Sulfamethoxazole / Trimethoprim Dosage
Medically reviewed by Drugs.com. Last updated on Aug 3, 2023.
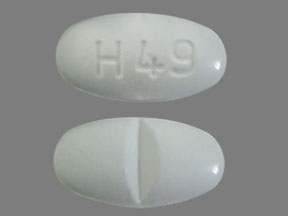
Applies to the following strengths: 400 mg-80 mg; 800 mg-160 mg; 200 mg-40 mg/5 mL; 80 mg-16 mg/mL
Usual Adult Dose for:
- Pneumocystis Pneumonia
- Pneumocystis Pneumonia Prophylaxis
- Urinary Tract Infection
- Shigellosis
- Bronchitis
- Traveler's Diarrhea
- Cystitis
- Pyelonephritis
- Granuloma Inguinale
- Meningitis
- Toxoplasmosis
- Toxoplasmosis - Prophylaxis
- Protozoan Infection
Usual Pediatric Dose for:
- Otitis Media
- Urinary Tract Infection
- Shigellosis
- Pneumocystis Pneumonia
- Pneumocystis Pneumonia Prophylaxis
- Meningitis
- Toxoplasmosis
- Toxoplasmosis - Prophylaxis
- Protozoan Infection
Additional dosage information:
Usual Adult Dose for Pneumocystis Pneumonia
IV: 15 to 20 mg/kg/day (trimethoprim component) IV in 3 or 4 equally divided doses (every 6 to 8 hours) for 14 days
- Maximum dose: 960 mg/day (trimethoprim component)
Comments:
- IV: In a published article, a total daily dose of 10 to 15 mg/kg was sufficient in 10 adult patients with normal renal function.
- Oral: For documented infection
Use: For the treatment of Pneumocystis jirovecii pneumonia
US CDC, National Institutes of Health (NIH), and HIV Medicine Association of the Infectious Diseases Society of America (HIVMA/IDSA) Recommendations for HIV-Infected Adults:
Moderate to Severe Pneumocystis Pneumonia (PCP):
- Preferred therapy: 15 to 20 mg/kg/day (trimethoprim component) IV in divided doses every 6 or 8 hours
Mild to Moderate PCP:
- Preferred therapy: 15 to 20 mg/kg/day (trimethoprim component) orally in 3 divided doses OR sulfamethoxazole-trimethoprim 1600 mg-320 mg orally 3 times a day
Total Duration of Therapy: 21 days
Comments:
- Recommended as preferred therapy for treating PCP due to P jirovecii
- For moderate to severe PCP: May switch from IV to oral formulation after clinical improvement
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Pneumocystis Pneumonia Prophylaxis
Sulfamethoxazole-trimethoprim 800 mg-160 mg orally once a day
Use: For prophylaxis against P jirovecii pneumonia in immunosuppressed individuals considered at increased risk of developing P jirovecii pneumonia
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adults:
Primary and Secondary Prophylaxis:
- Preferred therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally once a day OR sulfamethoxazole-trimethoprim 400 mg-80 mg orally once a day
- Alternative therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally 3 times a week
Comments:
- Recommended as the preferred regimen, and as an alternative regimen, for preventing the first episode of PCP (primary prophylaxis) and preventing subsequent episodes of PCP (secondary prophylaxis)
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Urinary Tract Infection
IV: 8 to 10 mg/kg/day (trimethoprim component) IV in 2 to 4 equally divided doses (every 6, 8, or 12 hours) for 14 days
- Maximum dose: 960 mg/day (trimethoprim component)
Comments:
- Initial episodes of uncomplicated urinary tract infections should be treated with an effective single-agent antibacterial rather than the combination.
Uses:
- IV: For the treatment of severe or complicated urinary tract infections due to susceptible strains of Escherichia coli, Klebsiella species, Enterobacter species, Morganella morganii, and Proteus species when oral administration is not feasible and when the organism is not susceptible to single-agent antibacterials effective in the urinary tract
- Oral: For the treatment of urinary tract infections due to susceptible strains of E coli, Klebsiella species, Enterobacter species, M morganii, Proteus mirabilis, and P vulgaris
Usual Adult Dose for Shigellosis
IV: 8 to 10 mg/kg/day (trimethoprim component) IV in 2 to 4 equally divided doses (every 6, 8, or 12 hours) for 5 days
- Maximum dose: 960 mg/day (trimethoprim component)
Comments:
- Oral: When antibacterial therapy is indicated
Use: For the treatment of enteritis due to susceptible strains of Shigella flexneri and S sonnei
Usual Adult Dose for Bronchitis
Sulfamethoxazole-trimethoprim 800 mg-160 mg orally every 12 hours for 14 days
Use: For the treatment of acute exacerbations of chronic bronchitis due to susceptible strains of Streptococcus pneumoniae or Haemophilus influenzae when physician deems that this drug could offer some advantage over the use of a single antimicrobial agent
Usual Adult Dose for Traveler's Diarrhea
Sulfamethoxazole-trimethoprim 800 mg-160 mg orally every 12 hours for 5 days
Use: For the treatment of traveler's diarrhea due to susceptible strains of enterotoxigenic E coli
Usual Adult Dose for Cystitis
Infectious Diseases Society of America (IDSA) and European Society for Microbiology and Infectious Diseases (ESCMID) Recommendations: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally twice a day
Duration of therapy:
- Acute uncomplicated cystitis: 3 days
- Acute pyelonephritis: 14 days
Comments:
- Recommended for acute uncomplicated cystitis if local resistance rates of infecting uropathogens do not exceed 20% or infecting strain is known to be susceptible
- Recommended for pyelonephritis if uropathogen is known to be susceptible
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Pyelonephritis
Infectious Diseases Society of America (IDSA) and European Society for Microbiology and Infectious Diseases (ESCMID) Recommendations: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally twice a day
Duration of therapy:
- Acute uncomplicated cystitis: 3 days
- Acute pyelonephritis: 14 days
Comments:
- Recommended for acute uncomplicated cystitis if local resistance rates of infecting uropathogens do not exceed 20% or infecting strain is known to be susceptible
- Recommended for pyelonephritis if uropathogen is known to be susceptible
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Granuloma Inguinale
US CDC Recommendations: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally twice a day
Duration of therapy: At least 3 weeks and until all lesions have completely healed
Comments:
- Recommended as an alternative regimen for the treatment of granuloma inguinale
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Meningitis
IDSA Recommendations: 10 to 20 mg/kg/day (trimethoprim component) IV in divided doses every 6 to 12 hours
Duration of therapy:
- Aerobic gram-negative bacilli: 21 days
- Listeria monocytogenes: At least 21 days
Comments:
- Recommended as an alternative regimen for meningitis due to L monocytogenes, E coli, other Enterobacteriaceae (depending on in vitro susceptibility test results), or methicillin-resistant Staphylococcus aureus
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Toxoplasmosis
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adults: 5 mg/kg (trimethoprim component) IV or orally twice a day
Duration of therapy: At least 6 weeks
Comments:
- Recommended as an alternative regimen for treating Toxoplasma gondii encephalitis
- Duration of therapy may be longer if clinical/radiologic disease is extensive or incomplete response at 6 weeks.
- After completion of acute therapy, all patients should be continued on chronic maintenance therapy.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Toxoplasmosis - Prophylaxis
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adults:
Primary Prophylaxis:
- Preferred regimen: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally once a day
- Alternative regimens: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally 3 times a week OR sulfamethoxazole-trimethoprim 400 mg-80 mg orally once a day
Chronic Maintenance Therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally twice a day OR sulfamethoxazole-trimethoprim 800 mg-160 mg orally once a day
Comments:
- Recommended as the preferred regimen, and as alternative regimens, for preventing the first episode of T gondii encephalitis (primary prophylaxis)
- Recommended as alternative regimens for chronic maintenance therapy (secondary prophylaxis) for T gondii encephalitis
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Protozoan Infection
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adults:
Acute Infection:
- Preferred therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally (or IV) 4 times a day for 10 days OR sulfamethoxazole-trimethoprim 800 mg-160 mg orally (or IV) twice a day for 7 to 10 days
Chronic Maintenance Therapy:
- Preferred therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally 3 times a week
Comments:
- Recommended as preferred therapy for treating cystoisosporiasis (formerly isosporiasis) due to Cystoisospora belli (formerly Isospora belli); recommended for acute infection and for chronic maintenance therapy (secondary prophylaxis) in patients with CD4 count less than 200 cells/mm3
- For acute infection: Can start with twice-daily dosing first and increase daily dose and/or duration (up to 3 to 4 weeks) if symptoms worsen/persist; IV therapy may be used for patients with potential/documented malabsorption.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Otitis Media
2 months or older: 4 mg/kg (trimethoprim component) orally every 12 hours for 10 days
Comments:
- This drug is not indicated for prophylactic or prolonged use in otitis media at any age.
Use: For the treatment of acute otitis media due to susceptible strains of S pneumoniae or H influenzae when according to physician judgment this drug offers some advantage over the use of other antimicrobial agents
Usual Pediatric Dose for Urinary Tract Infection
2 months or older:
- IV: 8 to 10 mg/kg/day (trimethoprim component) IV in 2 to 4 equally divided doses (every 6, 8, or 12 hours) for 10 to 14 days
- Maximum dose: 960 mg/day (trimethoprim component)
- Oral: 4 mg/kg (trimethoprim component) orally every 12 hours for 10 days
Uses:
- IV: For the treatment of severe or complicated urinary tract infections due to susceptible strains of E coli, Klebsiella species, Enterobacter species, M morganii, and Proteus species when oral administration is not feasible and when the organism is not susceptible to single-agent antibacterials effective in the urinary tract
- Oral: For the treatment of urinary tract infections due to susceptible strains of E coli, Klebsiella species, Enterobacter species, M morganii, P mirabilis, and P vulgaris
Usual Pediatric Dose for Shigellosis
2 months or older:
- IV: 8 to 10 mg/kg/day (trimethoprim component) IV in 2 to 4 equally divided doses (every 6, 8, or 12 hours) for 5 days
- Maximum dose: 960 mg/day (trimethoprim component)
- Oral: 4 mg/kg (trimethoprim component) orally every 12 hours for 5 days
Comments:
- Oral: When antibacterial therapy is indicated
Use: For the treatment of enteritis due to susceptible strains of S flexneri and S sonnei
Usual Pediatric Dose for Pneumocystis Pneumonia
2 months or older:
- IV: 15 to 20 mg/kg/day (trimethoprim component) IV in 3 or 4 equally divided doses (every 6 to 8 hours) for 14 days
- Maximum dose: 960 mg/day (trimethoprim component)
- Oral: 15 to 20 mg/kg/day (trimethoprim component) orally in equally divided doses every 6 hours for 14 to 21 days
Comments:
- Oral: For documented infection
Use: For the treatment of P jirovecii pneumonia
US CDC, NIH, HIVMA/IDSA, and Pediatric Infectious Disease Society (PIDS) Recommendations for HIV-Exposed and HIV-Infected Children:
- IV: 3.75 to 5 mg/kg (trimethoprim component) IV every 6 hours
- Oral: 15 to 20 mg/kg/day (trimethoprim component) orally in divided doses every 6 or 8 hours
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adolescents:
- Moderate to Severe PCP: 15 to 20 mg/kg/day (trimethoprim component) IV in divided doses every 6 or 8 hours
- Mild to Moderate PCP: 15 to 20 mg/kg/day (trimethoprim component) orally in 3 divided doses OR sulfamethoxazole-trimethoprim 1600 mg-320 mg orally 3 times a day
Total Duration of Therapy: 21 days
Comments:
- Recommended as first choice/preferred therapy for treating PCP due to P jirovecii
- Children: After acute pneumonitis resolved in mild to moderate disease, can switch from IV to oral formulation
- Adolescents: For moderate to severe PCP: May switch from IV to oral formulation after clinical improvement
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Pneumocystis Pneumonia Prophylaxis
2 months or older: 75 mg/m2 (trimethoprim component) orally twice a day, on 3 consecutive days per week
Maximum dose: 320 mg/day (trimethoprim component)
Use: For prophylaxis against P jirovecii pneumonia in immunosuppressed individuals considered at increased risk of developing P jirovecii pneumonia
US CDC, NIH, HIVMA/IDSA, and PIDS Recommendations for HIV-Exposed and HIV-Infected Children:
- Primary and Secondary Prophylaxis: 2.5 to 5 mg/kg (trimethoprim component) twice a day
- Maximum dose: 320 mg/day (trimethoprim component)
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adolescents:
Primary and Secondary Prophylaxis:
- Preferred therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally once a day OR sulfamethoxazole-trimethoprim 400 mg-80 mg orally once a day
- Alternative therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally 3 times a week
Comments:
- Children: Recommended as first choice for primary and secondary prophylaxis of PCP
- Adolescents: Recommended as the preferred regimen, and as an alternative regimen, for preventing the first episode of PCP (primary prophylaxis) and preventing subsequent episodes of PCP (secondary prophylaxis)
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Meningitis
IDSA Recommendations:
- Infants and children: 10 to 20 mg/kg/day (trimethoprim component) IV in divided doses every 6 to 12 hours
Duration of therapy:
- Aerobic gram-negative bacilli: 21 days
- L monocytogenes: At least 21 days
Comments:
- Recommended as an alternative regimen for meningitis due to L monocytogenes, E coli, other Enterobacteriaceae (depending on in vitro susceptibility test results), or methicillin-resistant S aureus
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Toxoplasmosis
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adolescents: 5 mg/kg (trimethoprim component) IV or orally twice a day
Duration of therapy: At least 6 weeks
Comments:
- Recommended as an alternative regimen for treating Toxoplasma gondii encephalitis
- Duration of therapy may be longer if clinical/radiologic disease is extensive or incomplete response at 6 weeks.
- After completion of acute therapy, all patients should be continued on chronic maintenance therapy.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Toxoplasmosis - Prophylaxis
US CDC, NIH, HIVMA/IDSA, and PIDS Recommendations for HIV-Exposed and HIV-Infected Children:
Primary Prophylaxis:
- First choice: 150 mg/m2 (trimethoprim component) orally once a day
- Alternative: 150 mg/m2 (trimethoprim component) orally once a day, on 3 consecutive days per week OR 75 mg/m2 (trimethoprim component) orally twice a day OR 75 mg/m2 (trimethoprim component) orally twice a day, 3 times a week on alternate days
Secondary Prophylaxis: 150 mg/m2 (trimethoprim component) orally once a day
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adolescents:
Primary Prophylaxis:
- Preferred regimen: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally once a day
- Alternative regimens: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally 3 times a week OR sulfamethoxazole-trimethoprim 400 mg-80 mg orally once a day
Chronic Maintenance Therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally twice a day OR sulfamethoxazole-trimethoprim 800 mg-160 mg orally once a day
Comments:
- Children: Recommended as the first choice, and as alternative regimens, for primary prophylaxis of toxoplasmosis; recommended as an alternative regimen for secondary prophylaxis (suppressive therapy) of toxoplasmosis
- Adolescents: Recommended as the preferred regimen, and as alternative regimens, for preventing the first episode of T gondii encephalitis (primary prophylaxis); recommended as alternative regimens for chronic maintenance therapy (secondary prophylaxis) for T gondii encephalitis
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Protozoan Infection
US CDC, NIH, HIVMA/IDSA, and PIDS Recommendations for HIV-Exposed and HIV-Infected Children:
- Treatment: 5 mg/kg (trimethoprim component) orally twice a day for 10 days
- Maximum dose: 160 mg/dose (trimethoprim component)
- Secondary Prophylaxis: 2.5 mg/kg (trimethoprim component) orally twice a day, 3 times a week
- Maximum dose: 80 mg/dose (trimethoprim component)
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adolescents:
- Acute Infection: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally (or IV) 4 times a day for 10 days OR sulfamethoxazole-trimethoprim 800 mg-160 mg orally (or IV) twice a day for 7 to 10 days
- Chronic Maintenance Therapy: Sulfamethoxazole-trimethoprim 800 mg-160 mg orally 3 times a week
Comments:
- Children: Recommended as first choice for treatment of cystoisosporiasis and for secondary prophylaxis if severe immunosuppression
- Children: For treatment: If symptoms worsen/persist, the dose may be administered more often (e.g., 3 to 4 times a day) and/or the duration of therapy may be extended to 3 to 4 weeks.
- Adolescents: Recommended as preferred therapy for treating cystoisosporiasis due to C belli; recommended for acute infection and for chronic maintenance therapy (secondary prophylaxis) in patients with CD4 count less than 200 cells/mm3
- Adolescents: For acute infection: Can start with twice-daily dosing first and increase daily dose and/or duration (up to 3 to 4 weeks) if symptoms worsen/persist; IV therapy may be used for patients with potential/documented malabsorption.
- Current guidelines should be consulted for additional information.
Renal Dose Adjustments
CrCl greater than 30 mL/min: No adjustment recommended.
CrCl 15 to 30 mL/min: Usual dose should be reduced by 50%.
CrCl less than 15 mL/min: Not recommended.
Comments:
- This drug is contraindicated in patients with severe renal dysfunction when renal function status cannot be monitored.
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adults and Adolescents for PCP Treatment:
CrCl 10 to 30 mL/min:
- IV: 5 mg/kg (trimethoprim component) IV every 12 hours
- Oral: Sulfamethoxazole-trimethoprim 1600 mg-320 mg orally every 12 hours
CrCl less than 10 mL/min:
- IV: 5 mg/kg (trimethoprim component) IV every 24 hours
- Oral: Sulfamethoxazole-trimethoprim 1600 mg-320 mg orally every 24 hours
Comments:
- Current guidelines should be consulted for additional information.
Liver Dose Adjustments
Marked liver damage: Contraindicated
Precautions
CONTRAINDICATIONS:
- Known hypersensitivity to trimethoprim or sulfonamides
- History of drug-induced immune thrombocytopenia with use of trimethoprim and/or sulfonamides
- Documented megaloblastic anemia due to folate deficiency
- Pediatric patients younger than 2 months
- Marked hepatic damage
- Severe renal insufficiency when renal function cannot be monitored
- Coadministration with dofetilide
Safety and efficacy have not been established in patients younger than 2 months.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Comments:
- Peritoneal dialysis is not effective and hemodialysis is only moderately effective in eliminating each component.
US CDC, NIH, and HIVMA/IDSA Recommendations for HIV-Infected Adults and Adolescents for PCP Treatment:
Hemodialysis:
- IV: 5 mg/kg (trimethoprim component) IV after dialysis on dialysis days
- Oral: Sulfamethoxazole-trimethoprim 1600 mg-320 mg orally after dialysis on dialysis days
Comments:
- To optimize therapy, can consider therapeutic drug monitoring; target trimethoprim levels: 5 to 8 mcg/mL
- Current guidelines should be consulted for additional information.
Other Comments
Administration advice:
- IV: Administer solution by IV infusion over 60 to 90 minutes; do not administer by rapid infusion or bolus injection; do not administer IM.
- Oral suspension: Shake well before use.
- Ensure adequate fluid intake and urinary output to prevent crystalluria.
Storage requirements:
- IV: Store vials at room temperature (15C to 30C [59F to 86F]); do not refrigerate.
- IV (after dilution): Do not refrigerate; use the diluted solution within 6, 4, or 2 hours if diluted in 125, 100, or 75 mL of 5% dextrose in water, respectively.
- Oral suspension: Store at 15C to 25C (59F to 77F); protect from light.
- Tablets: Store at 15C to 25C (59F to 77F) in a dry location; protect from light.
Reconstitution/preparation techniques:
- IV: Must be diluted prior to infusion; after initial entry into vial, remaining contents must be used within 48 hours.
- The manufacturer product information should be consulted.
IV compatibility:
- Compatible solution: 5% dextrose in water
- Compatible infusion systems: Unit-dose containers; unit-dose polyvinyl chloride and polyolefin containers
- This drug in 5% dextrose in water should not be mixed with drugs or solutions in the same container.
General:
- Weight-based dosing recommendations are based on the trimethoprim component.
- To reduce the development of drug-resistant organisms and maintain effective therapy, this drug should be used only to treat or prevent infections proven or strongly suspected to be caused by susceptible bacteria.
- Culture and susceptibility information should be considered when selecting/modifying antibacterial therapy or, if no data are available, local epidemiology and susceptibility patterns may be considered when selecting empiric therapy.
- Appropriate culture and susceptibility testing recommended before therapy to isolate and identify infecting organisms and to establish susceptibility to this drug. Therapy may be started before test results are known; appropriate therapy should be continued when results are available.
- Oral: Each double-strength tablet contains sulfamethoxazole 800 mg and trimethoprim 160 mg; each single-strength tablet contains sulfamethoxazole 400 mg and trimethoprim 80 mg; 5 mL of the oral suspension contains sulfamethoxazole 200 mg and trimethoprim 40 mg.
- Sulfonamides should not be used to treat group A beta-hemolytic streptococcal infections as they will not eradicate the organism and will not prevent sequelae (e.g., rheumatic fever).
Monitoring:
- Hematologic: Complete blood counts (frequently)
- Metabolic: Acid-base disturbances (with IV formulation); serum potassium in patients with underlying potassium metabolism disorders, with renal dysfunction, or using drugs known to induce hyperkalemia; for hyponatremia in symptomatic patients
- Renal: Urinalysis with careful microscopic examination, especially in patients with renal dysfunction (during therapy); renal function tests, especially in patients with renal dysfunction (during therapy)
Patient advice:
- Avoid missing doses and complete the entire course of therapy.
- Drink plenty of fluids.
- Consult physician at once if watery and bloody stools (with or without stomach cramps and fever) develop.
Frequently asked questions
- What drugs should be avoided with a sulfa allergy?
- Does Bactrim cause headaches?
- Can I drink alcohol when taking sulfamethoxazole / trimethoprim DS?
- What dose of co-trimoxazole is used in a patient with a UTI?
More about sulfamethoxazole / trimethoprim
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1,716)
- Drug images
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: sulfonamides
- En español
Patient resources
- Sulfamethoxazole and trimethoprim drug information
- Sulfamethoxazole/trimethoprim (Advanced Reading)
- Sulfamethoxazole and Trimethoprim Tablets
- Sulfamethoxazole and Trimethoprim Injection
- Sulfamethoxazole and Trimethoprim Suspension
Other brands
Bactrim, Septra, SMZ-TMP DS, Cotrim, ... +3 more
Professional resources
- Sulfamethoxazole Trimethoprim Oral Suspension prescribing information
- Sulfamethoxazole and Trimethoprim (FDA)
- Sulfamethoxazole and Trimethoprim Double Strength (FDA)
- Sulfamethoxazole and Trimethoprim Injection (FDA)
- Sulfamethoxazole and Trimethoprim Suspension (FDA)
Other brands
Bactrim, Septra, Co-trimoxazole, Sulfatrim
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.