokinetic interaction unlikely |
Monitor INR prior to colesevelam therapy and subsequently to ensure no appreciable alteration in INR; once INR is stable, monitor periodically at recommended intervals for warfarin therapy |
Colesevelam Pharmacokinetics
Absorption
Bioavailability
Not absorbed from the GI tract.
Onset
Maximum therapeutic response usually occurs within 2 weeks and is maintained during long-term (≥50 weeks) therapy.
Elimination
Elimination Route
Binds to bile acids in the intestine and forms a nonabsorbable complex that is excreted in feces.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C). Protect from moisture.
Actions
-
Binds to bile acids in the intestine and forms a nonabsorbable complex. Partial removal of bile acids from enterohepatic circulation results in increased conversion of cholesterol to bile acids in the liver. This causes an increased demand for cholesterol in liver cells, resulting in a compensatory increase in hepatic uptake (and thus systemic clearance) of circulating LDL-cholesterol.
-
Reduces serum total cholesterol, LDL-cholesterol, and apolipoprotein B (apo B), and increases HDL-cholesterol concentrations. Serum triglyceride concentrations may remain unchanged or increase slightly (5–10%).
The mechanism by which colesevelam improves glycemic control is unknown.
Advice to Patients
-
Risk of increased serum triglyceride concentrations in diabetic patients receiving colesevelam with a sulfonylurea or insulin; long-term effect of hypertriglyceridemia on CAD risk uncertain.
-
Importance of informing a clinician of high triglyceride concentrations (i.e., >300 mg/dL) before starting colesevelam therapy.
-
Importance of adherence to prescribed directions for use.
-
Importance of taking certain other drugs (e.g., glyburide, thyroid agents, oral contraceptives, warfarin, phenytoin, fat-soluble vitamins) at least 4 hours before colesevelam.
-
Importance of adhering to nondrug therapies and measures (i.e., lifestyle modifications, including dietary management, weight control, physical activity, and management of potentially contributory disease [e.g., diabetes mellitus]).
-
Importance of instructing diabetic patients regarding self-monitoring of blood glucose, adherence to meal planning, and regular physical exercise.
-
Importance of discontinuing colesevelam and seeking medical advice if severe abdominal pain or severe constipation occurs.
-
Importance of discontinuing colesevelam and seeking medical advice if symptoms of acute pancreatitis (e.g., severe abdominal pain with or without nausea, vomiting) occur.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription (e.g., glyburide, levothyroxine, oral contraceptives) and OTC (e.g., vitamins) drugs, as well as any concomitant illnesses (e.g., stomach or intestinal disease, including gastroparesis, abnormal contractions of the digestive system, or major GI surgery; vitamin A, D, E, or K deficiencies; difficulty swallowing).
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
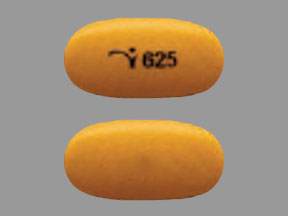
Tablets |
625 mg |
WelChol |
Daiichi Sankyo |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions July 26, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about colesevelam
- Check interactions
- Compare alternatives
- Reviews (121)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: bile acid sequestrants
- Breastfeeding
- En español