Imuran
Generic name: azathioprine [ ay-za-THYE-oh-preen ]
Brand names: Azasan, Imuran
Drug classes: Antirheumatics, Other immunosuppressants
What is Imuran?
Imuran weakens your body's immune system, to help keep it from "rejecting" a transplanted organ such as a kidney. Organ rejection happens when the immune system treats the new organ as an invader and attacks it.
Imuran is used to prevent your body from rejecting a transplanted kidney. This medicine is also used to treat symptoms of rheumatoid arthritis.
Imuran may also be used for purposes not listed in this medication guide.
Imuran side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Imuran may cause a serious brain infection that can lead to disability or death. Call your doctor right away if you have problems with speech, thought, vision, or muscle movement. These symptoms may start gradually and get worse quickly.
Stop using Imuran and call your doctor right away if you have any of these symptoms of lymphoma:
-
fever, swollen glands, body aches, night sweats, not feeling well;
-
pale skin, rash, easy bruising or bleeding;
-
cold hands and feet, feeling light-headed or short of breath;
-
pain in your upper stomach that may spread to your shoulder; or
-
feeling full after eating only a small amount, weight loss.
Also call your doctor at once if you have:
-
signs of infection (fever, chills, weakness, flu symptoms, sore throat, cough, pain or burning when you urinate);
-
severe nausea, vomiting, or diarrhea;
-
easy bruising, unusual bleeding;
-
rapid heartbeats, shortness of breath;
-
pale skin, cold hands and feet; or
-
dark urine, jaundice (yellowing of the skin or eyes).
Common side effects of Imuran may include:
-
nausea, diarrhea, stomach pain;
-
hair loss; or
-
skin rash.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Entyvio, Rinvoq, Benlysta, Stelara, Kesimpta, Avonex, Cimzia
Warnings
Imuran may cause a rare type of lymphoma (cancer) of the liver, spleen, and bone marrow that can be fatal. This has occurred mainly in teenagers and young men with Crohn's disease or ulcerative colitis.
Before taking this medicine
You should not take Imuran if you are allergic to Imuran.
You should not use Imuran to treat rheumatoid arthritis if you are pregnant. This medicine can harm an unborn baby. Use effective birth control to prevent pregnancy while using this medicine.
Imuran may cause a rare type of lymphoma (cancer) of the liver, spleen, and bone marrow that can be fatal. This has occurred mainly in teenagers and young men with Crohn's disease or ulcerative colitis. However, anyone with an inflammatory autoimmune disorder may have a higher risk of lymphoma. Talk with your doctor about your own risk.
While taking Imuran, you may have a higher risk of developing skin cancer. Ask your doctor about skin symptoms to watch for.
Tell your doctor if you have ever had:
-
kidney disease, or a kidney transplant (if you are using Imuran for rheumatoid arthritis);
-
any type of viral, bacterial, or fungal infection;
-
liver disease; or
-
chemotherapy with medications like cyclophosphamide, chlorambucil, melphalan, busulfan, and others.
You should not breast-feed while you are using Imuran.
How should I take Imuran?
Your doctor will perform blood tests to make sure you do not have conditions that would prevent you from safely using Imuran.
Follow all directions on your prescription label and read all medication guides or instruction sheets. Your doctor may occasionally change your dose. Use the medicine exactly as directed.
When given for kidney transplant, Imuran is usually given right before or on the day of transplant. For rheumatoid arthritis, this medicine is taken on a daily basis.
It may take up to 8 weeks before your symptoms improve. Keep using Imuran as directed and tell your doctor if your symptoms have not improved after 12 weeks of use.
Take with food if Imuran upsets your stomach.
You may not be able to continue taking other arthritis medications together with Imuran. Do not change your dose or dosing schedule without your doctor's advice.
Imuran affects your immune system. You may get infections more easily, even serious or fatal infections. Your doctor will need to examine you on a regular basis.
Store at room temperature away from moisture, heat, and light. Keep the bottle tightly closed when not in use.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while taking Imuran?
Avoid sunlight or tanning beds. Imuran can increase your risk of developing skin cancer. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Avoid being near people who are sick or have infections. Tell your doctor at once if you develop signs of infection.
Do not receive a "live" vaccine while using Imuran. The vaccine may not work as well and may not fully protect you from disease. Live vaccines include measles, mumps, rubella (MMR), polio, rotavirus, typhoid, yellow fever, varicella (chickenpox), and zoster (shingles).
What other drugs will affect Imuran?
Tell your doctor about all your current medicines. Many drugs can affect Imuran, especially:
-
febuxostat; or
This list is not complete and many other drugs may affect Imuran. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
More about Imuran (azathioprine)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (64)
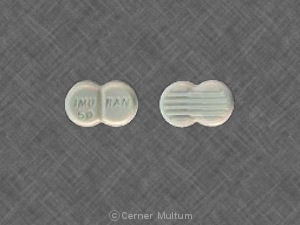
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Drug class: antirheumatics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 7.01.