Sulfadiazine Dosage
Medically reviewed by Drugs.com. Last updated on May 24, 2023.
Applies to the following strengths: 500 mg; sodium
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Rheumatic Fever Prophylaxis
Secondary prophylaxis of rheumatic fever, if patient is intolerant of penicillin:
1 g orally once a day.
The optimal duration has not been definitely determined. The American Heart Association recommends that prophylaxis be continued for at least 5 years or until the patient reaches age 21 (whichever is longer) for rheumatic fever without carditis, and for 10 years in patients with carditis but no valvar heart disease. Prophylaxis is recommended for at least 10 years since the last episode or until the patient reaches age 40 for carditis and persistent valvar disease; lifelong prophylaxis may be required.
Usual Adult Dose for Toxoplasmosis
Toxoplasmic encephalitis:
Initial dose: Pyrimethamine 200 mg orally once
Maintenance dose:
<60 kg: Sulfadiazine 1 g orally every 6 hours plus pyrimethamine 50 mg orally once a day.
>=60 kg: Sulfadiazine 1500 mg orally every 6 hours plus pyrimethamine 75 mg orally once a day.
In addition, leucovorin 10 to 20 mg/day orally (may increase up to 50 mg/day).
Corticosteroids and anticonvulsants may be given if indicated.
Duration: At least 6 weeks, followed by chronic suppressive therapy.
Usual Adult Dose for Toxoplasmosis - Prophylaxis
Secondary prophylaxis after acute treatment of toxoplasmic encephalitis:
Sulfadiazine, 500 to 1000 mg orally every 6 hours plus pyrimethamine 25 to 50 mg orally once a day plus leucovorin 10 to 25 mg orally once a day.
Duration: Lifelong in HIV-infected patients. Discontinuation may be considered if the patient has maintained CD4+ T-lymphocyte counts >200 cells/microL following HAART (e.g., >6 months) and has no symptoms of toxoplasmosis. Some experts would also recommend an MRI of the brain.
Usual Pediatric Dose for Rheumatic Fever Prophylaxis
Secondary prophylaxis of rheumatic fever, if patient is intolerant of penicillin:
> 2 months and <=27 kg: 500 mg orally once a day.
>27 kg: 1 g orally once a day.
The optimal duration has not been definitely determined. The American Heart Association recommends that prophylaxis be continued for at least 5 years or until the patient reaches age 21 (whichever is longer) for rheumatic fever without carditis, and for 10 years in patients with carditis but no valvar heart disease. Prophylaxis is recommended for at least 10 years since the last episode or until the patient reaches age 40 for carditis and persistent valvar disease; lifelong prophylaxis may be required.
Usual Pediatric Dose for Toxoplasmosis
Congenital toxoplasmosis:
Initial dose: Pyrimethamine 2 mg/kg orally once a day for 2 days
Maintenance dose: Sulfadiazine 50 mg/kg orally twice a day plus pyrimethamine 1 mg/kg orally once a day plus leucovorin 10 mg orally or IM once a day.
Duration: 12 months. After 2 to 6 months, decrease pyrimethamine to 1 mg/kg orally 3 times a week.
Acute acquired toxoplasmosis:
Initial dose: Pyrimethamine 2 mg/kg (maximum 50 mg) orally once a day for 3 days.
Maintenance dose: Sulfadiazine 25 to 50 mg/kg (maximum 1 to 1.5 g/dose) orally every 6 hours plus pyrimethamine 1 mg/kg (maximum 25 mg) orally once a day plus leucovorin 10 to 25 mg orally once a day.
Duration: At least 6 weeks, followed by chronic suppressive therapy.
Usual Pediatric Dose for Toxoplasmosis - Prophylaxis
Secondary prophylaxis after acute treatment of toxoplasmic encephalitis:
Sulfadiazine 85 to 120 mg/kg/day (maximum adult dose, 4 to 6 g/day) orally in 2 to 4 divided doses plus pyrimethamine, 1 mg/kg or 15 mg/m2 (maximum dose 25 mg) orally once a day plus leucovorin 5 mg orally every 3 days.
Duration: Lifelong in HIV-infected patients.
Renal Dose Adjustments
Monitoring is recommended in patients with renal impairment.
Adults:
CrCl 25 to 50 mL/min: Increase dosing interval to every 12 hours.
CrCl 10 to 25 mL/min: Increase dosing interval to every 24 hours
CrCl < 10 mL/min: Generally avoid due to the high risk of crystalluria.
Liver Dose Adjustments
Monitoring is recommended in patients with hepatic impairment.
Precautions
Sulfadiazine is contraindicated in infants <2 months old, except for congenital toxoplasmosis.
Fatalities associated with the administration of sulfonamides, although rare, have occurred due to severe reactions including Stevens-Johnson syndrome, toxic epidermal necrolysis, fulminant hepatic necrosis, agranulocytosis, aplastic anemia, and other blood dyscrasias. Patients should be advised to promptly report possible early signs of serious blood disorders (e.g., sore throat, fever, pallor, purpura, or jaundice).
Sulfonamides should not be used for the treatment of group A beta-hemolytic streptococcus infections because they will not eradicate the streptococci or prevent rheumatic fever and glomerulonephritis.
Sulfadiazine should be given cautiously to patients with blood dyscrasias, severe reactive airways disease, severe allergies, or glucose-6-phosphate dehydrogenase deficiency (due to the risk of hemolysis).
Adequate fluid intake should be maintained to prevent crystalluria and stone formation. Patients should be advised to drink at least 8 ounces of water with each dose and frequently during the day.
Frequent monitoring of complete blood counts and microscopic urinalysis is recommended during sulfonamide therapy.
Dialysis
Generally avoid due to the high risk of crystalluria.
Other Comments
Sulfadiazine and pyrimethamine prophylaxis also prevents Pneumocystis pneumonia.
More about sulfadiazine
- Check interactions
- Compare alternatives
- Pricing & coupons
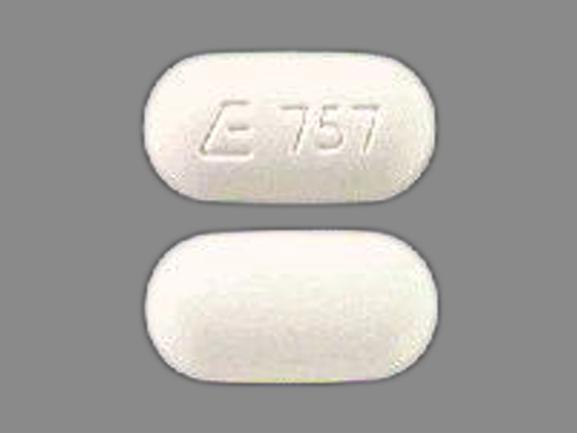
- Drug images
- Side effects
- During pregnancy
- Drug class: sulfonamides
- En español
Patient resources
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.