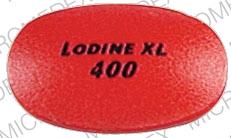
Lodine XL Side Effects
Generic name: etodolac
Medically reviewed by Drugs.com. Last updated on Nov 20, 2023.
Note: This document contains side effect information about etodolac. Some dosage forms listed on this page may not apply to the brand name Lodine XL.
Applies to etodolac: oral capsule, oral tablet, oral tablet extended release.
Warning
Oral route (Tablet; Capsule; Tablet, Extended Release)
NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may be increased in patients with cardiovascular disease or risk factors for cardiovascular disease. Etodolac is contraindicated for the treatment of perioperative pain in the setting of CABG surgery. NSAIDs can also cause an increased risk of serious gastrointestinal adverse events especially in the elderly, including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal.
Serious side effects of Lodine XL
Along with its needed effects, etodolac (the active ingredient contained in Lodine XL) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking etodolac:
More common
- Belching
- bloody or black, tarry stools
- blurred vision
- body aches or pain
- chest pain
- cloudy urine
- constipation
- cough or hoarseness
- decrease in urine output or decrease in urine-concentrating ability
- diarrhea
- dizziness
- dryness or soreness of throat
- feeling of indigestion
- fever or chills
- headache
- increased bleeding time
- itching, skin rash
- loss of appetite
- lower back or side pain
- nausea and vomiting
- nervousness
- pain in the chest below the breastbone
- painful or difficult urination
- pale skin
- pounding in the ears
- runny nose
- slow or fast heartbeat
- stomach bloating, burning, cramping, or pain
- swelling
- tender, swollen glands in neck
- trouble in swallowing
- trouble breathing
- unusual bleeding or bruising
- unusual tiredness or weakness
- voice changes
- vomiting of blood or material that looks like coffee grounds
- weight loss
Symptoms of overdose
- Agitation
- change in consciousness
- confusion
- depression
- difficult or trouble breathing
- hives
- hostility
- irregular, fast or slow, or shallow breathing
- irritability
- loss of consciousness
- muscle twitching
- pain or discomfort in chest, upper stomach, or throat
- pale or blue lips, fingernails, or skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- rapid weight gain
- seizures
- sleepiness
- stupor
- swelling of face, ankles, or hands
- tightness in chest
- trouble breathing
- unusual drowsiness, dullness, or feeling of sluggishness
Other side effects of Lodine XL
Some side effects of etodolac may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Bloated, full feeling
- continuing ringing or buzzing or other unexplained noise in ears
- excess air or gas in stomach or intestines
- hearing loss
- lack or loss of strength
- passing gas
- sneezing
- stuffy nose
For Healthcare Professionals
Applies to etodolac: oral capsule, oral tablet, oral tablet extended release.
General
The most frequently reported side effects were gastrointestinal in nature and included dyspepsia, abdominal pain, constipation, diarrhea, dyspepsia, flatulence, gross bleeding/perforation, heartburn, nausea, gastric ulcers, duodenal ulcers, and vomiting.[Ref]
Gastrointestinal
Very common (10% or more): Dyspepsia (10%)
Common (1% to 10%): Abdominal pain, constipation, diarrhea, dyspepsia, flatulence, gross bleeding/perforation, heartburn, nausea, gastric ulcer, duodenal ulcer, vomiting, abdominal distention, epigastric pain, stools abnormal, gastritis, melena
Very rare (less than 0.01%): Pancreatitis
Frequency not reported: Dry mouth, ulcerative stomatitis, eructation, peptic ulcer, gastrointestinal (GI) bleeding, perforation, esophagitis, esophageal stricture, cardiospasm, colitis, GI discomfort, burning sensation, gastralgia, upper abdominal discomfort, glossitis, hematemesis, rectal bleeding, heartburn, indigestion, ulcerative colitis exacerbated, Crohn's disease exacerbated
Postmarketing reports: Intestinal ulceration[Ref]
Cardiovascular
Frequency not reported: Hypertension, congestive heart failure, flushing, palpitations, arrhythmia, myocardial infarction, tachycardia, cardiac failure
Postmarketing reports: Necrotizing vasculitis[Ref]
Renal
Common (1% to 10%): Renal function abnormal
Frequency not reported: Renal calculus, interstitial nephritis, renal impairment, nephrotoxicity, nephrotic syndrome, renal failure
Postmarketing reports: Renal insufficiency, renal papillary necrosis[Ref]
Nervous system
Common (1% to 10%): Dizziness, headache
Frequency not reported: Syncope, somnolence, cerebrovascular accident, paresthesia, taste perversion, loss of taste, convulsion, coma, tremor, drowsiness, optic neuritis, stroke[Ref]
Dermatologic
Common (1% to 10%): Pruritus, rash
Very rare (less than 0.01%): Stevens-Johnson Syndrome, toxic epidermal necrolysis
Frequency not reported: Ecchymosis, angioedema, sweating, urticaria, exfoliative dermatitis, vesiculobullous rash, hyperpigmentation, alopecia, maculopapular rash, photosensitivity, skin peeling, purpura, erythema multiforme
Postmarketing reports: Allergic vasculitis, cutaneous vasculitis, leukocytoclastic vasculitis[Ref]
Hepatic
Common (1% to 10%): Liver enzymes increased
Frequency not reported: Bilirubinuria, hepatitis, jaundice
Postmarketing reports: Cholestatic hepatitis, hepatitis, cholestatic jaundice, duodenitis, hepatic failure, liver necrosis, fatal fulminant hepatitis[Ref]
Hematologic
Common (1% to 10%): Anemia, bleeding time increased
Frequency not reported: Thrombocytopenia, lymphadenopathy, neutropenia, agranulocytosis, hemolytic anemia, aplastic anemia, pancytopenia, leukopenia[Ref]
Metabolic
Frequency not reported: Anorexia
Postmarketing reports: Hyperglycemia[Ref]
Psychiatric
Common (1% to 10%): Depression, nervousness
Frequency not reported: Insomnia, confusion, anxiety, dreams abnormal, hallucination, disorientation[Ref]
Genitourinary
Common (1% to 10%): Dysuria, urinary frequency
Frequency not reported: Cystitis, hematuria, leukorrhea, uterine bleeding irregular, oliguria, polyuria, proteinuria[Ref]
Ocular
Common (1% to 10%): Vision blurred
Frequency not reported: Photophobia, transient visual disturbance, conjunctivitis[Ref]
Respiratory
Frequency not reported: Asthma/aggravated asthma, bronchitis, bronchospasm, dyspnea, pharyngitis, rhinitis, sinusitis, respiratory depression, pneumonia
Postmarketing reports: Pulmonary infiltration eosinophilic[Ref]
Musculoskeletal
Common (1% to 10%): Arthralgia
Frequency not reported: Muscle pain[Ref]
Other
Common (1% to 10%): Edema, tinnitus, fever, chills, asthenia, malaise, fatigue
Frequency not reported: Serum creatinine increased, infection, weight abnormal, irritability, deafness, meningitis, vertigo, sepsis, death, weakness, aseptic meningitis
Postmarketing reports: Thirst, BUN increased[Ref]
Immunologic
Frequency not reported: Allergic/hypersensitivity reaction, anaphylactic/anaphylactoid reaction[Ref]
More about Lodine XL (etodolac)
- Check interactions
- Compare alternatives
- Drug images
- Latest FDA alerts (4)
- Dosage information
- During pregnancy
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
References
1. Product Information. Lodine (etodolac). Wyeth-Ayerst Laboratories. 2001;PROD.
2. Cerner Multum, Inc. UK Summary of Product Characteristics.
3. Product Information. Etodolac ER (etodolac). Taro Pharmaceuticals U.S.A. Inc. 2016.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.