Nitrofurantoin (Monograph)
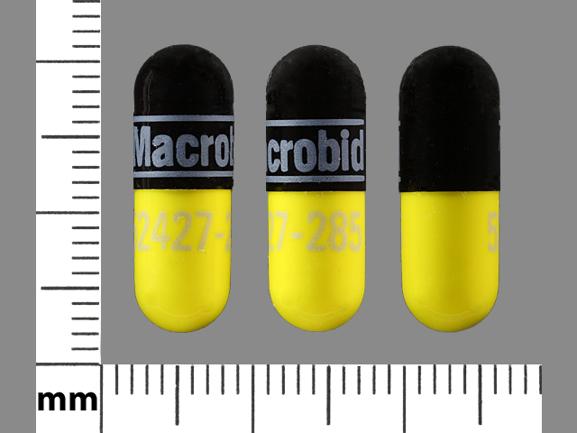
Brand names: Furadantin, Macrobid, Macrodantin
Drug class: Urinary Anti-infectives
VA class: AM600
Chemical name: 1-[[(5-Nitro-2-furanyl)methylene]amino]-2,4-imidazolidinedione
Molecular formula: C8H6N4O5
CAS number: 67-20-9
Introduction
Antibacterial; nitrofuran derivative.
Uses for Nitrofurantoin
Urinary Tract Infections (UTIs)
Treatment of UTIs caused by susceptible Staphylococcus aureus, S. saprophyticus, enterococci (e.g., Enterococcus faecalis), Escherichia coli, and some strains of Klebsiella or Enterobacter.
Consider that persistence or reappearance of bacteriuria may occur after nitrofurantoin treatment since the drug is not widely distributed into tissues. (See Selection and Use of Anti-infectives under Cautions.)
Not indicated for treatment of pyelonephritis or perinephric abscesses.
Nitrofurantoin Dosage and Administration
Administration
Oral Administration
Administer orally with food
Oral suspension is readily miscible with water, milk, fruit juice, or infant formula.
Dosage
Pediatric Patients
Urinary Tract Infections (UTIs) in Children ≥1 Month of Age
Oral
Capsules containing macrocrystals or suspension containing microcrystals: 5–7 mg/kg daily in 4 divided doses given for 7 days or for ≥3 days after urine becomes sterile.
If used for long-term suppressive therapy, manufacturers states 1 mg/kg daily given as a single dose or in 2 equally divided doses may be adequate.
Urinary Tract Infections (UTIs) in Children >12 Years of Age
Oral
Dual-release capsules: 100 mg every 12 hours for 7 days.
Adults
Urinary Tract Infections (UTIs)
Oral
Capsules containing macrocrystals or suspension containing microcrystals: 50–100 mg 4 times daily (50 mg 4 times daily for uncomplicated infections) given for 7 days or for ≥3 days after urine becomes sterile. If used for long-term suppressive therapy, manufacturer states 50–100 mg once daily at bedtime may be adequate.
Dual-release capsules: 100 mg every 12 hours for 7 days.
Cautions for Nitrofurantoin
Contraindications
-
Known hypersensitivity to nitrofurantoin.
-
Anuria, oliguria, or significant renal impairment (Clcr <60 mL/minute or clinically important Scr elevations).
-
Neonates <1 month of age. (See Pediatric Use under Cautions.)
-
Pregnant women at term (38–42 weeks of gestation), including during labor and delivery and when onset of labor is imminent. (See Pregnancy under Cautions.)
Warnings/Precautions
Warnings
Pulmonary Reactions
Acute, subacute, or chronic pulmonary reactions reported.
Discontinue nitrofurantoin immediately if an acute, subacute, or chronic pulmonary reaction is suspected. Pulmonary reactions have been cited as a contributing cause of death.
Acute pulmonary reactions usually manifested by sudden, severe dyspnea, chills, chest pain, fever, and cough; pulmonary infiltration with consolidation or pleural effusion on radiographs and eosinophilia also may occur. Usually evident within the first week of treatment and reversible when drug discontinued; resolution often is dramatic.
Fever and eosinophilia occur less frequently with subacute pulmonary reactions than with acute reaction. Recovery after subacute reactions may require several months; symptoms may become more severe if not recognized as being related to nitrofurantoin and if the drug is not discontinued.
Chronic pulmonary reactions are rare and can develop insidiously, usually in patients who have received continuous nitrofurantoin treatment for ≥6 months; the severity and degree of resolution depend on duration of nitrofurantoin treatment after symptoms first appear. Symptoms usually involve malaise, dyspnea on exertion, cough, and altered pulmonary function; radiologic and histologic examination may indicate diffuse interstitial pneumonitis and/or fibrosis; fever is rare.
Pulmonary function should be closely monitored in patients receiving long-term nitrofurantoin and the potential benefits of such therapy should be weighed against the potential risks.
Chronic pulmonary reactions may permanently impair pulmonary function (even after discontinuance of nitrofurantoin), especially if such reactions are not recognized early.
Hepatic Effects
Hepatotoxicity (including hepatitis, cholestatic jaundice, chronic active hepatitis, hepatic necrosis) reported rarely; fatalities have occurred.
Periodically monitor hepatic function during nitrofurantoin treatment since the onset of nitrofurantoin-associated hepatotoxicity may be insidious.
If hepatitis occurs, discontinue nitrofurantoin immediately and institute appropriate measures.
Peripheral Neuropathy
Peripheral neuropathy, which may be severe or irreversible, reported rarely; fatalities have occurred.
Initial symptoms include paresthesia and dysesthesia, usually of the lower extremities, which may progress to muscle weakness and muscle wasting. Severe neuropathy is characterized by edema of interstitial tissues, demyelination of peripheral nerve fibers, and secondary changes in the spinal cord and striated muscles.
Severity of symptoms and rate of recovery are not related to dosage or total amount of drug administered. Resolution varies inversely with severity of muscle weakness.
Risk of peripheral neuritis increased in patients with renal impairment (Clcr <60 mL/minute or clinically important Scr elevations), anemia, diabetes mellitus, electrolyte imbalance, vitamin B deficiency, and debilitating disease.
Optic Neuritis
Optic neuritis reported rarely.
Hematologic Effects
Hemolytic anemia reported rarely, usually in those with G-6-PD deficiency.
If hemolysis occurs, discontinue nitrofurantoin; hemolysis usually ceases when drug discontinued.
Superinfection/Clostridium difficile-associated Colitis
Possible emergence and overgrowth of nonsusceptible organism (e.g., Candida, Pseudomonas). Institute appropriate therapy if superinfection occurs.
Treatment with anti-infectives may permit overgrowth of clostridia. Consider Clostridium difficile-associated diarrhea and colitis (antibiotic-associated pseudomembranous colitis) if diarrhea develops and manage accordingly.
Some mild cases of C. difficile-associated diarrhea and colitis may respond to discontinuance alone. Manage moderate to severe cases with fluid, electrolyte, and protein supplementation; appropriate anti-infective therapy (e.g., oral metronidazole or vancomycin) recommended if colitis is severe.
General Precautions
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of nitrofurantoin and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Consider that many patients treated with nitrofurantoin are predisposed to persistence or reappearance of bacteriuria since the drug is not broadly distributed into tissues. Perform urine culture and susceptibility testing before and after nitrofurantoin treatment.
The lower eradication rates reported with nitrofurantoin should be weighed against the increased risk of systemic toxicity and development of resistance reported with anti-infectives that have broader tissue distribution. If persistence or reappearance of bacteriuria occurs after nitrofurantoin, retreat using an anti-infective with broader tissue distribution.
Systemic Infections
Not effective in systemic bacterial infections and has no effect on bacteria in blood or tissues outside the urinary tract.
Specific Populations
Pregnancy
Category B.
Contraindicated at term (38–42 weeks of gestation), including during labor and delivery and when onset of labor is imminent, since hemolytic anemia could occur in the neonate secondary to immature erythrocyte enzyme systems (glutathione instability).
Lactation
Distributed into milk; discontinue nursing or the drug.
Pediatric Use
Capsules containing macrocrystals: Contraindicated in infants <1 month of age.
Dual-release capsules: Safety and efficacy not established in children <12 years of age; contraindicated in infants <1 month of age.
Suspension containing microcrystals: Contraindicated in infants <1 month of age.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Some information suggests a higher incidence of pulmonary reactions (including fatalities) in geriatric patients; this may be related to the higher proportion of geriatric patients receiving long-term nitrofurantoin treatment. As in younger adults, chronic pulmonary reactions occur most frequently in those receiving the drug for ≥6 months. (See Pulmonary Reactions under Cautions.)
Some information suggests an increased incidence of severe hepatic effects, including fatalities, in geriatric patients. (See Hepatic Effects under Cautions.)
Consider age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy when selecting nitrofurantoin for use in geriatric patients.
Since nitrofurantoin is substantially eliminated by the kidneys; risk of adverse effects may be greater in patients with impaired renal function. Monitor renal function since geriatric patients are more likely to have renal impairment.
Renal Impairment
Patients with renal impairment are at increased risk for peripheral neuritis. (See Peripheral Neuritis under Cautions.)
If long-term therapy is used, periodically monitor for changes in renal function.
Contraindicated in those with anuria, oliguria, or significant renal impairment (Clcr <60 mL/minute or clinically important Scr elevations).
Therapeutic concentrations of nitrofurantoin may not be attained in urine of patients with Clcr <40 mL/minute.
Common Adverse Effects
GI effects (nausea, flatulence, vomiting, anorexia, diarrhea, dyspepsia, constipation, abdominal pain); headache; brown discoloration of urine.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Antacids (magnesium trisilicate) |
Decreased rate and extent of absorption of nitrofurantoin |
Avoid concomitant use |
|
Probenecid |
Possible inhibition of renal excretion of nitrofurantoin resulting in increased plasma nitrofurantoin concentrations (with increased risk of adverse effects) and decreased urine nitrofurantoin concentrations (with decreased efficacy in treatment of UTIs) |
|
|
Quinolones |
Some in vitro evidence of antagonism between quinolones and nitrofurantoin |
Clinical importance unknown |
|
Sulfinpyrazone |
Possible inhibition of renal excretion of nitrofurantoin resulting in increased plasma nitrofurantoin concentrations (with increased risk of adverse effects) and decreased urine nitrofurantoin concentrations (with decreased efficacy in treatment of UTIs) |
|
|
Tests for glucose |
Possible false-positive reactions in urine glucose tests using Benedict’s solution or Fehling’s solution |
Use glucose tests based on enzymatic glucose oxidase reactions (e.g., Clinistix, Tes-Tape) |
Nitrofurantoin Pharmacokinetics
Absorption
Bioavailability
Readily absorbed from GI tract.
May be given as an oral suspension containing nitrofurantoin microcrystals, as capsules containing nitrofurantoin macrocrystals, or as dual-release capsules containing nitrofurantoin macrocrystals (25%) and nitrofurantoin monohydrate (75%).
Absorption of macrocrystals is slower than that of microcrystals. The dual-release capsules provide slow release of nitrofurantoin over time.
Only negligible antibacterial activity attained in plasma. In adults with normal renal function, peak antibacterial concentrations attained in urine within 30 minutes following administration of nitrofurantoin microcrystals; peak urine concentrations attained more slowly with macrocrystals or dual-release capsules.
Food
Food in GI tract increases extent of absorption, presumably by increasing dissolution of the drug. Effect is most apparent with macrocrystals, resulting in a 40% increase in bioavailability if dual-release capsules are given with food.
Distribution
Extent
Only limited distribution into tissues.
Crosses the placenta.
Distributed into milk.
Plasma Protein Binding
20–60%.
Elimination
Metabolism
Partially metabolized, principally in the liver; small amounts of the drug are reduced to aminofurantoin.
Elimination Route
20–44% of a dose eliminated unchanged in urine by glomerular filtration and tubular secretion; about 1% eliminated as aminofurantoin.
Special Populations
Plasma concentrations are higher and half-life prolonged in patients with renal impairment. Therapeutic concentrations of nitrofurantoin may not be attained in urine of patients with Clcr <40 mL/minute.
Stability
Storage
Oral
Capsules
15–30°C. Protect from light.
Suspension
20–25°C in tight, light-resistant containers. Dispense in glass amber bottle; exposure to strong light may darken drug. Protect from freezing.
Actions and Spectrum
-
Usually bacteriostatic, but may be bactericidal at concentrations attained in urine.
-
Nitrofurantoin appears to be reduced by bacterial flavoproteins to reactive intermediates that inactivate or alter ribosomal proteins and other macromolecules in susceptible bacteria resulting in inhibition of aerobic energy metabolism and protein, DNA, RNA, and cell wall synthesis.
-
Spectrum of activity includes some gram-positive and -negative aerobes.
-
Gram-positive aerobes: Active in vitro and in clinical infections against Staphylococcus saprophyticus and enterococci (e.g., Enterococcus faecalis). Also active in vitro against S. aureus, coagulase-negative staphylococci (including S. epidermidis), Streptococcus agalactiae (group B streptococci), group D streptococci, and viridans streptococci.
-
Gram-negative aerobes: Active in vitro and in clinical infections against Escherichia coli. Also active in vitro against Citrobacter amalonaticus, C. diversus, C. freundii, Klebsiella oxytoca, and K. ozaenae. Some strains of Enterobacter and Klebsiella are resistant. Pseudomonas and most Proteus and Serratia also are resistant.
-
Cross-resistance with other anti-infectives has not been reported.
Advice to Patients
-
Advise patients that antibacterials (including nitrofurantoin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).
-
Importance of completing full course of therapy, even if feeling better after a few days.
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with nitrofurantoin or other antibacterials in the future.
-
Importance of taking with food to improve drug absorption and enhance tolerance. Consider that some patients who cannot tolerate microcrystalline nitrofurantoin are able to take the macrocrystal preparations without nausea.
-
Importance of not using antacids containing magnesium trisilicate during nitrofurantoin treatment.
-
Importance of contacting clinician if any unusual symptoms occur during nitrofurantoin treatment.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules (macrocrystals) |
25 mg |
Macrodantin |
Procter & Gamble |
|
50 mg* |
Macrodantin |
Procter & Gamble |
||
|
Nitrofurantoin Capsules (Macrocrystals) |
Mylan |
|||
|
100 mg* |
Macrodantin |
Procter & Gamble |
||
|
Nitrofurantoin Capsules (Macrocrystals) |
Mylan |
|||
|
Capsules, dual-release |
equivalent to nitrofurantoin 100 mg (provided by nitrofurantoin macrocrystals 25 mg and nitrofurantoin monohydrate 75 mg)* |
Macrobid (with povidone) |
Procter & Gamble |
|
|
Nitrofurantoin Capsules (dual-release) |
Mylan |
|||
|
Suspension (microcrystals) |
25 mg/5 mL |
Furadantin (with parabens) |
First Horizon |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions June 1, 2006. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
More about nitrofurantoin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1,856)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: urinary anti-infectives
- Breastfeeding
- En español
Patient resources
Professional resources
- Nitrofurantoin Capsules prescribing information
- Nitrofurantoin Macrocrystals (FDA)
- Nitrofurantoin Oral Suspension (FDA)
Other brands
Macrobid, Macrodantin, Furadantin