Epivir Side Effects
Generic name: lamivudine
Medically reviewed by Drugs.com. Last updated on May 21, 2023.
Note: This document contains side effect information about lamivudine. Some dosage forms listed on this page may not apply to the brand name Epivir.
Applies to lamivudine: oral solution, oral tablet.
Warning
Oral route (Tablet; Solution)
Epivir®Exacerbations of Hepatitis B, and Different Formulations of LamivudineExacerbations of Hepatitis BSevere acute exacerbations of hepatitis B have been reported in patients who are co-infected with hepatitis B virus (HBV) and human immunodeficiency virus (HIV-1) and have discontinued lamivudine. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who discontinue lamivudine and are co-infected with HIV-1 and HBV. If appropriate, initiation of anti-hepatitis B therapy may be warranted.Important Differences Among Lamivudine-Containing ProductsEpivir® tablets and oral solution (used to treat HIV-1 infection) contain a higher dose of the active ingredient (lamivudine) than Epivir-HBV® tablets and oral solution (used to treat chronic hepatitis B virus infection). Patients with HIV-1 infection should receive only dosage forms appropriate for treatment of HIV-1.
Oral route (Tablet; Solution)
Epivir-HBV®Severe acute exacerbations of hepatitis B have been reported in patients who have discontinued anti-hepatitis B therapy (including lamivudine). Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who discontinue anti-hepatitis B therapy. If appropriate, initiation of anti-hepatitis B therapy may be warranted.Lamivudine is not approved for the treatment of HIV-1 infection because the lamivudine dosage in this formulation is subtherapeutic and monotherapy is inappropriate for the treatment of HIV-1 infection. HIV-1 resistance may emerge in chronic hepatitis B-infected patients with unrecognized or untreated HIV-1 infection. HIV counseling and testing should be offered to all patients before beginning treatment with lamivudine and periodically during treatment.
Serious side effects of Epivir
Along with its needed effects, lamivudine (the active ingredient contained in Epivir) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking lamivudine:
Incidence not known
- Black, tarry stools
- bleeding gums
- bloating
- blood in the urine or stools
- blurred vision
- chills
- constipation
- cough
- dark urine
- decreased appetite
- diarrhea
- difficulty with swallowing
- dizziness
- dry mouth
- fast heartbeat
- fast, shallow breathing
- fever
- flushed, dry skin
- fruit-like breath odor
- general feeling of discomfort
- general tiredness and weakness
- increased hunger
- increased thirst
- increased urination
- indigestion
- light-colored stools
- loss of appetite
- muscle cramps, pain, stiffness, or spasms
- nausea
- pains in the stomach, side, or abdomen, possibly radiating to the back
- pinpoint red spots on the skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- right upper abdominal or stomach pain and fullness
- skin rash, hives, or itching
- sleepiness
- stomach discomfort
- tightness in the chest
- troubled breathing with exertion
- unexplained weight loss
- unusual bleeding or bruising
- unusual tiredness or weakness
- upper right abdominal or stomach pain
- vomiting
- yellow eyes or skin
Other side effects of Epivir
Some side effects of lamivudine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Belching
- burning, tingling, numbness or pain in the hands, arms, feet, or legs
- depression
- general feeling of discomfort or illness
- headache
- heartburn
- indigestion
- joint pain
- sensation of pins and needles
- sore throat
- stabbing pain
- stomach discomfort, upset, or pain
- stuffy or runny nose
- trouble sleeping
- weight loss
Incidence not known
- Hair loss or thinning of the hair
- pale skin
- sweating
- weight gain around your neck, upper back, breast, face, or waist
For Healthcare Professionals
Applies to lamivudine: oral solution, oral tablet.
General
The most common side effects reported with this drug have included headache, nausea, malaise, fatigue, nasal signs and symptoms, respiratory tract infections, throat and tonsil discomfort, abdominal discomfort and pain, vomiting, diarrhea, and cough. During clinical studies in HIV-1-infected patients, this drug was used with zidovudine (with or without other antiretroviral agents). Patients with hepatitis B virus (HBV) infection received lamivudine (the active ingredient contained in Epivir) monotherapy.[Ref]
Gastrointestinal
Increased serum lipase (at least 2.5 times the upper limit of normal [2.5 x ULN]) and amylase (greater than 2 x ULN) have been reported in 10% and up to 4.2% of patients, respectively. Amylase increases greater than 3 x ULN have also been reported.
Pancreatitis has been reported infrequently in adults, but has been more common in pediatric patients (up to 18% in 2 limited studies).[Ref]
Very common (10% or more): Nausea (up to 42%), diarrhea (up to 18%), vomiting (up to 15%), nausea and vomiting (up to 13%), abdominal discomfort and pain (up to 11.3%)
Common (1% to 10%): Abdominal pain, increased serum lipase, dyspeptic symptoms, abdominal cramps, taste disorders, abdominal discomfort, dyspepsia, increased amylase, upper abdominal pain, fungal gastrointestinal (GI) infection, GI discomfort and pain, gaseous symptoms
Uncommon (0.1% to 1%): Pancreatitis
Rare (0.01% to 0.1%): Abnormal pancreatic enzymes
Frequency not reported: Oral ulcerations, lesions
Postmarketing reports: Stomatitis, pancreatitis[Ref]
Nervous system
Very common (10% or more): Headache (up to 35.1%), dizziness (up to 35%), neuropathy (12.4%)
Common (1% to 10%): Hypnagogic effects, peripheral paresthesia
Uncommon (0.1% to 1%): Paresthesia, hypoesthesia
Very rare (less than 0.01%): Peripheral neuropathy
Postmarketing reports: Peripheral neuropathy, paresthesia[Ref]
Other
Very common (10% or more): Fatigue (up to 29%); malaise and fatigue (up to 27%); ear, nose, and throat infections (up to 25%)
Common (1% to 10%): Fever/chills; fever; malaise; viral ear, nose, and throat infection; viral infection
Postmarketing reports: Weakness
Antiretroviral therapy:
-Frequency not reported: Increased weight, increased blood lipid levels
Combination antiretroviral therapy:
-Frequency not reported: Fat loss, fat gain[Ref]
Hepatic
Very common (10% or more): Posttreatment ALT elevations (up to 27%), ALT elevations
Common (1% to 10%): Increased liver function tests, elevated AST, elevated ALT, abnormal liver function tests
Uncommon (0.1% to 1%): Elevated bilirubin, transient elevations in liver enzymes (AST, ALT)
Rare (0.01% to 0.1%): Hepatitis
Frequency not reported: Severe hepatomegaly with steatosis, hepatic decompensation, exacerbations of hepatitis/recurrent hepatitis
Postmarketing reports: Hepatic steatosis, posttreatment exacerbation of hepatitis B[Ref]
In HBV patients monitored for up to 16 weeks after discontinuing therapy, posttreatment ALT elevations occurred more often in those who had taken the HBV-specific product than subjects who had taken placebo.
Elevated AST (greater than 5 x ULN), ALT (greater than 5 x ULN), and bilirubin (greater than 2.5 x ULN) have been reported in up to 4%, up to 3.8%, and up to 0.8% of patients, respectively. ALT increases greater than 3 x ULN have also been reported.
Exacerbations of hepatitis (primarily detected by serum ALT elevations) have been reported during HBV therapy and after drug discontinuation. Most events were self-limited; however, fatalities were reported in some cases.
Lactic acidosis and severe hepatomegaly with steatosis (including fatal cases) have been reported with the use of nucleoside analogs.
Hepatic decompensation (some fatal) has been reported in patients coinfected with HIV-1 and hepatitis C receiving combination antiretroviral therapy for HIV-1 and interferon alfa with or without ribavirin.
Severe acute exacerbations of hepatitis B (including fatalities) have been reported in HBV-infected patients (including those coinfected with HIV-1) who have discontinued this drug. The causal relationship to stopping therapy was unknown.[Ref]
Psychiatric
Very common (10% or more): Dreams (up to 26%), sleep disorders (up to 16%), insomnia and other sleep disorders (11%), mood disorders (up to 11%)
Common (1% to 10%): Depressive disorders, anxiety[Ref]
Dermatologic
Very common (10% or more): Rash (up to 23%)
Common (1% to 10%): Alopecia, pruritus, sweating, fungal skin infections, acne and folliculitis, viral skin infection
Rare (0.01% to 0.1%): Angioedema
Frequency not reported: Paronychia, periungual pyogenic granulomata
Postmarketing reports: Urticaria, rash, pruritus, alopecia[Ref]
Respiratory
Very common (10% or more): Nasal signs and symptoms (20%), cough (up to 18%), viral respiratory infections (up to 15%), sore throat (13%), throat and tonsil discomfort and pain (up to 11.6%)
Common (1% to 10%): Bronchitis, sinus disorders, sinusitis, throat signs and symptoms, upper respiratory inflammation, breathing disorders
Frequency not reported: Respiratory tract infections, throat and tonsil discomfort
Postmarketing reports: Abnormal breath sounds/wheezing[Ref]
Hematologic
Decreased absolute neutrophil count (less than 750/mm3), platelets (less than 50,000/mm3), and hemoglobin (less than 8 g/dL) have been reported in up to 15%, up to 4%, and up to 2.9% of patients, respectively.
Severe neutropenia and severe anemia have been reported infrequently.[Ref]
Very common (10% or more): Decreased absolute neutrophil count (up to 15%)
Common (1% to 10%): Lymphatic signs and symptoms, neutropenia, decreased white cells, anemia, decreased platelets, decreased hemoglobin
Uncommon (0.1% to 1%): Thrombocytopenia
Very rare (less than 0.01%): Pure red cell aplasia
Postmarketing reports: Severe anemias progressing on therapy, lymphadenopathy, splenomegaly, anemia (including pure red cell aplasia), thrombocytopenia[Ref]
Musculoskeletal
Elevated CPK (at least 7 x baseline) has been reported in 9% of patients.[Ref]
Very common (10% or more): Musculoskeletal pain (up to 13.5%)
Common (1% to 10%): Elevated creatine phosphokinase (CPK), myalgia, arthralgia, muscle disorders, cramps
Rare (0.01% to 0.1%): Rhabdomyolysis
Frequency not reported: Osteonecrosis
Postmarketing reports: Muscle weakness, elevated CPK, rhabdomyolysis, muscle disorders (including myalgia, cramps)[Ref]
Metabolic
Very common (10% or more): Anorexia (up to 12%)
Common (1% to 10%): Anorexia and/or decreased appetite, hypertriglyceridemia, hyperamylasemia, abnormal enzyme levels
Uncommon (0.1% to 1%): Eating problems, disorders of thirst/fluid intake
Very rare (less than 0.01%): Lactic acidosis
Postmarketing reports: Hyperglycemia, redistribution/accumulation of body fat, hyperlactatemia, lactic acidosis
Antiretroviral therapy:
-Frequency not reported: Increased glucose levels[Ref]
Lactic acidosis and severe hepatomegaly with steatosis (including fatal cases) have been reported with the use of nucleoside analogs.[Ref]
Hypersensitivity
Frequency not reported: Anaphylactoid reaction
Postmarketing reports: Anaphylaxis[Ref]
Immunologic
Frequency not reported: Immune reconstitution/reactivation syndrome, autoimmune disorders in the setting of immune reconstitution (e.g., Graves' disease, polymyositis, Guillain-Barre syndrome, autoimmune hepatitis)[Ref]
Renal
Frequency not reported: Fanconi syndrome (at least 1 case)[Ref]
Ocular
Frequency not reported: Eye redness[Ref]
Frequently asked questions
- What drugs are contained in the HIV treatment Delstrigo?
- What is the difference between HIV treatments Symfi and Symfi Lo?
- How much does HIV treatment Cimduo cost?
- What drugs are contained in the HIV treatment Cimduo?
- What drugs are contained in the HIV treatment Symfi Lo?
More about Epivir (lamivudine)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
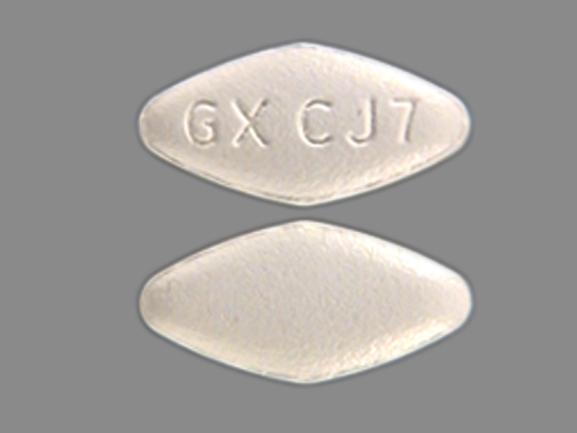
- Drug images
- Dosage information
- During pregnancy
- Generic availability
- Drug class: nucleoside reverse transcriptase inhibitors (NRTIs)
- Breastfeeding
- En español
Patient resources
Professional resources
Other formulations
Related treatment guides
References
1. van Leeuwen R, Lange JM, Hussey EK, Donn KH, Hall ST, Harker AJ, Jonker P, Danner SA. The safety and pharmacokinetics of a reverse transcriptase inhibitor, 3TC, in patients with HIV infection: a phase I study. AIDS. 1992;6:1471-5.
2. Pluda JM, Cooley TP, Montaner JS, Shay LE, Reinhalter NE, Warthan SN, Ruedy J, Hirst HM, Vicary CA, Quinn JB, et al. A phase I/II study of 2'-deoxy-3'-thiacytidine (lamivudine) in patients with advanced human immunodeficiency virus infection. J Infect Dis. 1995;171:1438-47.
3. van Leeuwen R, Katlama C, Kitchen V, Boucher CA, Tubiana R, McBride M, Ingrand D, Weber J, Hill A, McDade H, et al. Evaluation of safety and efficacy of 3TC (lamivudine) in patients with asymptomatic or mildly symptomatic human immunodeficiency virus infection: a phase I/II study. J Infect Dis. 1995;171:1166-71.
4. van Leeuwen R, Boucher C, Reiss P, Schuurman R, Nijhuis M, Danner S. Safety and efficacy of ZDV addition to 3TC monotherapy. Int Conf AIDS. 1994;10:21(ab.no.057b).
5. Product Information. Epivir (lamivudine). Glaxo Wellcome. 2001;PROD.
6. Brinkman K, terHofstede HJM, Burger DM, Smeitinkt JAM, Koopmans PP. Adverse effects of reverse transcriptase inhibitors: mitochondrial toxicity as common pathway. AIDS. 1998;12:1735-44.
7. Product Information. Epivir HBV (lamiVUDine). Glaxo Wellcome. PROD.
8. Drugs for HIV infection. Med Lett Drugs Ther. 2001;43:103-8.
9. Rivkina A, Rybalov S. Chronic hepatitis B: current and future treatment options. Pharmacotherapy. 2002;22:721-37.
10. Cerner Multum, Inc. UK Summary of Product Characteristics.
11. Warnke D, Barreto J, Temesgen Z. Antiretroviral drugs. J Clin Pharmacol. 2007;47:1570-9.
12. Cerner Multum, Inc. Australian Product Information.
13. Nelson M, Azwa A, Sokwala A, Harania RS, Stebbing J. Fanconi syndrome and lactic acidosis associated with stavudine and lamivudine therapy. AIDS. 2008;22:1374-6.
14. Danner S, van Leeuwen R, Katlama C, Ingrand D, Weber J, Kitchen V. 3TC in HIV positive, asymptomatic or mild ARC patients. Int Conf AIDS. 1993;9:477(ab.no.po-b26-205.
15. Piacenti FJ. An update and review of antiretroviral therapy. Pharmacotherapy. 2006;26:1111-33.
16. Asari A, Iles-Smith H, Chen YC, et al. Pharmacokinetics of lamivudine in subjects receiving peritoneal dialysis in end-stage renal failure. Br J Clin Pharmacol. 2007;64:738-44.
17. Cupler EJ, Dalakas MC. Exacerbation of peripheral neuropathy by lamivudine. Lancet. 1995;345:460-1.
18. SaintMarc T, Partisani M, PoizotMartin I, Bruno F, Rouviere O, Lang JM, Gastaut JA, Touraine JL. A syndrome of peripheral fat wasting (Lipodystrophy) in patients receiving long-term nucleoside analogue therapy. AIDS. 1999;13:1659-67.
19. Mallal SA, John M, Moore CB, James IR, McKinnon EJ. Contribution of nucleoside analogue reverse transcriptase inhibitors to subcutaneous fat wasting in patients with HIV infection. Aids. 2000;14:1309-16.
20. Martinez E, Mocroft A, GarciaViejo MA, PerezCuevas JB, Blanco JL, Mallolas J, Bianchi L, Conget I, Blanch J, Phillips A, Gatell. Risk of lipodystrophy in HIV-1-infected patients treated with protease inhibitors: a prospective cohort study. Lancet. 2001;357:592-8.
21. denBrinker M, Wit FWNM, WertheimvanDillen PME, Jurriaans S, Weel J, vanLeeuwen R, Pakker NG, Reiss P, Danner SA, Weverling G. Hepatitis B and C virus co-infection and the risk for hepatotoxicity of highly active antiretroviral therapy in HIV-1 infection. Aids. 2000;14:2895-902.
22. Bruno R, Sacchi P, Filice C, Filice G. Acute liver failure during lamivudine treatment in a hepatitis B cirrhotic patient. Am J Gastroenterol. 2001;96:265.
23. Ormseth EJ, Holtzmuller KC, Goodman ZD, Colonna JO, Batty DS, Sjogren MH. Hepatic decompensation associated with lamivudine: A case report and review of lamivudine-induced hepatotoxicity. Am J Gastroenterol. 2001;96:1619-22.
24. Cameron DW, Becker S, King MS, et al. Exploratory study comparing the metabolic toxicities of a lopinavir/ritonavir plus saquinavir dual protease inhibitor regimen versus a lopinavir/ritonavir plus zidovudine/lamivudine nucleoside regimen. J Antimicrob Chemother. 2007;59:957-63.
25. Fong IW. Hair loss associated with lamivudine. Lancet. 1994;344:1702.
26. Williams LH, Fleckman P. Painless periungual pyogenic granulomata associated with reverse transcriptase inhibitor therapy in a patient with human immunodeficiency virus infection. Br J Dermatol. 2007;156:163-4.
27. Weitzel T, Plettenberg A, Albrecht D, Lorenzen T, Stoehr A. Severe anaemia as a newly recognized side-effect caused by lamivudine. AIDS. 1999;13:2309-11.
28. Kainer MA, Mijch A. Anaphylactoid reaction, angioedema, and urticaria associated with lamivudine. Lancet. 1996;348:1519.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.