Sulfamethoxazole and Trimethoprim
Medically reviewed by Drugs.com. Last updated on Jul 29, 2024.
Pronunciation
(sul fa meth OKS a zole & trye METH oh prim)
Index Terms
- Cotrimoxazole
- Co-Trimoxazole
- Septra
- SMX-TMP
- SMZ-TMP
- Sulfamethoxazole-Trimethoprim
- Sulfamethoxazole/Trimethoprim
- Sulfatrim
- TMP-SMX
- TMP-SMZ
- Trimethoprim and Sulfamethoxazole
- Trimethoprim-Sulfamethoxazole
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Intravenous:
Generic: Sulfamethoxazole 80 mg and trimethoprim 16 mg per mL (5 mL, 10 mL, 30 mL)
Suspension, Oral:
Sulfatrim Pediatric: Sulfamethoxazole 200 mg and trimethoprim 40 mg per 5 mL (473 mL) [contains alcohol, usp, fd&c red #40, fd&c yellow #6 (sunset yellow), methylparaben, polysorbate 80, propylene glycol, propylparaben, saccharin sodium]
Sulfatrim Pediatric: Sulfamethoxazole 200 mg and trimethoprim 40 mg per 5 mL (473 mL [DSC]) [contains alcohol, usp, fd&c red #40, fd&c yellow #6 (sunset yellow), methylparaben, polysorbate 80, propylene glycol, propylparaben, saccharin sodium; cherry flavor]
Generic: Sulfamethoxazole 200 mg and trimethoprim 40 mg per 5 mL (20 mL, 473 mL)
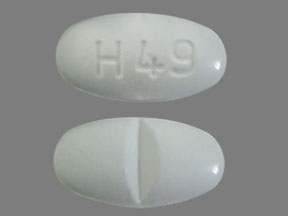
Tablet, Oral:
Bactrim: Sulfamethoxazole 400 mg and trimethoprim 80 mg [scored; contains sodium benzoate]
Bactrim DS: Sulfamethoxazole 800 mg and trimethoprim 160 mg [scored; contains sodium benzoate]
Generic: Sulfamethoxazole 400 mg and trimethoprim 80 mg, Sulfamethoxazole 800 mg and trimethoprim 160 mg
Related/similar drugs
prednisone, amoxicillin, doxycycline, ciprofloxacin, cephalexin, azithromycin, metronidazole
Brand Names: U.S.
- Bactrim
- Bactrim DS
- Sulfatrim Pediatric
Pharmacologic Category
- Antibiotic, Miscellaneous
- Antibiotic, Sulfonamide Derivative
Pharmacology
Sulfamethoxazole interferes with bacterial folic acid synthesis and growth via inhibition of dihydrofolic acid formation from para-aminobenzoic acid; trimethoprim inhibits dihydrofolic acid reduction to tetrahydrofolate resulting in sequential inhibition of enzymes of the folic acid pathway
Absorption
Oral: Rapid; almost completely (90% to 100%)
Distribution
Both SMX and TMP distribute to middle ear fluid, sputum, vaginal fluid; TMP also distributes into bronchial secretions
Vd: TMP:
Newborns: ~2.7 L/kg (range: 1.3 to 4.1 hours) (Springer 1982)
Infants: 1.5 L/kg (Hoppu 1989)
Children 1 to 10 years: 0.86 to 1 L/kg (Hoppu 1987)
Adults: ~1.3 L/kg (Hoppu 1987)
Metabolism
Hepatic, both to multiple metabolites; SMX to hydroxy (via CYP2C9) and acetyl derivatives, and also conjugated with glucuronide; TMP to oxide and hydroxy derivatives; the free forms of both SMX and TMP are therapeutically active
Excretion
Both are excreted in urine as metabolites and unchanged drug
Time to Peak
Serum: Oral: 1 to 4 hours
Half-Life Elimination
TMP: Prolonged in renal failure
Newborns: ~19 hours; range: 11 to 27 hours (Springer 1982)
Infants 2 months to 1 year: ~4.6 hours; range: 3 to 6 hours (Hoppu 1989)
Children 1 to 10 years: 3.7 to 5.5 hours (Hoppu 1987)
Children and Adolescents >10 years: 8.19 hours
Adults: 6 to 11 hours
SMX: 9 to 12 hours, prolonged in renal failure
Protein Binding
SMX: ~70%, TMP: ~44%
Special Populations: Renal Function Impairment
Patients with severely impaired renal function exhibit an increase in the half-lives of both components, requiring dosage adjustments.
Special Populations: Elderly
Total body clearance of trimethoprim was 19% lower in elderly patients.
Use: Labeled Indications
Oral: Treatment of urinary tract infections (UTIs) due to Escherichia coli, Klebsiella and Enterobacter spp, Morganella morganii, Proteus mirabilis, and Proteus vulgaris; acute otitis media; acute exacerbations of chronic obstructive pulmonary disease due to susceptible strains of Haemophilus influenzae or Streptococcus pneumoniae; treatment and prophylaxis of Pneumocystis pneumonia (PCP); traveler's diarrhea due to enterotoxigenic E. coli; treatment of shigellosis caused by Shigella flexneri or Shigella sonnei.
IV: Treatment of PCP; treatment of shigellosis caused by S. flexneri or S. sonnei; treatment of severe or complicated UTIs due to E. coli, Klebsiella and Enterobacter spp, M. morganii, P. mirabilis, and P. vulgaris.
Off Label Uses
Bite wound infection, prophylaxis or treatment (animal or human bite)
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTI), sulfamethoxazole/trimethoprim, in combination with an appropriate agent for anaerobic coverage, is an effective and recommended alternative for the prophylaxis and treatment of animal bite wounds.
Clinical experience suggests the utility of sulfamethoxazole/trimethoprim as an alternative agent for the prophylaxis and treatment of human bite wounds [Baddour 2019a], [Baddour 2019b].
Cyclosporiasis
Data from a randomized, double-blind, placebo-controlled trial in immunocompetent patients [Hoge 1995] and a prospective cohort study in patients with HIV [Pape 1994] support the use of sulfamethoxazole/trimethoprim in the treatment of cyclosporiasis.
Based on the Centers for Disease Control and Prevention (CDC) recommendations for the treatment for cyclosporiasis, sulfamethoxazole/trimethoprim is the preferred treatment for cyclosporiasis (immunocompetent or HIV-infected patients).
Cystitis, uncomplicated, prophylaxis for recurrent infection
Data from a limited number of clinical trials of continuous prophylaxis and postcoital prophylaxis suggest that sulfamethoxazole/trimethoprim may be beneficial in the prophylaxis of recurrent uncomplicated cystitis [Stamm 1980], [Stapleton 1990].
Based on the American Urological Association/Canadian Urological Association/Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction guidelines for recurrent uncomplicated urinary tract infections in women, sulfamethoxazole/trimethoprim is an effective and recommended agent and may be considered for prophylaxis of recurrent uncomplicated cystitis in nonpregnant women [AUA/CUA/SUFU [Anger 2019]].
Cystoisosporiasis (Isosporiasis)
Based on the US Department of Health and Human Services (HHS) guidelines for prevention and treatment of opportunistic infections in adults and adolescents with HIV, sulfamethoxazole/trimethoprim is an effective and recommended agent for treatment or chronic suppressive therapy (secondary prophylaxis) of Isospora belli infection in adolescent and adult patients with HIV.
Based on the CDC recommendations for the treatment for cystoisosporiasis, sulfamethoxazole/trimethoprim is the preferred treatment for Cystoisospora belli (Isospora belli) in immunocompetent (when treatment is indicated) or immunosuppressed patients (expert consultation is recommended).
Diabetic foot infection
According to the IDSA clinical practice guideline for the diagnosis and treatment of diabetic foot infections, sulfamethoxazole/trimethoprim is a reasonable treatment option for mild diabetic foot infections.
Epididymitis
Clinical experience suggests that sulfamethoxazole/trimethoprim is an alternative agent for the treatment of epididymitis [Eyre 2019].
Granuloma inguinale (Donovanosis)
Based on the CDC sexually transmitted diseases treatment guidelines, sulfamethoxazole/trimethoprim is an effective and recommended alternative agent in the treatment of granuloma inguinale.
Intracranial abscess (brain abscess, intracranial epidural abscess) and spinal epidural abscess (methicillin-resistant Staphylococcus aureus)
IDSA guidelines cite limited data evaluating the effectiveness of sulfamethoxazole/trimethoprim in the treatment of brain abscess and spinal epidural abscess caused by methicillin-resistant Staphylococcus aureus (MRSA). However, the guidelines support the initial use and evaluation of vancomycin treatment; if vancomycin is contraindicated or resistance is expected, use of linezolid or sulfamethoxazole/trimethoprim should be considered as alternative therapy. Sulfamethoxazole/trimethoprim can be given as a single agent or in combination with rifampin [IDSA [Liu 2011]].
Clinical experience also suggests the utility of sulfamethoxazole/trimethoprim as an alternative agent for MRSA intracranial epidural abscess [Sexton 2019a].
Melioidosis (Burkholderia pseudomallei) infection
An HHS Workshop on treatment of and postexposure prophylaxis for Burkholderia pseudomallei and B. mallei infection suggests the use of sulfamethoxazole/trimethoprim as a potential addition to initial intensive therapy (with ceftazidime or a carbapenem) in focal disease of the CNS, prostate, bone, or other deep-seated infection, and as eradication therapy (initiated after completion of initial intensive therapy) [Lipsitz 2012].
Meningitis, bacterial
Based on the IDSA guidelines for the management of bacterial meningitis and health care-associated ventriculitis and meningitis, sulfamethoxazole/trimethoprim is an effective and recommended alternative agent for the treatment of meningitis due to MRSA, Listeria monocytogenes, E. coli, and other susceptible Enterobacteriaceae.
Nocardiosis
Data from a limited number of patients studied suggest that sulfamethoxazole/trimethoprim may be beneficial for the treatment of nocardiosis (as monotherapy or combination therapy, depending on severity of infection) [Wang 2015].
Clinical experience also suggests the utility of sulfamethoxazole/trimethoprim in the treatment of nocardiosis [Lerner 1996], [Spelman 2019b].
Osteomyelitis
According to IDSA guidelines, sulfamethoxazole/trimethoprim, in combination with rifampin, is a reasonable treatment option for MRSA osteomyelitis [IDSA [Liu 2011]].
Peritonitis, spontaneous bacterial (prevention)
Data from controlled trials support use of sulfamethoxazole/trimethoprim as primary long-term prophylaxis in cirrhotic patients with low protein ascites or as secondary long-term prophylaxis in patients who have experienced a prior spontaneous bacterial peritonitis (SBP) episode [Alvarez 2005], [Lontos 2014], [Singh 1995].
Based on American Association for the Study of Liver Diseases guidelines on the management of adult patients with ascites due to cirrhosis, sulfamethoxazole/trimethoprim is recommended for long-term prophylaxis in patients who have experienced a prior SBP episode and as primary prophylaxis in cirrhotic patients with low protein ascites. Increasing bacterial resistance rates to antibiotics used in the treatment and prevention of SBP have been documented; therefore, local epidemiological patterns should be considered, and use of antibiotic prophylaxis should be restricted to patients at high risk of SBP [AASLD [Runyon 2012]].
Prostatitis
Data from open-label, non-comparative studies suggest the utility of sulfamethoxazole/trimethoprim in the treatment of chronic bacterial prostatitis [Dow 1975], [Meares 1975]. In addition, clinical experience suggests the utility of sulfamethoxazole/trimethoprim in the treatment of acute and chronic bacterial prostatitis [Lipsky 2010].
Prosthetic joint infection
Data from a limited number of patients in a prospective, consecutive, therapeutic case series with no control group suggest that sulfamethoxazole/trimethoprim may be beneficial for the treatment of prosthetic joint infection [Cordero-Ampuero 2007]. Additional data may be necessary to further define the role of sulfamethoxazole/trimethoprim in the treatment of this condition.
Based on the IDSA clinical practice guideline for the diagnosis and management of prosthetic joint infection, sulfamethoxazole/trimethoprim is an effective and recommended agent for treatment and chronic oral antimicrobial suppression of prosthetic joint infection due to staphylococci (methicillin-resistant) or Enterobacteriaceae, after completion of pathogen-specific parenteral therapy in patients undergoing 1-stage exchange or debridement with retention of prosthesis.
Q fever (Coxiella burnetii)
Based on the CDC diagnosis and management of Q fever guidelines, sulfamethoxazole/trimethoprim given for the treatment of Q fever (Coxiella burnetii) is effective and recommended in the management of this condition in pregnant women up to 32 weeks' gestation (alternative agent in nonpregnant adults).
Septic arthritis (methicillin-resistant Staphylococcus aureus)
Based on the IDSA guidelines for the treatment of MRSA infections in adults and children, sulfamethoxazole/trimethoprim is an effective and recommended treatment option for septic arthritis without prosthetic material caused by MRSA following initial therapy with an appropriate IV antibiotic.
Skin and soft tissue infections
Data from a limited number of patients studied suggest that sulfamethoxazole/trimethoprim may be beneficial for the treatment of uncomplicated skin infections caused by streptococci [Miller 2015].
Clinical experience also suggests the utility of sulfamethoxazole/trimethoprim as an alternative agent in the treatment of mild skin and soft tissue infections (including impetigo and erysipelas) caused by streptococci [Baddour 2019c], [Bowen 2017], [Spelman 2019a].
Based on the IDSA guidelines for the diagnosis and management of SSTIs and the treatment of MRSA infections in adults and children, sulfamethoxazole/trimethoprim is an effective and recommended treatment option for mild to moderate SSTIs caused by MRSA.
Stenotrophomonas maltophilia infections
Data from a limited number of patients studied suggest that sulfamethoxazole/trimethoprim may be beneficial for the treatment of Stenotrophomonas maltophilia infections [Wang 2014].
Clinical experience also suggests the utility of sulfamethoxazole/trimethoprim in the treatment of Stenotrophomonas maltophilia [Looney 2009].
Toxoplasma gondii encephalitis (prophylaxis/treatment/chronic maintenance) in patients with HIV
Based on the HHS guidelines for prevention and treatment of opportunistic infections in adults and adolescents with HIV, sulfamethoxazole/trimethoprim is an effective and recommended agent for primary prophylaxis of Toxoplasma gondii encephalitis and is an effective and recommended alternative agent for the treatment of or as chronic maintenance therapy of T. gondii encephalitis in HIV-infected patients.
Contraindications
Hypersensitivity to any sulfa drug, trimethoprim, or any component of the formulation; history of drug induced-immune thrombocytopenia with use of sulfonamides or trimethoprim; megaloblastic anemia due to folate deficiency; infants <2 months (manufacturer's labeling), infants <4 weeks (CDC 2009); marked hepatic damage or severe renal disease (if patient not monitored); concomitant administration with dofetilide
Note: Although the FDA approved product labeling states this medication is contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See “Warnings/Precautions” for more detail.
Canadian labeling: Additional contraindications (not in US labeling): Blood dyscrasias; pregnancy; breastfeeding; premature infants; acute porphyria.
Dosing: Adult
Note: Weight-based dosing recommendations are based on the trimethoprim (TMP) component. Each double-strength tablet contains TMP 160 mg and sulfamethoxazole (SMX) 800 mg. Each single-strength tablet contains TMP 80 mg and SMX 400 mg. The undiluted IV solution contains TMP 16 mg per mL and SMX 80 mg per mL. IV solutions must be diluted in D5W prior to use. Diluted IV solutions have limited stability and can precipitate unpredictably; refer to a detailed IV compatibility reference.
General dosing guidelines:
Oral: 1 to 2 double-strength tablets every 12 to 24 hours. Note: Serum creatinine and potassium concentrations should be monitored in outpatients receiving high-dose therapy (>5 mg/kg/day [TMP component]) (Gentry 2013).
IV: 8 to 20 mg/kg/day (TMP component) divided every 6 to 12 hours.
Bite wound infection, prophylaxis or treatment (animal or human bite) (alternative agent) (off-label use): Oral: 1 double-strength tablet twice daily; in combination with an appropriate agent for anaerobic coverage. Duration of therapy for prophylaxis is 3 to 5 days (IDSA [Stevens 2014]); duration of therapy for established infection is typically 5 to 14 days (Baddour 2019a; Baddour 2019b).
Chronic obstructive pulmonary disease, acute exacerbation (alternative agent): Note: Avoid use in patients with risk factors for Pseudomonas infection or poor outcomes (eg, ≥65 years of age with major comorbidities, FEV1 <50% predicted, frequent exacerbations) (Sethi 2020).
Oral: 1 double-strength tablet every 12 hours for 3 to 7 days (GOLD 2020; Sethi 2020; manufacturer's labeling).
Diabetic foot infection, mild (methicillin-resistant Staphylococcus aureus) (off-label use): Oral: 2 double-strength tablets twice daily, usually for 1 to 2 weeks (IDSA [Lipsky 2012]; Lipsky 2004). Note: When used as empiric therapy, must be used in combination with other appropriate agents. Some experts also use this agent for selected moderate infections (Lipsky 2012).
Diarrhea, infectious:
Cyclosporiasis (off-label use):
Immunocompromised (AIDS-associated): Limited data available: Oral: 1 double-strength tablet twice daily for 14 days, followed by secondary prophylaxis with 1 double-strength tablet 3 times weekly (Pape 1994; Weller 2019).
Immunocompetent: Oral: 1 double-strength tablet twice daily for 7 to 10 days (CDC 2013; Hoge 1995).
Cystoisosporiasis (isosporiasis) (off-label use):
Immunocompromised (AIDS-associated): Oral, IV: 160 mg (TMP component) twice daily for 7 to 10 days; if symptoms worsen or persist, may increase dose to 160 mg (TMP component) 4 times daily and/or prolong duration to 21 to 28 days. In patients with CD4 <200 cells/mm3, follow treatment with secondary prophylaxis of one double-strength tablet orally 3 times weekly (HHS [OI adult 2020]).
Immunocompetent (usually self-limited; treatment not always indicated): Oral: 1 double-strength tablet twice daily for 7 to 10 days (CDC 2013).
Shigellosis (widespread resistance [alternative agent if susceptibility is documented]): Oral: 1 double-strength tablet twice daily for 5 to 7 days (Agha 2020).
Intracranial abscess (brain abscess, intracranial epidural abscess) and spinal epidural abscess (alternative agent for methicillin-resistant S. aureus) (off-label use): IV: 5 mg/kg/dose (TMP component) every 8 to 12 hours (IDSA [Liu 2011]; Sexton 2019a; Sexton 2019b; Southwick 2019). Duration generally ranges from 4 to 8 weeks for brain abscess and spinal epidural abscess and 6 to 8 weeks for intracranial epidural abscess (Sexton 2019a; Sexton 2019b; Southwick 2019).
Melioidosis (Burkholderia pseudomallei) infection (off-label use):
Initial intensive therapy (as a potential add-on to primary therapy [ceftazidime or a carbapenem] in focal disease of the CNS, prostate, bone, joint, skin, or soft tissue): Oral, IV:
40 to 60 kg: 240 mg (TMP component) twice daily (Currie 2019).
>60 kg: 320 mg (TMP component) twice daily (Currie 2019).
Eradication therapy (begin after completion of initial intensive therapy): Oral:
40 to 60 kg: 240 mg (TMP component) twice daily (Lipsitz 2012).
>60 kg: 320 mg (TMP component) twice daily (Lipsitz 2012).
Meningitis, bacterial (alternative agent for methicillin-resistant S. aureus, L. monocytogenes, E. coli, and other Enterobacteriaceae) (off-label use): IV: 5 mg/kg/dose (TMP component) every 6 to 12 hours (IDSA [Tunkel 2004]; IDSA [Tunkel 2017]). Note: Some experts prefer 5 mg/kg/dose (TMP component) every 8 hours (Hasbun 2019).
Nocardiosis (off-label use): Limited data available to guide treatment. Due to concerns for resistance, susceptibility testing should be performed on isolates (CDC 2017).
Cutaneous infections (superficial; no other organ involvement): Oral: 5 to 10 mg/kg/day (TMP component) in 2 divided doses (Spelman 2019b).
Pulmonary infection (mild to moderate):
Immunocompetent patients: Oral: 5 to 10 mg/kg/day (TMP component) in 2 divided doses (Spelman 2019b).
Immunocompromised patients: Oral: 15 mg/kg/day (TMP component) in 3 to 4 divided doses (Spelman 2019b).
Pulmonary infection (severe), CNS, disseminated, or multi-site infection: IV: 15 mg/kg/day (TMP component) in 3 to 4 divided doses (Spelman 2019b). Note: When used as empiric therapy, must be used in combination with 1 to 2 additional agents. Consult an infectious diseases specialist for specific treatment recommendations.
Duration: Prolonged treatment is required (range: 3 months to ≥1 year [combined parenteral/oral therapy]) (Spelman 2019b).
Osteomyelitis due to methicillin-resistant S. aureus (alternative agent) (off-label use): Oral, IV: 4 mg/kg/dose (TMP component) every 12 hours with rifampin (IDSA [Liu 2011]).
Peritonitis, spontaneous bacterial (prevention) (off-label use):
High-risk patients (eg, hospitalized patients with Child-Pugh class B or C cirrhosis and active GI bleeding): Oral: 1 double-strength tablet twice daily (Runyon 2019).
Long-term secondary SBP prophylaxis: Oral: 1 double-strength tablet once daily (Runyon 2019).
Pneumocystis pneumonia:
Prophylaxis, primary and secondary:
Patients with HIV: Oral: 1 double-strength tablet once daily or 1 single-strength tablet once daily (preferred regimens) or 1 double-strength tablet 3 times weekly (alternative regimen). Note: In patients also requiring prophylaxis for toxoplasmosis, 1 double-strength tablet once daily should be used (HHS [OI adult 2020]).
Duration in patients with HIV receiving ART: Continue until undetectable viral load and CD4 count >200 cells/mm3 for >3 months (HHS [OI adult 2020]); some experts discontinue primary prophylaxis in patients with CD4 counts between 100 and 200 cells/mm3 who are receiving ART and have had an undetectable viral load for ≥3 to 6 months (COHERE 2010; HHS [OI adult 2020]).
Immunocompromised host, HIV-uninfected (eg, transplant recipients, cancer-related, hematopoietic stem cell transplant [HSCT]): Oral: 1 double-strength tablet once daily or 1 single-strength tablet once daily (preferred regimens); alternatively, 1 double-strength tablet 3 times weekly (Fishman 2001; Montoya 2001; Tomblyn 2009).
Duration after solid organ transplant (except lung): ≥6 to 12 months and during periods of increased immunosuppression (eg, treatment for acute rejection) (Fishman 2019; Martin 2013).
Duration after lung transplant: Lifelong therapy should be considered (Martin 2013; Palmer 2019).
Duration for cancer-related (including HSCT) in patients at high risk for PCP infection: Based on expert opinion, continue until risk factor(s) for PCP infection are no longer present (Neumann 2013, Thomas 2017). Consult other specialized databases for more detailed information.
Treatment (HHS [OI adult 2020]; ATS [Limper 2011]; Thomas 2017): Note: Secondary prophylaxis should be initiated immediately upon completion of therapy.
Moderate to severe infection: IV: 15 to 20 mg/kg/day (TMP component) in 3 or 4 divided doses for 21 days; may switch to oral therapy after clinical improvement. Note: Patients with moderate or severe infection (PaO2 <70 mm Hg at room air or alveolar-arterial oxygen gradient ≥35 mm Hg) should receive adjunctive glucocorticoids.
Mild to moderate infection: Oral: 15 to 20 mg/kg/day (TMP component) in 3 divided doses for 21 days or two double-strength tablets 3 times daily.
Prostatitis (off-label use):
Acute bacterial prostatitis: Oral: 1 double-strength tablet twice daily for 4 to 6 weeks (Lipsky 2010; Meyrier 2019a).
Chronic bacterial prostatitis (alternative agent): Oral: 1 double-strength tablet twice daily for ≥6 weeks (Lipsky 2010; Meares 1975; Meyrier 2019b).
Prosthetic joint infection (off-label use): Oral continuation therapy for methicillin-resistant S. aureus and Enterobacteriaceae (following pathogen-specific IV therapy in patients undergoing 1-stage exchange or debridement with retention of prosthesis):
Oral: 1 double-strength tablet twice daily. For S. aureus infections, combine with rifampin (Berbari 2019; IDSA [Osmon 2013]). Duration is a minimum of 3 months, depending on patient-specific factors (Berbari 2019).
Q fever (C. burnetii) (preferred agent for pregnant women ≤32 weeks of gestation; alternative agent for non-pregnant adults) (off-label use): Oral: Acute illness: 1 double-strength tablet twice daily during pregnancy but not beyond 32 weeks' gestation; administer with folic acid supplementation. Note: Discontinue therapy for the final 8 weeks of pregnancy due to hyperbilirubinemia risk (CDC [Anderson 2013]).
Septic arthritis (without prosthetic material) due to methicillin-resistant S. aureus (alternative agent following initial IV therapy with an appropriate antibiotic) (off-label use): Oral: 2 double-strength tablets twice daily or 4 mg/kg/dose (TMP component) twice daily (maximum: 320 mg [TMP component]/dose) for completion of 3- to 4-week total treatment course (IV and oral) (Goldenberg 2019; IDSA [Liu 2011]).
Sexually transmitted infections:
Epididymitis in patients ≥35 years of age and who are at low risk for sexually transmitted infections (ie, likely to be caused by enteric organisms) (alternative agent) (off-label use): Oral: 1 double-strength tablet twice daily for 10 days (Eyre 2019).
Granuloma inguinale (donovanosis) (alternative agent) (off-label use): Oral: 1 double-strength tablet every 12 hours for at least 3 weeks and until lesions have healed (CDC [Workowski 2015]). Note: If symptoms do not improve within the first few days of therapy, another agent (eg, aminoglycoside) can be added (CDC [Workowski 2015]).
Skin/soft tissue infection, mild to moderate (outpatient treatment) (off-label use): Oral: 1 to 2 double-strength tablets twice daily (IDSA [Liu 2011]; IDSA [Stevens 2014]; Miller 2015); treat for 5 to 14 days depending on severity and clinical response (IDSA [Stevens 2014]; Spelman 2019a). Note: For empiric therapy of purulent cellulitis, monotherapy with sulfamethoxazole/trimethoprim is appropriate. For empiric therapy of nonpurulent cellulitis, guidelines suggest an additional agent (eg, amoxicillin, cephalexin) for beta-hemolytic streptococci (IDSA [Liu 2011]; IDSA [Stevens 2014]). However, limited data suggest that sulfamethoxazole and trimethoprim is an effective alternative agent for treatment of nonpurulent cellulitis (Bowen 2017; Miller 2015).
Stenotrophomonas maltophilia infections (hospital-acquired or ventilator-associated pneumonia, bacteremia, or other sites) (off-label use): IV: 15 mg/kg/day (TMP component) in 3 or 4 divided doses. Duration depends on site of infection; 14 days for bacteremia and 7 days for pneumonia in an immunocompetent host with evidence of clinical improvement (Lewis 2019; Looney 2009).
Toxoplasma gondii encephalitis (AIDS associated) (off-label use):
Primary prophylaxis: Oral: 1 double-strength tablet once daily (preferred) or 1 double-strength tablet 3 times weekly or 1 single-strength tablet once daily; primary prophylaxis is indicated for T. gondii IgG-positive patients with CD4 count <100 cells/mm3. Continue primary prophylaxis following initiation of ART until CD4 count >200 cells/mm3 for >3 months; some experts discontinue primary prophylaxis in patients with a CD4 count between 100 to 200 cells/mm3 who are receiving ART and have had an undetectable viral load for ≥3 to 6 months (HHS [OI adult 2020]).
Treatment (alternative agent): Oral, IV: 10 mg/kg/day (TMP component) in 2 divided doses for at least 6 weeks; longer duration may be needed if clinical or radiologic disease is extensive or response is incomplete at 6 weeks (HHS [OI adult 2020]).
Secondary prophylaxis (chronic maintenance therapy) (alternative agent): Oral: 1 double-strength tablet twice daily or, alternatively, 1 double-strength tablet once daily (lower dose may be associated with increased relapse risk). Continue following initiation of ART until CD4 count >200 cells/mm3 for >6 months (HHS [OI adult 2020]).
Urinary tract infection: Note: Uncomplicated urinary tract infection (UTI) has traditionally been defined as infection in an otherwise healthy nonpregnant female with a normal urinary tract; UTI in other patient populations has been considered complicated. Some experts instead categorize UTI as either acute simple cystitis (mild infection limited to the bladder with no signs/symptoms of upper tract or systemic infection in a nonpregnant adult) or complicated UTI (pyelonephritis or cystitis symptoms with other signs/symptoms of systemic infection) (Hooton 2019a; Hooton 2019b).
Acute uncomplicated or simple cystitis: Note: Avoid use if resistance prevalence is known to exceed 20% or if patient has risk factors for multidrug resistant gram-negative infection (Hooton 2019a; Hooton 2019b):
Oral: 1 double-strength tablet twice daily; treat females for 3 days (Hooton 2019a; IDSA [Gupta 2011]) and males for 7 days (Hooton 2019b).
Cystitis, uncomplicated, prophylaxis for recurrent infection (off-label use): Note: Prophylaxis may be considered in nonpregnant women with bothersome, recurrent uncomplicated cystitis despite nonantimicrobial preventative measures. The optimal duration of treatment has not been established; duration ranges from 3 to 12 months, with periodic assessment and monitoring (AUA/CUA/SUFU [Anger 2019]; Hooton 2019c).
Continuous prophylaxis: Oral: One-half of a single-strength tablet once daily or 3 times weekly (AUA/CUA/SUFU [Anger 2019]; Stamm 1980).
Postcoital prophylaxis: Females with cystitis temporally related to sexual intercourse: Oral: One-half to 1 single-strength tablet as a single dose immediately before or after sexual intercourse (AUA/CUA/SUFU [Anger 2019]; Stapleton 1990).
Urinary tract infection, complicated (including pyelonephritis) (outpatient targeted therapy [if the isolate is known to be susceptible]):
Oral: 1 double-strength tablet twice daily for 14 days (IDSA [Gupta 2011]); for women who have a rapid response to treatment, some experts treat for 7 to 10 days (Hooton 2019d). Note: Oral therapy should follow appropriate parenteral therapy. For outpatient treatment of mild infection, a single dose of a long-acting parenteral agent is acceptable prior to oral therapy; for outpatients who are more ill or are at risk for more severe illness, consider continuing parenteral therapy until culture and susceptibility results are available (Hooton 2019d; IDSA [Gupta 2011]).
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosage recommendations are based on the trimethoprim (TMP) component:
General dosing, susceptible infection: Infants ≥2 months, Children, and Adolescents: Oral, IV: 6 to 12 mg TMP/kg/day in divided doses every 12 hours; maximum single dose: 160 mg TMP/dose (Red Book [AAP 2015])
Catheter (peritoneal dialysis); exit-site or tunnel infection: Limited data available: Infants, Children, and Adolescents: Oral: 5 to 10 mg TMP/kg/dose once daily; maximum dose: 80 mg TMP/dose (ISPD [Warady 2012])
Cyclosporiasis: Limited data available: Infants ≥2 months, Children, and Adolescents: Oral: 8 to 10 mg TMP/kg/day in divided doses twice daily for 7 to 10 days; maximum single dose: 160 mg TMP (Red Book [AAP 2015])
Meningitis: Infants ≥2 months, Children, and Adolescents: IV: 10 to 20 mg TMP/kg/day divided every 6 to 12 hours for 7 to 21 days; duration dependent on the pathogen and clinical course (Tunkel 2004)
MRSA, community-acquired mild to moderate skin/soft tissue infection: Infants ≥2 months, Children, and Adolescents: Oral: 8 to 12 mg TMP/kg/day in divided doses every 12 hours (Liu 2011); alternatively, use of 20 mg TMP/kg/day in divided doses every 6 hours has been reported (Long 2012). If using empirically, consider addition of group A streptococcal coverage.
Otitis media, acute: Infants ≥2 months, Children, and Adolescents: Oral: 6 to 10 mg TMP/kg/day in divided doses every 12 hours for 10 days. Note: Due to resistance of S. pneumoniae, should not be used in patients that fail first-line amoxicillin therapy (AAP [Lieberthal 2013]).
Pneumocystis jirovecii pneumonia (PCP) (HIV-exposed/-positive):
Prophylaxis:
Infants (at least 4 weeks of age) and Children: Oral: 5 to 10 mg TMP/kg/day or 150 mg TMP/m2/day; dose may be given as a single daily dose or in divided doses every 12 hours given 2 to 3 days per week on consecutive days or alternating days; maximum daily dose: TMP 320 mg/day (HHS [OI pediatric 2016])
Adolescents: Oral: 80 to 160 mg TMP daily or alternatively, 160 mg TMP 3 times weekly (HHS [OI adult 2017]):
Treatment:
Infants >2 months and Children: Initial: IV: 15 to 20 mg TMP/kg/day in divided doses every 6 hours for 21 days; as acute pneumonitis subsides in patients with mild to moderate disease and no malabsorption issues nor diarrhea, may transition to oral therapy of same daily dose (15 to 20 mg/kg/day TMP) administered in divided doses 3 or 4 times daily (HHS [OI pediatric 2016])
Adolescents (HHS [OI adult 2017]):
Mild to moderate: Oral: 15 to 20 mg TMP/kg/day in 3 divided doses for 21 days or alternatively, 320 mg TMP 3 times daily for 21 days
Moderate to severe: Initial: IV: 15 to 20 mg TMP/kg/day in 3 to 4 divided doses for 21 days; may switch to oral after clinical improvement
Q-Fever (Coxiella burnetii); mild infection (doxycycline therapeutic failure): Limited data available, dose should be based on severity of illness: Children <8 years: Oral: Usual dose range: 8 to 10 mg TMP/kg/day in divided doses twice daily for 14 days; a wider dose range of 4 to 20 mg TMP/kg/day divided twice daily has been suggested to address varying degrees of severity; however, reported pediatric efficacy experience (eg, case series) are lacking; monitor patients receiving doses at the high and low end of the range closely for efficacy and possible adverse effects (Bradley 2017; CDC 2013)
Shigellosis: Infants ≥2 months, Children, and Adolescents: Note: Due to reported widespread resistance empiric therapy with sulfamethoxazole and trimethoprim is not recommended (CDC-NARMS 2010; WHO 2005)
Oral:
Manufacturer's labeling: 8 mg TMP/kg/day in divided doses every 12 hours for 5 days; maximum single dose: 160 mg TMP
Alternate dosing: IDSA recommendations for infectious diarrhea: 10 mg TMP/kg/day in divided doses every 12 hours for 3 days (for immunocompetent patients) or 7 to 10 days (for immunocompromised patients); maximum single dose: 160 mg TMP (Guerrant 2001)
IV: 8 to 10 mg TMP/kg/day in divided doses every 6, 8, or 12 hours for up to 5 days
Toxoplasmosis (HIV-exposed/infected):
Prophylaxis, primary:
Infants ≥2 months and Children: Oral: 150 mg TMP/m2/day; dose may be administered as a single daily dose (preferred) or in divided doses every 12 hours; alternatively, may also be given 3 times weekly for 3 consecutive or alternating days (HHS [OI pediatric 2016])
Adolescents: Oral: 160 mg TMP daily (preferred) or 160 mg TMP 3 times weekly or 80 mg TMP daily (HHS [OI adult 2017])
Treatment, encephalitis: Adolescents: Oral, IV: 10 mg/kg/day TMP in two divided doses for at least 6 weeks; longer duration may be required in some patients; following treatment all patients should receive chronic maintenance therapy daily (HHS [OI adult 2017])
Secondary prophylaxis (chronic suppressive therapy, alternative regimen): Note: Only use when pyrimethamine is unavailable or not tolerated:
Infants and Children: Oral: 150 mg TMP/m2/day once daily (HHS [OI pediatric 2016])
Adolescents: Maintenance therapy; postencephalitis treatment: Oral: 160 mg TMP once or twice daily: May discontinue when asymptomatic and CD4 count >200 cells/mm3 for >6 months in response to ART. Note: Once-daily dosing may be associated with an increased risk of relapse; if used, a gradual transition (eg, follow acute treatment with 4 to 6 weeks of 160 mg TMP twice daily before lowering to once-daily dosing) may be beneficial (HHS [OI adult 2017])
Urinary tract infection:
Treatment:
Oral:
Infants and Children 2 to 24 months: 6 to 12 mg TMP/kg/day in divided doses every 12 hours for 7 to 14 days (AAP 2011)
Children >24 months and Adolescents: 8 mg TMP/kg/day in divided doses every 12 hours for 3 days; longer duration may be required in some patients; maximum single dose: 160 mg TMP
IV: Infants ≥2 months, Children, and Adolescents: 8 to 10 mg TMP/kg/day in divided doses every 6, 8, or 12 hours for up to 14 days with serious infections
Prophylaxis: Infants ≥2 months, Children, and Adolescents: Oral: 2 mg TMP/kg/dose once daily (Mattoo 2007; Red Book [AAP 2012])
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Reconstitution
IV: Must dilute well in D5W prior to administration (ie, 1:15 to 1:25, which equates to 5 mL of drug solution diluted in 75-125 mL base solution)
Administration
IV: Infuse diluted solution over 60 to 90 minutes (administration over 30 to 60 minutes has also been described [Septra Canadian product monograph]); not for IM injection.
Oral: Administer without regard to meals. Administer with at least 8 ounces of water.
Dietary Considerations
Should be taken with 8 oz of water. May be taken without regard to meals.
Storage
Injection: Store at room temperature; do not refrigerate. Less soluble in more alkaline pH. Solution must be diluted prior to administration. Following dilution, store at room temperature; do not refrigerate. Manufacturer recommended dilutions and stability of parenteral admixture at room temperature (25°C):
5 mL/125 mL D5W; stable for 6 hours.
5 mL/100 mL D5W; stable for 4 hours.
5 mL/75 mL D5W; stable for 2 hours.
Studies have also confirmed limited stability in NS; detailed references should be consulted.
Suspension, tablet: Store at controlled room temperature of 15°C to 25°C (59°F to 77°F). Protect from light.
Drug Interactions
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Amantadine: Trimethoprim may enhance the adverse/toxic effect of Amantadine. Specifically, the risk of myoclonus and/or delirium may be increased. Amantadine may increase the serum concentration of Trimethoprim. Trimethoprim may increase the serum concentration of Amantadine. Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amodiaquine: Trimethoprim may enhance the neutropenic effect of Amodiaquine. Trimethoprim may increase the serum concentration of Amodiaquine. Avoid combination
Androgens: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Monitor therapy
Angiotensin II Receptor Blockers: Trimethoprim may enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Trimethoprim may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
AzaTHIOprine: Sulfamethoxazole may enhance the myelosuppressive effect of AzaTHIOprine. Monitor therapy
AzaTHIOprine: Trimethoprim may enhance the myelosuppressive effect of AzaTHIOprine. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Chloroprocaine: May diminish the therapeutic effect of Sulfonamide Antibiotics. Management: Avoid concurrent use of chloroprocaine and systemic sulfonamide-based antimicrobials whenever possible. Consider therapy modification
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
CycloSPORINE (Systemic): Sulfonamide Antibiotics may enhance the nephrotoxic effect of CycloSPORINE (Systemic). Sulfonamide Antibiotics may decrease the serum concentration of CycloSPORINE (Systemic). Monitor therapy
Dapsone (Systemic): Trimethoprim may increase the serum concentration of Dapsone (Systemic). Dapsone (Systemic) may increase the serum concentration of Trimethoprim. Monitor therapy
Dapsone (Topical): Trimethoprim may enhance the adverse/toxic effect of Dapsone (Topical). More specifically, trimethoprim may increase the risk for hemolysis Monitor therapy
Dexketoprofen: May enhance the adverse/toxic effect of Sulfonamides. Monitor therapy
Digoxin: Trimethoprim may increase the serum concentration of Digoxin. Monitor therapy
Dofetilide: Trimethoprim may increase the serum concentration of Dofetilide. Avoid combination
Eplerenone: Trimethoprim may enhance the hyperkalemic effect of Eplerenone. Monitor therapy
Fexinidazole [INT]: May increase the serum concentration of Products Containing Propylene Glycol. Avoid combination
Fosphenytoin: May decrease the serum concentration of Trimethoprim. Trimethoprim may increase the serum concentration of Fosphenytoin. Management: Consider alternatives to this combination when possible, to avoid potential decreased trimethoprim efficacy and increased phenytoin concentrations/effects. Monitor patients receiving this combination closely for both of these possible effects. Consider therapy modification
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
LamiVUDine: Trimethoprim may increase the serum concentration of LamiVUDine. Monitor therapy
Leucovorin Calcium-Levoleucovorin: May diminish the therapeutic effect of Trimethoprim. Management: Avoid concurrent use of leucovorin or levoleucovorin with trimethoprim (plus sulfamethoxazole) for Pneumocystis jirovecii pneumonia. If trimethoprim is used for another indication, monitor closely for reduced efficacy. Avoid combination
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Maitake: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Memantine: Trimethoprim may enhance the adverse/toxic effect of Memantine. Specifically, the risk of myoclonus and/or delirium may be increased. Trimethoprim may increase the serum concentration of Memantine. Memantine may increase the serum concentration of Trimethoprim. Monitor therapy
Mercaptopurine: Sulfamethoxazole may enhance the myelosuppressive effect of Mercaptopurine. Monitor therapy
Mercaptopurine: Trimethoprim may enhance the myelosuppressive effect of Mercaptopurine. Monitor therapy
MetFORMIN: Trimethoprim may increase the serum concentration of MetFORMIN. Monitor therapy
Methenamine: May enhance the adverse/toxic effect of Sulfonamide Antibiotics. Specifically, the combination may result in the formation of an insoluble precipitate in the urine. Avoid combination
Methotrexate: Trimethoprim may enhance the adverse/toxic effect of Methotrexate. Management: Consider avoiding concomitant use of methotrexate and either sulfamethoxazole or trimethoprim. If used concomitantly, monitor for the development of signs and symptoms of methotrexate toxicity (e.g., bone marrow suppression). Consider therapy modification
MetroNIDAZOLE (Systemic): May enhance the adverse/toxic effect of Products Containing Propylene Glycol. A disulfiram-like reaction may occur. Avoid combination
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Monitor therapy
Phenytoin: Trimethoprim may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Trimethoprim. Management: Consider alternatives to this combination when possible, to avoid potential decreased trimethoprim efficacy and increased phenytoin concentrations/effects. Monitor patients receiving this combination closely for both of these possible effects. Consider therapy modification
Phenytoin: Sulfamethoxazole may increase the serum concentration of Phenytoin. Management: Avoid coadministration of phenytoin and sulfamethoxazole. If coadministered, monitor phenytoin concentrations and for evidence of phenytoin toxicity. Risk of toxicity is increased with sulfamethoxazole/trimethoprim combination product. Consider therapy modification
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Potassium P-Aminobenzoate: May diminish the therapeutic effect of Sulfonamide Antibiotics. Avoid combination
PRALAtrexate: Trimethoprim may increase the serum concentration of PRALAtrexate. More specifically, trimethoprim may decrease excretion of pralatrexate. Management: Closely monitor for increased pralatrexate serum level and/or possible toxicity with concomitant use of trimethoprim. Monitor for decreased pralatrexate levels with discontinuation of trimethoprim. Monitor therapy
PRALAtrexate: Sulfamethoxazole may increase the serum concentration of PRALAtrexate. More specifically, sulfamethoxazole may decrease excretion of pralatrexate. Management: Closely monitor for increased pralatrexate serum level and/or possible toxicity with concomitant use of sulfamethoxazole. Monitor for decreased pralatrexate levels with discontinuation of sulfamethoxazole. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Procainamide: Trimethoprim may increase serum concentrations of the active metabolite(s) of Procainamide. Trimethoprim may increase the serum concentration of Procainamide. Management: Consider alternatives to trimethoprim-containing regimens to avoid this interaction. If coadministered, monitor for increased procainamide adverse effects (increased QTc) if trimethoprim is initiated/dose increased. Consider therapy modification
Procaine: May diminish the therapeutic effect of Sulfonamide Antibiotics. Avoid combination
Prothionamide: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Monitor therapy
Pyrimethamine: May enhance the adverse/toxic effect of Trimethoprim. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Quinolones may diminish the therapeutic effect of Agents with Blood Glucose Lowering Effects. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Repaglinide: CYP2C8 Inhibitors (Weak) may increase the serum concentration of Repaglinide. Monitor therapy
RifAMPin: May decrease the serum concentration of Trimethoprim. Monitor therapy
RifAMPin: May decrease the serum concentration of Sulfamethoxazole. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Monitor therapy
Sapropterin: Trimethoprim may decrease the serum concentration of Sapropterin. Specifically, trimethoprim may decrease tissue concentrations of tetrahydrobiopterin. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Agents with Blood Glucose Lowering Effects. Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Spironolactone: Trimethoprim may enhance the hyperkalemic effect of Spironolactone. Monitor therapy
Sulfonylureas: Sulfonamide Antibiotics may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Avoid use of live attenuated typhoid vaccine (Ty21a) in patients being treated with systemic antibacterial agents. Postpone vaccination until 3 days after cessation of antibiotics and avoid starting antibiotics within 3 days of last vaccine dose. Consider therapy modification
Varenicline: Trimethoprim may increase the serum concentration of Varenicline. Management: Monitor for increased varenicline adverse effects with concomitant use of trimethoprim, particularly in patients with severe renal impairment. International product labeling recommendations vary. Consult appropriate labeling. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Sulfonamide Antibiotics may enhance the anticoagulant effect of Vitamin K Antagonists. Management: Consider reducing the vitamin K antagonist dose by 10% to 20% prior to starting the sulfonamide antibiotic. Monitor INR closely to further guide dosing. Consider therapy modification
Test Interactions
Increased creatinine (Jaffé alkaline picrate reaction); increased serum methotrexate by dihydrofolate reductase method
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
Frequency not defined:
Cardiovascular: Hypersensitivity myocarditis (Nayak 2013), polyarteritis nodosa
Dermatologic: Acute generalized exanthematous pustulosis (Anliker 2003), erythema multiforme, exfoliative dermatitis, skin photosensitivity, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis (Zhang 2019), urticaria
Endocrine & metabolic: Hyperkalemia (Alappan 1999), hyponatremia (Babyev 2013)
Gastrointestinal: Abdominal pain, anorexia, diarrhea, glottis edema, kernicterus (neonates), nausea, pancreatitis, stomatitis, vomiting
Genitourinary: Crystalluria, diuresis, toxic nephrosis (with anuria and oliguria)
Hematologic & oncologic: Agranulocytosis (Andres 2003), aplastic anemia (IAAAS 1989), eosinophilia, hemolysis (with G6PD deficiency) (Calabrò 1989), hemolytic anemia (Williams 2017), Henoch-Schönlein purpura, hypoprothrombinemia, leukopenia (Gordin 1984), megaloblastic anemia (Kobrinsky 1981), methemoglobinemia (Carroll 2016), neutropenia, thrombocytopenia (Mitta 2019)
Hepatic: Cholestatic jaundice (Ogilvie 1980), hepatotoxicity (including hepatitis, cholestasis, and hepatic necrosis) (Slim 2017), hyperbilirubinemia, increased serum transaminases
Hypersensitivity: Angioedema, serum sickness (Platt 1988)
Immunologic: Drug reaction with eosinophilia and systemic symptoms (Kardaun 2013)
Nervous system: Apathy, aseptic meningitis (Bruner 2014), ataxia, chills, depression, fatigue, hallucination, headache, insomnia, nervousness, peripheral neuritis, seizure, vertigo
Neuromuscular & skeletal: Arthralgia, asthenia, myalgia, rhabdomyolysis (mainly in AIDS patients), systemic lupus erythematosus
Ophthalmic: Conjunctival injection, injected sclera, uveitis
Otic: Tinnitus
Renal: Interstitial nephritis, nephrotoxicity (in association with concomitant cyclosporine)
Respiratory: Cough, dyspnea, pulmonary infiltrates
Miscellaneous: Fever (Gordin 1984)
Postmarketing:
Cardiovascular: Prolonged QT interval on ECG (Lopez 1987)
Endocrine & metabolic: Hypoglycemia (rare: <1%) (Nunnari 2010; Strevel 2006), metabolic acidosis (Porras 1998)
Gastrointestinal: Clostridioides difficile colitis (rare: <1%) (Brown 2013; Gordin 1994; Hensgens 2012), dysgeusia (Syed 2016)
Hematologic & oncologic: Thrombotic thrombocytopenic purpura (Bapani 2013)
Hypersensitivity: Anaphylaxis (rare: <1%) (Harle 1988; Kuyucu 2014), fixed drug eruption (Can 2014)
Renal: Acute kidney injury (Fraser 2012)
Respiratory: Acute respiratory distress syndrome (Miller 2019)
Warnings/Precautions
Concerns related to adverse effects:
• Blood dyscrasias: Fatalities associated with severe reactions including agranulocytosis, aplastic anemia, and other blood dyscrasias have occurred; discontinue use at first sign of rash or signs of serious adverse reactions.
• Dermatologic reactions: Fatalities associated with severe reactions including Stevens-Johnson syndrome and toxic epidermal necrolysis have occurred; discontinue use at first sign of rash.
• Hepatic necrosis: Fatalities associated with hepatic necrosis have occurred; discontinue use at first sign of rash or signs of serious adverse reactions.
• Hyperkalemia: May cause hyperkalemia; potential risk factors for trimethoprim-induced hyperkalemia include high dosage (20 mg/kg/day of trimethoprim), renal impairment, older age, hypoaldosteronism, and concomitant use of medications causing or exacerbating hyperkalemia (Perazella 2000).
• Hypoglycemia: May cause hypoglycemia, particularly in malnourished, or patients with renal or hepatic impairment.
• Hyponatremia: Severe and symptomatic hyponatremia may occur, particularly in patients treated for Pneumocystis jirovecii pneumonia (PCP).
• Sulfonamide (“sulfa”) allergy: Traditionally, concerns for cross-reactivity have extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur, or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides and antibiotic sulfonamides. A nonantibiotic sulfonamide compound which contains the arylamine structure and therefore may cross-react with antibiotic sulfonamides is sulfasalazine (Zawodniak 2010). T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
• Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
• Thrombocytopenia: Immune mediated thrombocytopenia may occur. Severe cases which may be life-threatening or fatal have been reported. Thrombocytopenia usually resolves within 1 week following discontinuation of therapy.
Disease-related concerns:
• Asthma/allergies: Use with caution in patients with allergies or asthma.
• Hepatic impairment: Use with caution in patients with hepatic impairment.
• Renal impairment: Use with caution in patients with renal impairment; dosage adjustment recommended. Maintain adequate hydration to prevent crystalluria.
• Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
• Leucovorin: Avoid concomitant use when treating Pneumocystis jirovecii pneumonia (PCP) in patients with HIV; may increase risk of treatment failure and death.
Special populations:
• AIDS patients: Incidence of adverse effects appears to be increased in patients with AIDS.
• Elderly: Use with caution in elderly patients; greater risk for more severe adverse reactions, including hyperkalemia associated with trimethoprim use. Elderly patients are at an increased risk for severe and potentially life-threatening hyperkalemia when trimethoprim is used concomitantly with medications known to cause or exacerbate hyperkalemia, such as spironolactone, ACE inhibitors, or ARBs (Antoniou 2010; Antoniou 2011; Antoniou, 2015).
• G6PD deficiency: Use with caution in patients with G6PD deficiency; hemolysis may occur (dose-related).
• Patients with potential for folate deficiency: Use with caution in patients with potential folate deficiency (malnourished, chronic anticonvulsant therapy, or elderly).
• Porphyria: Use with caution in patients with porphyria.
• Slow acetylators: May be more prone to adverse reactions.
Dosage form specific issues:
• Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer’s labeling.
• Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP ["Inactive" 1997]; Zar 2007).
• Sulfite sensitivity: Injection may contain sodium metabisulfite, a sulfite that may cause allergic-type reactions, including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible persons. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic persons.
Other warnings/precautions:
• Appropriate use: When used for uncomplicated urinary tract infections, this combination should not be used if a single agent is effective. Additionally, sulfonamides should not be used to treat group A beta-hemolytic streptococcal infections.
Monitoring Parameters
CBC, serum potassium, creatinine, BUN
Pregnancy Considerations
Sulfamethoxazole and trimethoprim cross the placenta.
An increased risk of congenital malformations (neural tube defects, cardiovascular malformations, urinary tract defects, oral clefts, club foot) following maternal use of sulfamethoxazole and trimethoprim during pregnancy has been observed in some studies. Folic acid supplementation may decrease this risk (Crider 2009; Czeizel 2001; Hernandez-Diaz 2000; Hernandez-Diaz 2001; Matok 2009). Due to theoretical concerns that sulfonamides pass the placenta and may cause kernicterus in the newborn, neonatal health care providers should be informed if maternal sulfonamide therapy is used near the time of delivery (HHS [OI adult 2020]).
The pharmacokinetics of sulfamethoxazole and trimethoprim are similar to nonpregnant values in early pregnancy (Ylikorkala 1973). Sulfamethoxazole and trimethoprim are recommended for the prophylaxis or treatment of Pneumocystis jirovecii pneumonia (PCP), prophylaxis of Toxoplasmic gondii encephalitis (TE), and for the acute and chronic treatment of Q fever in pregnancy (Anderson [CDC 2013]; HHS [OI adult 2020]). Sulfonamides may also be used to treat other infections in pregnant women when clinically appropriate; use during the first trimester should be limited to situations where no alternative therapies are available (ACOG 717 2017).
Patient Education
What is this drug used for?
• It is used to treat or prevent bacterial infections.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Nausea
• Vomiting
• Diarrhea
• Lack of appetite
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Severe sulfonamide reaction like rash; red, swollen, blistered, or peeling skin; red or irritated eyes; mouth, throat, nose, or eye sores; fever, chills, or sore throat.
• Cough that is new or worse
• Loss of strength and energy
• Any bruising or bleeding
• Liver problems like dark urine, fatigue, lack of appetite, nausea or abdominal pain, light-colored stools, vomiting, or yellow skin.
• High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, or numbness or tingling feeling.
• Aseptic meningitis like headache, fever, chills, severe nausea or vomiting, stiff neck, rash, sensitivity to lights, fatigue, or confusion.
• Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
• Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
• Low sodium like headache, trouble focusing, trouble with memory, confusion, weakness, seizures, or change in balance.
• Mood changes
• Sensing things that seem real but are not
• Muscle pain
• Joint pain
• Purple patches on skin or mouth
• Shortness of breath
• Severe injection site pain
• Burning
• Swelling
• Irritation
• Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
Frequently asked questions
- What drugs should be avoided with a sulfa allergy?
- Does Bactrim cause headaches?
- Can I drink alcohol when taking sulfamethoxazole / trimethoprim DS?
- What dose of co-trimoxazole is used in a patient with a UTI?
More about sulfamethoxazole / trimethoprim
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1,716)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: sulfonamides
- En español
Patient resources
- Sulfamethoxazole and trimethoprim drug information
- Sulfamethoxazole/trimethoprim (Advanced Reading)
- Sulfamethoxazole and Trimethoprim Tablets
- Sulfamethoxazole and Trimethoprim Injection
- Sulfamethoxazole and Trimethoprim Suspension
Other brands
Bactrim, Septra, SMZ-TMP DS, Cotrim, ... +3 more
Professional resources
- Sulfamethoxazole Trimethoprim Oral Suspension prescribing information
- Sulfamethoxazole and Trimethoprim (FDA)
- Sulfamethoxazole and Trimethoprim Double Strength (FDA)
- Sulfamethoxazole and Trimethoprim Injection (FDA)
- Sulfamethoxazole and Trimethoprim Suspension (FDA)
Other brands
Bactrim, Septra, Co-trimoxazole, Sulfatrim
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.