Sulfadiazine (Monograph)
Drug class: Sulfonamides
VA class: AM650
Chemical name: N1-2-pyrimidinylsulfanilamide
Molecular formula: C10H10N4O2S
CAS number: 68-35-9
Introduction
Antibacterial; intermediate-acting sulfonamide.
Uses for Sulfadiazine
Prevention of Rheumatic Fever Recurrence
Alternative for prevention of recurrent attacks of rheumatic fever (secondary prophylaxis).
IM penicillin G benzathine is drug of choice for secondary prophylaxis of rheumatic fever; alternatives include oral penicillin V, oral sulfadiazine, and oral sulfisoxazole (only available in the US in fixed combination with erythromycin).
AHA and AAP recommend long-term (continuous) secondary prophylaxis in patients who have been treated for documented acute rheumatic fever (even if manifested solely by Sydenham chorea) and in those with evidence of rheumatic heart disease (even after prosthetic valve replacement).
Do not use for treatment of Streptococcus pyogenes (group A β-hemolytic streptococci, GAS) infections (e.g., pharyngitis and tonsillitis). Sulfadiazine will not eradicate S. pyogenes and, therefore, will not prevent sequelae such as rheumatic fever and glomerulonephritis.
Toxoplasmosis
Treatment of toxoplasmosis caused by Toxoplasma gondii; usually used in conjunction with pyrimethamine (and leucovorin). Designated an orphan drug by FDA for use in conjunction with pyrimethamine for treatment of T. gondii encephalitis in patients with or without HIV infection.
CDC, NIH, IDSA, and AAP recommend sulfadiazine in conjunction with pyrimethamine (and leucovorin) as the regimen of choice for initial treatment of toxoplasmosis in HIV-infected adults and adolescents and for treatment of acquired CNS, ocular, or systemic toxoplasmosis in HIV-infected children.
Sulfadiazine in conjunction with atovaquone is recommended by CDC, NIH, and IDSA as one of several alternative regimens for treatment of toxoplasmosis in HIV-infected adults and adolescents who cannot tolerate or do not respond to or relapsed with the regimen of choice; sulfadiazine and atovaquone regimen not adequately studied for treatment of toxoplasmosis in children.
Sulfadiazine in conjunction with pyrimethamine (and leucovorin) is the regimen of choice for treatment of congenital toxoplasmosis. Empiric treatment of congenital toxoplasmosis should be strongly considered if the mother had symptomatic or asymptomatic Toxoplasma infection during pregnancy, even if the mother received toxoplasmosis treatment during the pregnancy.
Sulfadiazine used in conjunction with pyrimethamine (and leucovorin) is the regimen of choice for chronic maintenance therapy (secondary prophylaxis) to prevent relapse of T. gondii encephalitis† [off-label] in HIV-infected adults, adolescents, and children who have completed initial treatment of the disease.
Acute Otitis Media (AOM)
Has been used in conjunction with penicillin for treatment of AOM caused by susceptible Haemophilus influenzae.
When anti-infective therapy indicated for treatment of AOM, AAP recommends high-dose amoxicillin or fixed combination of amoxicillin and clavulanate as drugs of first choice for initial treatment and certain cephalosporins (cefdinir, cefpodoxime, cefuroxime, ceftriaxone) as alternatives for initial treatment in penicillin-allergic patients who do not have a history of severe and/or recent penicillin-allergic reactions. AAP states that sulfonamides should not be used as alternatives in patients who do not respond to amoxicillin.
Chancroid
Has been used for treatment of chancroid caused by H. ducreyi. CDC recommends azithromycin, ceftriaxone, ciprofloxacin, or erythromycin as the drugs of choice for chancroid; sulfadiazine not included in CDC recommendations.
Chlamydial Infections
Has been used for treatment of infections caused by Chlamydia trachomatis (e.g., inclusion conjunctivitis, trachoma). Other anti-infectives (e.g., azithromycin, erythromycin) usually drugs of choice for these infections.
Haemophilus influenzae Infections
Has been used for treatment of meningitis caused by H. influenzae as an adjunct to streptomycin. Other anti-infectives (e.g., ceftriaxone, cefotaxime, chloramphenicol, cefepime, meropenem, fluoroquinolones) usually recommended.
Malaria
Has been used as an adjunct in the treatment of malaria caused by chloroquine-resistant Plasmodium falciparum. Not included in recommendations for treatment of malaria.
Neisseria meningitidis Infections
Has been used for chemoprophylaxis in close contacts of individuals with invasive meningococcal disease caused by sulfonamide-susceptible Neisseria meningitidis serogroup A. No longer recommended because of high prevalence of N. meningitidis resistant to sulfonamides. CDC and AAP recommend rifampin, ciprofloxacin, or ceftriaxone for such prophylaxis.
Has been used for treatment of infections caused by susceptible N. meningitidis (including meningitis). Other anti-infectives (e.g., ceftriaxone, cefotaxime, penicillin G, ampicillin, chloramphenicol, fluoroquinolones, aztreonam) usually recommended.
Nocardia Infections
Has been used for treatment of nocardiosis. Fixed combination of sulfamethoxazole and trimethoprim (co-trimoxazole) usually treatment of choice for Nocardia infections; some experts suggest avoiding sulfonamides that are less urine soluble (e.g., sulfadiazine).
Multiple-drug regimens may be necessary in immunocompromised patients or those with severe or disseminated infections. Other drugs used alone or in multiple-drug regimens for treatment of nocardiosis include amikacin, tetracyclines, cephalosporins (ceftriaxone), carbapenems (imipenem, meropenem), fixed combination of amoxicillin and clavulanate, clarithromycin, cycloserine, or linezolid. In vitro susceptibility testing, if available, recommended to guide selection of anti-infectives for treatment of severe nocardiosis or for those who cannot tolerate or fail to respond to sulfonamide treatment.
Plague
Has been used for treatment of plague† [off-label] caused by Yersinia pestis. May reduce mortality in patients with bubonic plague, but sulfonamides not generally recommended for pneumonic plague.
Not considered a preferred or alternative agent for treatment of plague; sulfonamides appear to be less effective than other anti-infectives used in the treatment of plague (e.g., streptomycin, tetracycline, doxycycline).
Urinary Tract Infections (UTIs)
Has been used for treatment of UTIs (e.g., pyelonephritis, pyelitis, cystitis) in the absence of obstructive uropathy or foreign bodies.
Use only when UTIs are caused by susceptible Escherichia coli, Klebsiella, Enterobacter, Staphylococcus aureus, Proteus mirabilis, or P. vulgaris and only when other more soluble sulfonamides have been ineffective.
Sulfadiazine Dosage and Administration
Administration
Oral Administration
Administer orally with a full glass (250 mL) of water.
Maintain adequate fluid intake during therapy to minimize risk of crystalluria and stone formation.
Dosage
Pediatric Patients
General Pediatric Dosage
Oral
Infants and children >2 months of age: Manufacturer recommends 75 mg/kg or 2 g/m2 initially, followed by 150 mg/kg or 4 g/m2 daily given in 4–6 equally divided doses.
Children beyond neonatal period: AAP recommends 120–150 mg/kg daily given in 4–6 divided doses for the treatment of mild, moderate, or severe infections.
Prevention of Rheumatic Fever Recurrence
Oral
Infants and children >2 months of age: Manufacturer recommends 500 mg once daily in those weighing <30 kg or 1 g once daily in those weighing >30 kg.
AHA and AAP recommend 500 mg once daily in those weighing ≤27 kg or 1 g once daily in those weighing >27 kg.
Long-term, continuous prophylaxis required. (See Adults under Dosage and Administration.)
Toxoplasmosis
Treatment of Congenital Toxoplasmosis
Oral50 mg/kg twice daily in conjunction with oral pyrimethamine (2 mg/kg once daily for 2 days, then 1 mg/kg once daily for 2–6 months, then 1 mg/kg 3 times weekly) and oral or IM leucovorin (10 mg with each pyrimethamine dose).
Recommended duration in HIV-infected infants is 12 months.
Treatment of Toxoplasmosis in HIV-infected Infants and Children
Oral25–50 mg/kg (up to 1–1.5 g) 4 times daily in conjunction with oral pyrimethamine (2 mg/kg [up to 50 mg] once daily for 3 days, then 1 mg/kg [up to 25 mg] once daily) and oral leucovorin (10–25 mg once daily).
Treatment duration at least 6 weeks; longer duration may be appropriate if disease is extensive or response incomplete at 6 weeks.
Treatment of Toxoplasmosis in HIV-infected Adolescents
Oral1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral pyrimethamine (200-mg loading dose, then 50 mg once daily in those weighing <60 kg or 75 mg once daily in those weighing ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).
Alternatively, 1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral atovaquone (1.5 g twice daily).
Treatment duration at least 6 weeks; longer duration may be appropriate if clinical or radiologic disease is extensive or response incomplete at 6 weeks.
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Infants and Children† [off-label]
Oral42.5–60 mg/kg twice daily (up to 2–4 g daily) in conjunction with oral pyrimethamine (1 mg/kg or 15 mg/m2 [up to 25 mg] once daily) and oral leucovorin (5 mg once every 3 days).
Safety of discontinuing secondary prophylaxis against toxoplasmosis in HIV-infected children receiving potent antiretroviral therapy not extensively studied. If child has completed initial toxoplasmosis treatment, is asymptomatic for toxoplasmosis, and has received ≥6 months of antiretroviral therapy, can consider discontinuing secondary prophylaxis in those 1 to <6 years of age if CD4+ T-cell percentages remain ≥15% for >6 consecutive months or in those ≥6 years of age if CD4+ T-cell counts remain >200/mm3 for >6 consecutive months.
Reinitiate secondary toxoplasmosis prophylaxis if CD4+ T-cell percentages decrease to <15% in HIV-infected children <6 years of age or if CD4+ T-cell counts decrease to <200/mm3 in HIV-infected children ≥6 years of age.
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Adolescents† [off-label]
Oral2–4 g daily in 2–4 divided doses in conjunction with oral pyrimethamine (25–50 mg once daily) and oral leucovorin (10–25 mg once daily).
Criteria for initiating or discontinuing secondary prophylaxis against toxoplasmosis in adolescents are the same as those for adults. (See Adults under Dosage and Administration.)
Adults
General Adult Dosage
Oral
2–4 g initially, followed by 2–4 g daily in 3–6 equally divided doses.
Prevention of Rheumatic Fever Recurrence
Oral
Adults weighing >30 kg: Manufacturer recommends 1 g once daily.
Adults weighing >27 kg: AHA and AAP recommend 1 g once daily.
AHA and AAP recommend long-term, continuous prophylaxis. (See Table 1.)
|
Patient Category |
Duration |
|---|---|
|
Rheumatic fever without carditis |
5 years or until 21 years of age, whichever is longer |
|
Rheumatic fever with carditis but no residual heart disease (no valvular disease) |
10 years since last episode or until 21 years of age, whichever is longer |
|
Rheumatic fever with carditis and residual heart disease (persistent valvular disease) |
10 years since last episode or until 40 years of age, whichever is longer; sometimes for life |
Toxoplasmosis
Treatment of Toxoplasmosis in HIV-infected Adults
Oral1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral pyrimethamine (200-mg loading dose, then 50 mg once daily in those weighing <60 kg or 75 mg once daily in those weighing ≥60 kg) and oral leucovorin (10–25 mg once daily; may be increased to 50 mg once or twice daily).
Alternatively, 1 g every 6 hours in those weighing <60 kg or 1.5 g every 6 hours in those weighing ≥60 kg in conjunction with oral atovaquone (1.5 g twice daily).
Treatment duration at least 6 weeks; longer duration may be appropriate if clinical or radiologic disease is extensive or response incomplete at 6 weeks.
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Adults† [off-label]
Oral2–4 g daily in 2–4 divided doses in conjunction with oral pyrimethamine (25–50 mg once daily) and oral leucovorin (10–25 mg once daily).
Initiate secondary toxoplasmosis prophylaxis in all HIV-infected adults who have been treated for T. gondii encephalitis.
Consider discontinuing secondary toxoplasmosis prophylaxis in adults who completed toxoplasmosis treatment, are asymptomatic with respect to toxoplasmic encephalitis, and have responded to antiretroviral therapy with CD4+ T-cell counts that have remained >200/mm3 for >6 months.
Reinitiate secondary toxoplasmosis prophylaxis if CD4+ T-cell count decreases to <200/mm3.
Nocardiosis
Oral
4–8 g daily for a minimum of 6 weeks. Continue for several months after apparent cure to prevent relapse.
Prescribing Limits
Pediatric Patients
General Pediatric Dosage
Oral
Maximum 6 g daily.
Toxoplasmosis
Treatment in HIV-infected Infants and Children
OralMaximum 1–1.5 g per dose 4 times daily.
Prevention of Recurrence (Secondary Prophylaxis) of Toxoplasmosis in HIV-infected Infants and Children†
OralMaximum 2–4 g daily.
Special Populations
No specific dosage recommendations.
Cautions for Sulfadiazine
Contraindications
-
Hypersensitivity to sulfonamides or other chemically related drugs (e.g., sulfonylureas, thiazides).
-
Infants <2 months of age (except as adjunctive therapy with pyrimethamine for treatment of congenital toxoplasmosis). (See Toxoplasmosis under Uses.)
-
Pregnancy at term.
-
Nursing women.
-
Porphyria.
Warnings/Precautions
Warnings
Severe Reactions
Severe (sometimes fatal) reactions, including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias, reported with sulfonamides.
Sore throat, fever, pallor, purpura, or jaundice may be early indications of serious reactions.
Discontinue sulfadiazine at first appearance of rash or any sign of adverse reactions.
Sensitivity Reactions
Hypersensitivity Reactions
Deaths associated with sulfonamide hypersensitivity reactions reported.
Serum sickness syndrome or serum sickness-like reactions (e.g., fever, chills, rigors, flushing, joint pain, urticarial eruptions, conjunctivitis, bronchospasm, leukopenia) reported with sulfonamides.
Various dermatologic reactions, including rash, pruritus, urticaria, erythema nodosum, erythema multiforme (Stevens-Johnson syndrome), Lyell’s syndrome (may be associated with corneal damage), Behcet’s syndrome, toxic epidermal necrolysis, and exfoliative dermatitis, reported in patients receiving sulfonamides.
Photosensitivity reported.
Incidence of hypersensitivity reactions appears to increase with increased sulfonamide dosage.
Use with caution in patients with severe allergy or bronchial asthma.
If a hypersensitivity reaction occurs during sulfonamide therapy, immediately discontinue the drug.
Desensitization
Desensitization to sulfadiazine has been performed when use of the drug for the treatment of toxoplasmosis was considered necessary in HIV-infected patients who had a history of sulfadiazine hypersensitivity.
Consult specialized references for specific information on desensitization procedures and dosage.
Cross-sensitivity
Although cross-sensitization has been reported to occur between the various anti-infective sulfonamides, some diuretics such as acetazolamide and the thiazides, some goitrogens, and sulfonylurea antidiabetic agents, the association between hypersensitivity to sulfonamide anti-infectives and subsequent sensitivity reactions to non-anti-infective sulfonamides (e.g., thiazides, sulfonylurea antidiabetic agents, furosemide, dapsone, probenecid) appears to result from a predisposition to allergic reactions in general rather than to cross-sensitivity to the sulfa moiety per se.
General Precautions
Renal Effects
Sulfonamides have been associated with renal toxicity manifested by renal colic, nephritis, urolithiasis, toxic nephrosis with anuria and oliguria, hematuria, proteinuria, crystalluria, kidney stone formation, and elevation of BUN and serum creatinine concentrations. Nephritis and hemolytic-uremic syndrome also have been reported.
Adverse renal effects usually are the result of crystalluria. Risk of crystalluria may be decreased by maintaining an adequate urinary output and by increasing urinary pH. Unless the urine is highly acidic and/or the drug is relatively insoluble, alkalinization of the urine usually is not necessary if urinary output is maintained at a minimum of 1.5 L daily.
Perform urinalysis and assess kidney function frequently during sulfonamide therapy. Maintain adequate fluid intake to minimize risk of crystalluria and stone formation.
If persistent, heavy crystalluria, hematuria, or oliguria occurs, sulfonamide therapy should be discontinued and alkali therapy maintained.
Patients with G6PD Deficiency
Hemolysis may occur in individuals with glucose-6-phosphate dehydrogenase (G6PD) deficiency; this effect may be dose-related.
Laboratory Monitoring
Perform CBCs frequently during sulfadiazine therapy.
Perform urinalysis (with careful microscopic examination) frequently during sulfadiazine therapy, especially in patients with impaired renal function.
Considerable interindividual variations in sulfadiazine plasma concentrations occur with a given dosage. Measure sulfadiazine blood concentrations in patients being treated for serious infections. Free sulfonamide concentrations of 5–15 mg/100 mL may be considered therapeutically effective for most infections; concentrations of 12–15 mg/100 mL may be considered optimal for serious infections. Do not exceed total blood concentrations of 20 mg/100 mL since adverse reactions occur more frequently above this level.
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of sulfadiazine and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. Consider that in vitro susceptibility tests are not always reliable for sulfonamides. If the patient is already taking sulfonamides, ensure that follow-up cultures have aminobenzoic acid added to the culture media.
Specific Populations
Pregnancy
Category C.
Contraindicated in pregnant women at term. Crosses placenta; may increase risk of neonatal hyperbilirubinemia and kernicterus.
Lactation
Contraindicated in nursing women; discontinue drug or nursing.
Distributed into milk; may cause kernicterus in the infant.
Pediatric Use
Contraindicated in infants <2 months of age (except when considered necessary for adjunctive use with pyrimethamine for treatment of congenital toxoplasmosis). (See Toxoplasmosis under Uses.)
Kernicterus, caused by displacement of bilirubin from protein binding sites, has occurred in neonates treated with sulfonamides.
Hepatic Impairment
Use with caution.
Renal Impairment
Use with caution. (See Renal Effects under Cautions.)
Common Adverse Effects
GI effects (anorexia, nausea, vomiting, abdominal pain), headache, peripheral neuritis, fever, rash, pancreatitis, stomatitis, depression.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticoagulants, oral (warfarin) |
Sulfonamides may potentiate effects of warfarin by displacing it from its protein-binding sites |
Closely monitor |
|
Antidiabetic agents |
Sulfonamides may potentiate hypoglycemic effects of oral antidiabetic agents, including sulfonylurea agents |
Increased glucose monitoring warranted |
|
Methotrexate |
Sulfonamides may increase concentrations and potentiate effects of methotrexate by displacing it from protein-binding sites or inhibiting renal transport of the drug |
Use concomitantly with caution |
|
Probenecid |
May displace sulfonamides from plasma albumin and increase concentrations of free drug in plasma |
|
|
NSAIAs (indomethacin) |
May displace sulfonamides from binding sites and increase concentrations of free drug in plasma |
Observe patient for possible adverse effects |
|
Salicylates |
May displace sulfonamides from plasma albumin and increase concentrations of free drug in plasma |
Observe patient for possible adverse effects |
|
Thiazide diuretics |
Sulfonamides may potentiate diuretic effects by displacing thiazide diuretics from their protein-binding sites |
|
|
Uricosuric agents |
Sulfonamides may potentiate effects of uricosuric agents by displacing the agents from their protein-binding sites |
Sulfadiazine Pharmacokinetics
Absorption
Bioavailability
Readily absorbed from GI tract.
Peak plasma concentrations attained within 3–7 hours. Considerable interindividual variations in plasma sulfadiazine concentrations attained with a given dosage.
Exists in blood as free, conjugated, and protein-bound drug; only the free form is microbiologically active.
Distribution
Extent
Distributed into most body tissues; appears to freely cross cell membranes.
Distributed into CSF. Free and total CSF concentrations may reach 32–65 and 40–60% of concurrent blood concentrations, respectively. Higher sulfonamide CSF concentrations may be reached if meninges are inflamed.
Crosses placenta.
Distributed into milk.
Plasma Protein Binding
38–48%.
Elimination
Metabolism
Liver; undergoes N4-acetylation (up to 40%).
Elimination Route
Excreted principally in urine in the N4-acetylated form (about 15–40%) and unchanged (about 43–60%). Approximately 50% of a single dose is excreted in the urine within 24 hours; 60–85% can be recovered within 72 hours.
Half-life
About 7–17 hours.
Stability
Storage
Oral
Tablets
20–25°C in tight, light-resistant container.
Actions and Spectrum
-
Competitively inhibits bacterial synthesis of folic acid (pteroylglutamic acid) from aminobenzoic acid.
-
Bacteriostatic in action.
-
Inhibits only microorganisms that synthesize their own folic acid. Animal cells and bacteria capable of utilizing folic acid precursors or preformed folic acid are resistant to sulfonamides.
Advice to Patients
-
Advise patients to drink a full glass of water (250 mL) with each dose and at frequent intervals throughout the day to prevent crystalluria and stone formation.
-
Importance of reporting the occurrence of sore throat, fever, pallor, purpura, or jaundice to a clinician since this may indicate a serious blood disorder.
-
Advise patients that photosensitivity has been reported with sulfonamides and they should avoid exposure to UV light or prolonged exposure to sunlight.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
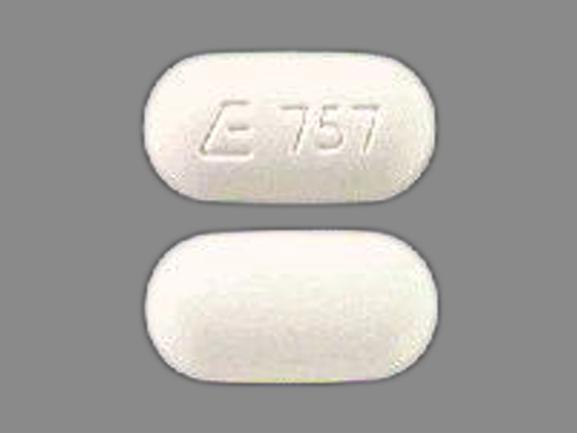
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
500 mg* |
Sulfadiazine Tablets |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions October 20, 2015. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about sulfadiazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: sulfonamides
- En español