Chlorpromazine Side Effects
Medically reviewed by Drugs.com. Last updated on Dec 23, 2024.
Applies to chlorpromazine: oral tablets, parenteral injection.
Important warnings
This medicine can cause some serious health issues
-
Increased Mortality in Geriatric Patients with Dementia-related Psychosis
- Geriatric patients with dementia-related psychosis treated with antipsychotic agents are at an increased risk of death.101 105 106 n
- Analyses of 17 placebo-controlled trials in geriatric patients mainly receiving atypical antipsychotic agents revealed an approximate 1.6- to 1.7-fold increase in mortality compared with that in patients receiving placebo.101 105 106 n
- Most fatalities appeared to result from cardiovascular-related events (e.g., heart failure, sudden death) or infections (mostly pneumonia).105 106 n
- Observational studies suggest that conventional or first-generation antipsychotic agents also may increase mortality in such patients.101 105 106
- Antipsychotic agents, including chlorpromazine, are not approved for the treatment of dementia-related psychosis.101 105 106 n
Side effects include:
Extrapyramidal reactions (e.g., Parkinson-like symptoms, dystonia, akathisia, tardive dyskinesia), drowsiness, dizziness, skin reactions or rash, dry mouth, orthostatic hypotension, amenorrhea, galactorrhea, weight gain.
See also:
For healthcare professionals
Applies to chlorpromazine: compounding powder, injectable solution, oral capsule extended release, oral concentrate, oral syrup, oral tablet, rectal suppository.
General adverse events
The most frequently reported side effects included drowsiness, sedation, dry mouth, and nasal stuffiness.[Ref]
Hematologic
- Very common (10% or more): Mild leukopenia (up to 30%)
- Common (1% to 10%): Agranulocytosis, leukopenia, eosinophilia, hemolytic anemia, aplastic anemia, thrombocytopenia purpura, pancytopenia
- Uncommon (0.1% to 1%): Purpura, leukocytosis, coagulation defects[Ref]
Nervous system
- Common (1% to 10%): Hypertonia, tardive dyskinesia, tardive dystonia, extrapyramidal syndrome, akathisia, parkinsonism, motor restlessness, drowsiness, convulsion/convulsive seizures (petit mal and grand mal), lowering of the seizure threshold, acute dyskinesia or dystonia
- Uncommon (0.1% to 1%): Cerebral edema, epileptic fits, neuroleptic malignant syndrome, myasthenia gravis, abnormality of cerebrospinal fluid proteins
- Frequency not reported: Lethargy, akinesia, hyperkinesia, autonomic dysfunction, tremor, drooling, pill rolling motion, cogwheel rigidity, shuffling gait, rhythmical involuntary movements of the tongue/face/mouth/jaw, involuntary movements of the extremities, fine vermicular movements of the tongue, dizziness, headache, momentary fainting, pseudo-parkinsonism, mask-like facies
- Postmarketing reports: Cerebrovascular adverse events[Ref]
Acute dystonia and/or dyskinesia typically were transitory, occurring more frequently in children and young adults within the first 4 days of treatment or after dose changes.
Akathisia usually occurred after patients were given large initial doses.
Autonomic dysfunction occurred as a symptom of neuroleptic malignant syndrome.
Convulsive seizures have occurred more frequently in patients with a history of seizures and/or with EEG abnormalities.
Momentary fainting occurred most commonly in patients after the first injection, with a lower frequency of occurrence in subsequent injections; patients given oral formulations rarely fainted after the initial dose.
Parkinsonism more commonly occurred in adults and elderly patients after weeks to months of treatment.
Sedation and somnolence occurred more frequently at the start of treatment.[Ref]
Gastrointestinal
- Common (1% to 10%): Dry mouth, constipation, nausea, obstipation, adynamic ileus, atonic colon
- Uncommon (0.1% to 1%): Paralytic ileus
- Postmarketing reports: Ischemic colitis, intestinal perforation/fatal intestinal perforation, gastrointestinal (GI) necrosis/fatal GI necrosis, intestinal obstruction, tongue protrusion, difficulty swallowing, necrotizing colitis/fatal necrotizing colitis[Ref]
Psychiatric
- Common (1% to 10%): Anxiety, mental confusion, agitation, excitement, aggravation of schizophrenic symptoms
- Uncommon (0.1% to 1%): Nightmares, dysphoria, catatonic excitement, mental dulling/slowing
- Rare (0.01% to 0.1%): Psychotic symptoms, catatonic-like states
- Frequency not reported: Insomnia, altered mood, altered consciousness[Ref]
Altered consciousness occurred as a symptom of neuroleptic malignant syndrome.[Ref]
Ocular
- Common (1% to 10%): Blurred vision, photophobia, corneal/eye deposits, miosis and mydriasis
- Uncommon (0.1% to 1%): Optic atrophy, lens opacities, pigmentary retinopathy, precipitation/aggravation of narrow angle glaucoma
- Frequency not reported: Oculogyric crisis, ocular changes, accommodation disorder[Ref]
Accommodation disorder was related to anticholinergic effects of this drug.
Eye deposits occurred in the anterior segment of the eye from drug accumulation; however, the deposits usually did not have impact on sight.[Ref]
Genitourinary
- Common (1% to 10%): Urinary retention/hesitancy, priapism, ejaculation disorders/impotence
- Uncommon (0.1% to 1%): Amenorrhea, incontinence, lactation and moderate breast engorgement (female patients)
- Frequency not reported: Galactorrhea, oligomenorrhea, erectile dysfunction, female sexual arousal disorder[Ref]
Lactation and breast engorgement in female patients occurred with large doses.
Urinary retention was linked to anticholinergic effects of this drug.[Ref]
Dermatologic
- Common (1% to 10%): Contact dermatitis, photosensitivity/photosensitivity reaction, urticarial/maculopapular/petechial or edematous reaction
- Uncommon (0.1% to 1%): Skin pigmentation, exfoliative dermatitis, toxic epidermal necrolysis
- Frequency not reported: Allergic dermatitis, skin rashes
- Postmarketing reports: Angioneurotic edema[Ref]
Metabolic
- Common (1% to 10%): Impaired glucose tolerance, hyperglycemia, weight gain
- Uncommon (0.1% to 1%): Hypoglycemia, water retention
- Postmarketing reports: Hypertriglyceridemia, hyponatremia, increased appetite[Ref]
Cardiovascular
- Common (1% to 10%): Orthostatic/postural hypotension, ECG changes (electrocardiogram QT prolongation, ST depression, U-Wave and T-Wave changes)
- Uncommon (0.1% to 1%): Arrhythmias, hypertensive crisis, AV block, ventricular tachycardia/tachycardia, QT prolongation and fibrillation, edema, labile blood pressure
- Frequency not reported: Ventricular fibrillation, Torsade de pointes, cardiac arrest, sudden cardiac death, profound hypotension, peripheral edema, venous embolism, deep vein thrombosis, cardiac arrhythmias (including ventricular and atrial arrhythmias)[Ref]
Cardiac arrest may be related to dose as well as preexisting conditions (e.g., cardiac disease, old age, hypokalemia, concurrent tricyclic antidepressants).
Hypertensive crisis occurred after abrupt withdrawal of treatment.
Orthostatic hypotension occurred more frequently in elderly and/or volume depleted patients, and was more likely to occur with IM administration.
Sudden cardiac death may be related to causes of cardiac origin.[Ref]
Endocrine
- Common (1% to 10%): Hypothalamic effects, hyperprolactinemia/elevated prolactin levels
- Uncommon (0.1% to 1%): Gynecomastia, profuse sweating, false positive pregnancy tests, inappropriate antidiuretic hormone secretion[Ref]
Other
- Common (1% to 10%): Paradoxical reactions, impaired thermoregulation/temperature regulation disorder
- Uncommon (0.1% to 1%): Hyperthermia, hypothermia, malignant hyperpyrexia
- Frequency not reported: Sudden death, jitteriness, neonatal drug withdrawal syndrome[Ref]
Hyperthermia occurred as a symptom of neuroleptic malignant syndrome.
Mild fevers have occurred in patient who received large doses intramuscularly.
Sudden death may be related to causes of cardiac origin, asphyxia, convulsions, or hyperpyrexia.[Ref]
Respiratory
- Common (1% to 10%): Nasal congestion/stuffiness, respiratory depression
- Uncommon (0.1% to 1%): Dyspnea
- Frequency not reported: Bronchospasm, pulmonary embolism/fatal pulmonary embolism
- Postmarketing reports: Asthma, laryngeal edema, throat tightness, asphyxia (failure of the cough reflex)[Ref]
Local
- Common (1% to 10%): Injection site pain, injection abscess
- Uncommon (0.1% to 1%): Contact skin sensitization[Ref]
Contact sensitization has occurred in individuals who frequently handled this drug.[Ref]
Immunologic
- Common (1% to 10%): Positive systemic lupus erythematosus (SLE) cells, antinuclear antibody (ANA) positive/raised ANA titer[Ref]
Hepatic
- Common (1% to 10%): Cholestatic jaundice
- Uncommon (0.1% to 1%): Liver injury, fatal liver injury, cholestatic/hepatocellular or mixed liver injury
- Frequency not reported: Progressive hepatic fibrosis[Ref]
Musculoskeletal
- Uncommon (0.1% to 1%): Elevated creatine phosphokinase, muscular rigidity/rigidity, myoglobinuria/rhabdomyolysis
- Rare (0.01% to 0.1%): Systemic lupus erythematosus
- Frequency not reported: Torticollis, trismus
- Postmarketing reports: Prolonged, abnormal muscle contractions, neck muscle spasms[Ref]
Elevated creatine phosphokinase, muscular rigidity, and myoglobinuria/rhabdomyolysis are symptoms of neuroleptic malignant syndrome.
Rigidity occurred as a symptom of neuroleptic malignant syndrome.[Ref]
Renal
- Uncommon (0.1% to 1%): Glycosuria, acute renal failure[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Severe allergic reactions/allergic reactions
- Rare (0.01% to 0.1%): Anaphylactic/anaphylactoid reactions
- Frequency not reported: Angioedema[Ref]
References
1. (2002) "Product Information. Thorazine (chlorpromazine)." SmithKline Beecham
2. Cerner Multum, Inc. "UK Summary of Product Characteristics."
3. Cerner Multum, Inc. "Australian Product Information."
Frequently asked questions
More about chlorpromazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (71)
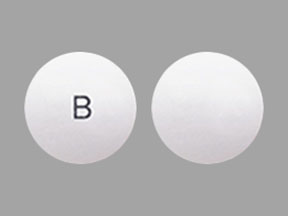
- Drug images
- Dosage information
- During pregnancy
- Drug class: phenothiazine antiemetics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
- ChlorproMAZINE monograph
- Chlorpromazine (FDA)
- Chlorpromazine Oral Concentrate (FDA)
- Chlorpromazine Tablets (FDA)
Related treatment guides
Further information
Chlorpromazine side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.