Carbidopa and Levodopa
Medically reviewed by Drugs.com. Last updated on May 11, 2023.
Pronunciation
(kar bi DOE pa & lee voe DOE pa)
Index Terms
- Carbidopa/Levodopa
- Levodopa and Carbidopa
- Parcopa
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release, Oral:
Rytary: Carbidopa 23.75 mg and levodopa 95 mg, Carbidopa 36.25 mg and levodopa 145 mg, Carbidopa 48.75 mg and levodopa 195 mg, Carbidopa 61.25 mg and levodopa 245 mg [contains fd&c blue #2 (indigotine)]
Suspension, Enteral:
Duopa: Carbidopa 5 mg and levodopa 20 mg per mL (100 mL)
Tablet, Oral:
Sinemet: Carbidopa 10 mg and levodopa 100 mg, Carbidopa 25 mg and levodopa 250 mg [contains fd&c blue #2 aluminum lake]
Sinemet: Carbidopa 25 mg and levodopa 100 mg [contains fd&c yellow #10 aluminum lake]
Generic: Carbidopa 10 mg and levodopa 100 mg, Carbidopa 25 mg and levodopa 100 mg, Carbidopa 25 mg and levodopa 250 mg
Tablet Disintegrating, Oral:
Generic: Carbidopa 10 mg and levodopa 100 mg, Carbidopa 25 mg and levodopa 100 mg, Carbidopa 25 mg and levodopa 250 mg
Tablet Extended Release, Oral:
Sinemet CR: Carbidopa 25 mg and levodopa 100 mg [DSC], Carbidopa 50 mg and levodopa 200 mg [DSC] [contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake]
Generic: Carbidopa 25 mg and levodopa 100 mg, Carbidopa 50 mg and levodopa 200 mg
Related/similar drugs
ropinirole, benztropine, pramipexole, carbidopa / levodopa, Sinemet, Exelon, Gocovri
Brand Names: U.S.
- Duopa
- Rytary
- Sinemet
- Sinemet CR [DSC]
Pharmacologic Category
- Anti-Parkinson Agent, Decarboxylase Inhibitor
- Anti-Parkinson Agent, Dopamine Precursor
Pharmacology
Parkinson disease symptoms are due to a lack of striatal dopamine; levodopa circulates in the plasma to the blood-brain-barrier (BBB), where it crosses, to be converted by striatal enzymes to dopamine; carbidopa inhibits the peripheral plasma breakdown of levodopa by inhibiting its decarboxylation, and thereby increases available levodopa at the BBB
Absorption
Absorption of levodopa may be decreased with high-fat, high-calorie or high-protein meal.
Distribution
Levodopa: 0.9 to 1.6 L/kg (in presence of carbidopa), crosses the blood-brain barrier; Carbidopa: Does not cross the blood-brain barrier
Metabolism
Levodopa has two major pathways (decarboxylation and O-methylation) and two minor pathways (transamination and oxidation) of metabolism; Carbidopa inhibits the decarboxylation of levodopa to dopamine in the peripheral tissue to allow greater levodopa distribution into the CNS
Excretion
Urine
Time to Peak
Levodopa component: Immediate release: 0.5 to 1 hour; controlled release: 1.5 to 2 hours; extended release: 1 to 4.5 hours (Hsu 2015; manufacturer's labeling). Intestinal gel [Canadian product]: 2.9 hours with therapeutic plasma levels reached 10 to 30 minutes following morning bolus dose; intestinal suspension: 2.5 hours.
Half-Life Elimination
Levodopa (in presence of carbidopa): Immediate release: 1.5 hours; controlled release: 1.6 hours; extended release: 1.9 hours (Hsu 2015; manufacturer's labeling).
Special Populations: Elderly
The AUC and Cmax of levodopa may be increased in elderly patients.
Special Populations: Gender
Increased carbidopa and levodopa peak concentrations and systemic exposure in females compared with males.
Use: Labeled Indications
Parkinson disease: Treatment of Parkinson disease, postencephalitic parkinsonism, and symptomatic parkinsonism that may follow carbon monoxide and/or manganese intoxication; treatment of motor fluctuations in advanced Parkinson disease (intestinal suspension [Duopa] only).
Off Label Uses
Parkinsonism (including corticobasal degeneration, dementia with Lewy bodies, drug-induced parkinsonism, multiple system atrophy, and progressive supranuclear palsy)
Data from a limited number of patients studied suggest that levodopa may provide transient symptomatic relief in some patients with corticobasal degeneration, dementia with Lewy bodies, drug-induced parkinsonism, multiple system atrophy (MSA), or progressive supranuclear palsy (PSP); dosing utilized was similar to dosing for Parkinson disease [Collins 1995], [Goldman 2008], [Hardie 1988], [Kompoliti 1998], [Ling 2010], [Low 2015], [Molloy 2005], [Tinazzi 2009].
Based on the American Academy of Neurology second consensus statement on the diagnosis of MSA and the Movement Disorder Society criteria for clinical diagnosis of PSP, response to a levodopa challenge (utilizing dosing similar to dosing for Parkinson disease) may contribute to the diagnosis of MSA or PSP [Gilman 2008], [Höglinger 2017].
Restless leg syndrome, intermittent
Based on the American Academy of Sleep Medicine practice parameters for the treatment of restless legs syndrome (RLS) and periodic limb movement disorder, the use of carbidopa and levodopa is an effective and recommended alternative treatment option in patients with intermittent RLS who do not require daily therapy; however, risk of RLS symptom augmentation and early morning rebound symptoms exists with this therapy [AASM [Aurora 2012]].
The European Federation of Neurological Societies/European Neurological Society/European Sleep Research Society guidelines for the management of RLS consider levodopa effective in reducing RLS symptoms as an on-demand treatment in intermittent RLS [EFNS/ENS/ESRS [Garcia-Borreguero 2012]].
Based on the International Restless Legs Syndrome Study Group/European Restless Legs Syndrome Study Group/RLS Foundation guidelines for the prevention and treatment of dopaminergic augmentation in RLS, levodopa may be effective for intermittent treatment of RLS but frequency should be limited to only 2 to 3 administrations per week due to the risk of augmentation [IRLSSG/EURLSSG/RLS-F [Garcia-Borreguero 2016]].
Clinical experience also suggests the utility of carbidopa and levodopa in the management of RLS [Silber 2004].
Contraindications
Hypersensitivity to levodopa, carbidopa, or any component of the formulation; concurrent use with nonselective monoamine oxidase inhibitors (MAOIs) or use within the last 14 days
Tablets: Additional contraindications: Narrow angle glaucoma
Canadian labeling: Additional contraindications (not in US labeling): Clinical or laboratory evidence of uncompensated cardiovascular, endocrine, hepatic, hematologic or pulmonary disease (eg, including bronchial asthma), or renal disease; when administration of a sympathomimetic amine (eg, epinephrine, norepinephrine, isoproterenol) is contraindicated; in the presence of a suspicious, undiagnosed skin lesion or history of melanoma; intestinal gel therapy in patients with any condition preventing the required placement of a PEG tube for administration (ie, pathological changes of gastric wall, inability to bring gastric and abdominal wall together, blood coagulation disorders, peritonitis, acute pancreatitis, paralytic ileus).
Dosing: Adult
Parkinson disease:
Immediate-release tablet, orally disintegrating tablet:
Note: Tablets are available in carbidopa 25 mg/levodopa 100 mg, carbidopa 10 mg/levodopa 100 mg, and carbidopa 25 mg/levodopa 250 mg strengths. For patients with daily levodopa requirements ≤400 mg/day, tablets with carbidopa 25 mg/levodopa 100 mg should be used to decrease the risk of adverse effects from peripheral dopamine. For those with higher daily levodopa requirements, different strength tablets may be given to provide the optimum dosage, as long as a carbidopa dose ≥75 mg/day is maintained (Hoehn 1980; Kaakkola 1985).
Oral: Initial: Carbidopa 12.5 mg/levodopa 50 mg or carbidopa 25 mg/levodopa 100 mg 2 to 3 times daily (Block 1997; Fahn 2004); may increase daily dose by 1 tablet of carbidopa 25 mg/levodopa 100 mg every 1 to 2 days. For patients who require higher doses of levodopa for symptom control, titrating with a tablet that has a carbidopa:levodopa ratio of 1:10 may allow for better symptom control without exceeding the usual maximum dosage of carbidopa. Usual maximum daily dose: Carbidopa 200 mg/day and levodopa 2 g/day; dosing frequency ≥4 times daily may be required. Note: Many experts use a slower titration, over weeks to months, to improve tolerability and establish the lowest dose of levodopa that provides a satisfactory clinical response (Espay 2017; Spindler 2020).
Controlled-release tablet:
Note: Intervals between doses should be 4 to 8 hours while awake; when divided doses are not equal, the smaller doses should be given toward the end of the day.
For patients initiating levodopa therapy:
Note: Controlled-release carbidopa/levodopa may exhibit erratic pharmacokinetics; therefore, controlled-release formulations are not recommended for initial therapy in Parkinson disease (Espay 2017; Grimes 2019; Spindler 2020).
Oral: Initial: Carbidopa 50 mg/levodopa 200 mg 2 times daily, at intervals not <6 hours; may adjust dose no faster than every 3 days to a maximum dose of levodopa 2.4 g/day.
Conversion from immediate release to controlled release: Oral: Initial: Substitute controlled-release dosage at an amount that provides ~10% more levodopa/day; total calculated dosage is administered in divided doses 2 to 3 times/day (or ≥3 times/day for patients maintained on levodopa ≥700 mg). Depending on clinical response, dosage may need to be increased to provide up to 30% more levodopa/day. May adjust dose every 3 days to a maximum dose of levodopa 2.4 g/day.
Extended-release capsule:
Note: Carbidopa/levodopa ER capsules are not interchangeable with other carbidopa/levodopa products on a 1:1 basis.
For patients initiating levodopa therapy: Oral: Initial: Carbidopa 23.75 mg/levodopa 95 mg 3 times daily for 3 days; on day 4, may increase to carbidopa 36.25 mg/levodopa 145 mg 3 times daily (Espay 2017; Pahwa 2014). May increase dose further based on response and tolerability in levodopa 50 mg increments at intervals ≥1 week up to carbidopa 97.5 mg/levodopa 390 mg 3 times daily (Espay 2017). Frequency of dosing may be increased to a maximum of 5 times daily if needed and tolerated (maximum: carbidopa 612.5 mg/levodopa 2.45 g per day).
Conversion from immediate release to extended release: Oral: Initial: Dose based on current total daily dose of levodopa in immediate-release carbidopa/levodopa as follows:
Total daily dose of levodopa in immediate-release carbidopa/levodopa | Recommended starting dosage of extended-release carbidopa/levodopaa | |
|---|---|---|
Total daily dose of levodopa in extended-release carbidopa/levodopa | Initial extended-release carbidopa/levodopa dosing regimenb | |
aFor patients currently treated with IR carbidopa/levodopa plus catechol-O-methyl transferase (COMT) inhibitors (eg, entacapone) and converting to monotherapy with carbidopa/levodopa ER capsules, the initial total daily dose of carbidopa/levodopa ER capsules may need to be increased. bAdjust dose as needed; frequency of dosing may be increased to a maximum of 5 times daily if needed and tolerated (maximum dose: carbidopa 612.5 mg/levodopa 2.45 g per day) (Espay 2017). | ||
400 to 549 mg | 855 mg | 3 capsules ER carbidopa 23.75 mg/levodopa 95 mg 3 times daily |
550 to 749 mg | 1.14 g | 4 capsules ER carbidopa 23.75 mg/levodopa 95 mg 3 times daily |
750 to 949 mg | 1.305 g | 3 capsules ER carbidopa 36.25 mg/levodopa 145 mg 3 times daily |
950 mg to 1.249 g | 1.755 g | 3 capsules ER carbidopa 48.75 mg/levodopa 195 mg 3 times daily |
≥1.25 g | 2.205 g | 3 capsules ER carbidopa 61.25 mg/levodopa 245 mg 3 times daily |
or | ||
2.34 g | 4 capsules ER carbidopa 48.75 mg/levodopa 195 mg 3 times daily | |
Intestinal suspension (Duopa), intestinal gel (Duodopa [Canadian product]):
Note: Prior to initiation of therapy, convert patients from all forms of levodopa to oral IR carbidopa/levodopa tablets. Total daily dose of intestinal infusion (expressed in terms of levodopa) consists of a morning dose, a continuous dose, and extra doses. Maximum daily dose is levodopa 2 g (ie, one cassette per day) administered over 16 hours. Following the daily 16-hour infusion, some patients may require a routine nighttime dosage of oral carbidopa/levodopa. Nighttime intestinal infusion dosing may be necessary in certain rare situations (eg, nocturnal akinesia) (Ricciardi 2016).
Intestinal infusion via PEG-J tube: Initial:
Morning bolus dose: Day 1: Determine levodopa dose by using previous day's first oral IR carbidopa/levodopa dose. Reduce this dose to 60% to 80% of first oral IR carbidopa/levodopa dose and administer this amount over 10 to 30 minutes; usual levodopa dose: 100 to 200 mg (Burack 2018; Fernandez 2013; Lew 2015; Olanow 2014; Pahwa 2014; manufacturer's labeling).
Continuous dose: Day 1: Determine the amount of oral IR levodopa received in previous day's total waking hours. Do not include nighttime or first oral IR carbidopa/levodopa doses. Divide by 16 hours (usual duration of infusion) for hourly infusion rate (Burack 2018; Olanow 2014; Pahwa 2014; manufacturer's labeling). Usual levodopa dose: 20 to 120 mg/hour (Lew 2015; Nyholm 2003).
Extra bolus doses: Usual levodopa dose: 10 to 40 mg every 1 to 2 hours as needed (Lew 2015; Pahwa 2014). Note: Frequent extra doses may cause or worsen dyskinesias.
Day 2 and subsequent dosage adjustment: After day 1 of intestinal infusion, adjust as needed based on response and tolerability.
Restless legs syndrome, intermittent (alternative agent) (off-label use):
Note: Due to risk of augmentation, limit frequency to 2 to 3 administrations per week. May also be taken as needed prior to specific restless legs syndrome (RLS) triggers, such as prolonged immobility (IRLSSG/EURLSSG/RLS-F [Garcia-Borreguero 2016]).
Immediate-release tablet: Oral: Initial: Carbidopa 12.5 mg/levodopa 50 mg to carbidopa 25 mg/levodopa 100 mg as needed in the evening, at bedtime, or upon waking during the night due to RLS symptoms; may adjust dose (based on levodopa component) no faster than every 3 days to a maximum of 200 mg/day (Earley 1996; EFNS/ENS/ESRS [Garcia-Borreguero 2012]; Silber 2004).
Controlled-release tablet: Oral: Initial: Carbidopa 25 mg/levodopa 100 mg as needed before bedtime for RLS symptoms that awaken patient during the night; may adjust dose (based on levodopa component) no faster than every 3 days to a maximum dose of 200 mg/day (Earley 1996; EFNS/ENS/ESRS [Garcia-Borreguero 2012]; Silber 2004).
Discontinuation of therapy: Discontinuation of therapy may result in neuroleptic malignant-like syndrome (Grimes 2019; Serrano-Dueñas 2003). Avoid sudden discontinuation or rapid dose reduction; some experts recommend a gradual taper over several weeks or more (Oliver 2020).
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
Intestinal suspension (Duopa):
Dyskinesias or levodopa-related adverse reactions within 1 hour of morning dose on preceding day: Decrease morning levodopa dose by 20 mg.
Dyskinesias or adverse reactions lasting ≥1 hour on the preceding day: Decrease continuous levodopa dose by 6 mg per hour.
Dyskinesias or adverse reactions lasting for 2 or more periods of ≥1 hour on the preceding day: Decrease continuous levodopa dose by 12 mg per hour.
Reconstitution
Intestinal suspension (Duopa): Fully thaw in refrigerator prior to use. To ensure controlled thawing, take the cartons containing the seven individual cassettes out of the transport box and separate the cartons from each other. Assign a 12-week, use-by date based on the time the cartons are put into the refrigerator to thaw (may take up to 96 hours to thaw). Once thawed, the individual cartons may be packed in a closer configuration within the refrigerator. Remove one cassette from refrigerator 20 minutes prior to administration (failure to use at room temperature may result in inaccurate dosage).
Extemporaneously Prepared
An oral suspension containing carbidopa 1.25 mg and levodopa 5 mg per mL may be made with tablets. Crush ten tablets each containing carbidopa 25 mg and levodopa 100 mg and reduce to a fine powder. Add small portions of a 1:1 mixture of Ora-Sweet® and Ora-Plus® and mix to a uniform paste; mix while adding the vehicle in equal proportions to almost 200 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add sufficient quantity of vehicle to make 200 mL. Label "shake well" and "refrigerate". Stable 42 days under refrigeration. Also stable 28 days at room temperature.
Nahata MC, Morosco RS, and Leguire LE, "Development of Two Stable Oral Suspensions of Levodopa-Carbidopa for Children With Amblyopia," J Pediatr Ophthalmol Strabismus, 2000, 37(6):333-7.11392406Administration
Intestinal suspension (Duopa): Remove one cassette from refrigerator 20 minutes prior to use (failure to use at room temperature may result in inaccurate dosage). Administer as a 16-hour infusion through either a nasojejunal tube (temporary administration) or through a percutaneous endoscopic gastrostomy-jejunostomy (PEG-J) tube (long-term administration) connected to the CADD-Legacy 1400 pump. At the end of administration, disconnect the tube from the pump at the end of the infusion and flush with room-temperature drinking water with a syringe. Following discontinuation of the daily infusion, patients should administer their routine night-time dosage of oral immediate-release carbidopa/levodopa.
Intestinal gel (Duodopa [Canadian product]): Gel is administered directly to the jejunum via a portable infusion pump (CADD-legacy Duodopa pump). Administer through a temporary nasojejunal tube for a short-term test period to evaluate patient response and for dose optimization. Long-term administration requires placement of PEG-J tube for intestinal infusion. Continuous maintenance dose is infused throughout the day for up to 16 hours; if necessary, may administer at night (eg, nocturnal akinesia). Disconnect PEG-J tube from infusion pump at end of infusion and flush with room temperature water to prevent occlusion of tubing. Following discontinuation of the daily infusion, patients should administer their routine night-time dosage of oral levodopa/carbidopa.
Oral:
Extended-release capsule: Administer with or without food; a high-fat, high-calorie meal may delay the absorption of levodopa by ~2 hours. Swallow capsules whole; do not chew, divide, or crush capsules. Patients who have difficulty swallowing intact capsules may open the capsule, sprinkle entire contents on a small amount of applesauce (1 to 2 tablespoons) and consume immediately (do not store for future use).
Oral tablet formulations: Space doses evenly over the waking hours. Administer with meals to decrease GI upset. Controlled release product should not be chewed or crushed. Orally disintegrating tablets do not require water; the tablet should disintegrate on the tongue's surface before swallowing.
Bariatric surgery: Capsule and tablet, extended release: Some institutions may have specific protocols that conflict with these recommendations; refer to institutional protocols as appropriate. Do not cut, crush, or chew. Switch to immediate-release formulation (tablet or orally disintegrating tablet) or capsule may be opened and contents sprinkled onto soft food of choice. Patient should be instructed to swallow the mixture without biting down or chewing.
Dietary Considerations
Avoid high protein diets (>2 g/kg) which may decrease the efficacy of levodopa via competition with amino acids in crossing the blood-brain barrier. Some products may contain phenylalanine.
Storage
Oral formulations: Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F). Protect from light and moisture.
Intestinal suspension (Duopa): Store in freezer at -20°C (-4°F). Fully thaw in refrigerator at 2°C to 8°C (36°F to 46°F) prior to use; protect from light. To ensure controlled thawing, remove the cartons containing the seven individual cassettes from the transport box and separate the cartons from each other. Assign a 12-week, use-by date based on the time the cartons are put in the refrigerator to thaw (may take up to 96 hours to thaw). Once thawed, the individual cartons may be packed in a closer configuration within the refrigerator. Cassettes are for single use only and should be discarded daily following infusion (up to 16 hours). Do not re-use opened cassettes.
Intestinal gel (Duodopa [Canadian product]): Store in refrigerator at 2°C to 8°C (36°F to 46°F). Keep in outer carton to protect from light. Cassettes are for single use only and should be discarded daily following infusion (up to 16 hours).
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When used at chemotherapy doses, hold blood pressure lowering medications for 24 hours before amifostine administration. If blood pressure lowering therapy cannot be held, do not administer amifostine. Use caution with radiotherapy doses of amifostine. Consider therapy modification
Amisulpride (Injection): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Amisulpride (Oral): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Amisulpride (Oral). Avoid combination
Antipsychotic Agents (First Generation [Typical]): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Antipsychotic Agents (First Generation [Typical]). Management: Avoid concomitant therapy if possible. If antipsychotic use is necessary, consider using atypical antipsychotics such as clozapine, quetiapine, or ziprasidone at lower initial doses, or a non-dopamine antagonist (eg, pimavanserin). Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Management: Consider avoiding atypical antipsychotic use in patients with Parkinson disease. If an atypical antipsychotic is necessary, consider using clozapine, quetiapine, or ziprasidone at lower initial doses, or a non-dopamine antagonist (eg, pimavanserin). Consider therapy modification
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Biperiden: May enhance the adverse/toxic effect of Levodopa-Containing Products. Specifically, the risk of choreic movements or dyskinesias may be increased. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brivudine [INT]: May enhance the adverse/toxic effect of Anti-Parkinson Agents (Dopamine Agonist). Specifically, the risk of chorea may be increased. Monitor therapy
Bromopride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
BuPROPion: Anti-Parkinson Agents (Dopamine Agonist) may enhance the adverse/toxic effect of BuPROPion. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Droxidopa: Carbidopa may diminish the therapeutic effect of Droxidopa. Carbidopa may decrease serum concentrations of the active metabolite(s) of Droxidopa. Carbidopa may increase the serum concentration of Droxidopa. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Fosphenytoin-Phenytoin: May diminish the therapeutic effect of Levodopa-Containing Products. Monitor therapy
Glycopyrrolate (Systemic): May decrease the serum concentration of Levodopa-Containing Products. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Iron Preparations: May decrease the serum concentration of Levodopa. Only applies to oral iron preparations. Management: Consider separating doses of the agents by 2 or more hours to minimize the effects of this interaction. Monitor for decreased therapeutic effects of levodopa during concomitant therapy, particularly if doses cannot be separated. Consider therapy modification
Isoniazid: May diminish the therapeutic effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Macimorelin: Levodopa-Containing Products may diminish the diagnostic effect of Macimorelin. Avoid combination
Methionine: May diminish the therapeutic effect of Levodopa-Containing Products. Management: Avoid large daily doses of methionine in patients receiving levodopa (clinical studies showing interaction used 4.5 g methionine daily). More typical doses of methionine (eg, 500 mg) may not cause a problem. Consider therapy modification
Methotrimeprazine: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Methotrimeprazine. Avoid combination
Methylphenidate: May enhance the adverse/toxic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Metoclopramide: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors: Levodopa-Containing Products may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Of particular concern is the development of hypertensive reactions when levodopa is used with nonselective MAOI. Avoid combination
Monoamine Oxidase Inhibitors (Type B): Levodopa-Containing Products may enhance the orthostatic hypotensive effect of Monoamine Oxidase Inhibitors (Type B). Monitor therapy
Multivitamins/Fluoride (with ADE): May diminish the therapeutic effect of Levodopa-Containing Products. Management: Concurrent use of a multivitamin and levodopa (without carbidopa) should be avoided. Consider therapy modification
Multivitamins/Minerals (with ADEK, Folate, Iron): May diminish the therapeutic effect of Levodopa. Multivitamins/Minerals (with ADEK, Folate, Iron) may decrease the serum concentration of Levodopa. Only applies to oral iron-containing preparations. Management: Separate doses of these agents by 2 or more hours. Monitor for decreased levodopa effects, particularly if doses cannot be separated. Concurrent use of a multivitamin and levodopa (without carbidopa) should be avoided. Consider therapy modification
Multivitamins/Minerals (with AE, No Iron): May diminish the therapeutic effect of Levodopa-Containing Products. Management: Concurrent use of a multivitamin and levodopa (without carbidopa) should be avoided. Consider therapy modification
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Papaverine: May enhance the hypotensive effect of Levodopa-Containing Products. Papaverine may diminish the therapeutic effect of Levodopa-Containing Products. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pyridoxine: May diminish the therapeutic effect of Levodopa-Containing Products. Management: The concomitant use of pyridoxine and levodopa (in the absence of a dopa decarboxylase inhibitor (DDI)) should be avoided. Use of a DDI (eg, carbidopa) with levodopa will essentially eliminate the risk of this interaction. Consider therapy modification
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Sapropterin: May enhance the adverse/toxic effect of Levodopa-Containing Products. Monitor therapy
Solriamfetol: May enhance the adverse/toxic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Spiramycin: May decrease the serum concentration of Carbidopa. And thus may decrease the effectiveness of levodopa. Monitor therapy
Sulpiride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Test Interactions
False-positive reaction for urinary glucose; false-negative reaction using glucose-oxidase tests for glucosuria; false-positive urine ketones; false diagnosis for pheochromocytoma (rare) based on plasma and urine levels of catecholamines
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
>10%:
Cardiovascular: Orthostatic hypotension (enteral suspension: 70% to 73%; oral: 1% to 5%)
Central nervous system: Dizziness (2% to 19%), headache (oral : 1% to 17%), depression (enteral suspension: 11%; oral: 1% to 2%)
Gastrointestinal: Nausea (enteral suspension: 30%; oral: 3% to 20%), constipation (enteral suspension: 22%; oral: ≤6%)
Neuromuscular & skeletal: Dyskinesia (2% to 17%), increased creatine phosphokinase (enteral suspension: ≤17%)
Renal: Increased blood urea nitrogen (enteral suspension: ≤13%)
1% to 10%:
Cardiovascular: Hypertension (enteral suspension: 8%), peripheral edema (enteral suspension: 8%), ischemia (oral: ≤2%), chest pain (oral: ≤1%)
Central nervous system: Insomnia (oral: 1% to 9%), anxiety (2% to 8%), confusion (2% to 8%), abnormal dreams (oral: ≤6%), polyneuropathy (enteral suspension: 5%), sleep disorder (enteral suspension: 5%), hallucination (≤5%), psychosis (≤5%), dystonia (oral: ≤2%), on-off phenomenon (oral: 1% to 2%), paresthesia (oral: ≤1%)
Dermatologic: Skin rash (enteral suspension: 5%)
Endocrine & metabolic: Increased serum glucose (≥1%)
Gastrointestinal: Xerostomia (oral: 1% to 7%), diarrhea (≤5%), dyspepsia (≤5%), vomiting (oral: 2% to 5%), anorexia (oral: 1%)
Genitourinary: Bacteriuria (enteral suspension: 5%; oral: ≥1%), urinary tract infection (oral: 2%), hematuria (oral: ≥1%), urinary frequency (oral: ≤1%)
Hematologic & oncologic: Leukocyturia (enteral suspension: 5%; oral: ≥1%), decreased hematocrit (oral: ≥1%), decreased hemoglobin (oral: ≥1%)
Neuromuscular & skeletal: Back pain (oral: ≤2%), muscle cramps (oral: ≤1%), shoulder pain (oral: ≤1%)
Respiratory: Atelectasis (enteral suspension: 8%), oropharyngeal pain (enteral suspension: 8%), upper respiratory tract infection (enteral suspension: 8%; oral: 1% to 2%), dyspnea (oral: ≤2%)
Miscellaneous: Fever (enteral suspension: 5%)
<1%, postmarketing, and/or case reports: Abdominal distress, abdominal pain, abnormal behavior, abnormal gait, abnormality in thinking, agitation, agranulocytosis, alopecia, anemia, angioedema, asthenia, ataxia, blepharospasm, blurred vision, bruxism, bullous rash (including pemphigus-like reactions), cardiac arrhythmia, common cold, cough, decreased mental acuity, decreased serum potassium, delirium, delusions, dementia, diaphoresis, diplopia, discoloration of saliva, discoloration of sweat, disorientation, drowsiness, duodenal ulcer, dysgeusia, dysphagia, edema, euphoria, extrapyramidal reaction, falling, fatigue, flatulence, flushing, gastrointestinal hemorrhage, glossopyrosis, glycosuria, heartburn, hemolytic anemia, Henoch-Schonlein purpura, hiccups, hoarseness, Horner syndrome (reactivation), hot flash, hypotension, impulse control disorder, increased lactate dehydrogenase, increased libido (including hypersexuality), increased serum alanine aminotransferase, increased serum alkaline phosphatase, increased serum aspartate transaminase, increased serum bilirubin, increased tremors, increased uric acid, leukopenia, lower extremity pain, malaise, malignant melanoma, memory impairment, muscle twitching, mydriasis, myocardial infarction, narcolepsy, nervousness, neuroleptic malignant syndrome, nightmares, numbness, oculogyric crisis, palpitations, paranoia, pathological gambling, peripheral neuropathy, phlebitis, positive direct Coombs test, priapism, proteinuria, pruritus, seizure, sense of stimulation, sialorrhea, suicidal ideation, suicidal tendencies, syncope, thrombocytopenia, trismus, urinary incontinence, urinary retention, urine discoloration, urticaria, weight gain, weight loss
Warnings/Precautions
Concerns related to adverse effects:
• Abnormal thinking/behavioral changes: Abnormal thinking and behavior changes have been reported and may include aggressive behavior, agitation, confusion, delirium, delusions, disorientation, paranoid ideation, and psychotic-like behavior.
• Dyskinesias: May cause or exacerbate dyskinesias; may require dosage reduction.
• Hallucinations: Hallucinations may occur and be accompanied by confusion and to a lesser extent sleep disorder and excessive dreaming; typically presents shortly after initiation of therapy and may require dose reduction.
• Impulse control disorders: Dopamine agonists used for Parkinson disease or restless legs syndrome have been associated with compulsive behaviors and/or loss of impulse control, which has manifested as pathological gambling, increased sexual urges, intense urges to spend money, binge or compulsive eating, and/or other intense urges. Dose reduction or discontinuation of therapy has been reported to reverse these behaviors in some, but not all cases.
• Melanoma: Risk for melanoma development is increased in Parkinson disease patients; drug causation or factors contributing to risk have not been established. Patients should be monitored closely and periodic skin examinations should be performed.
• Neuroleptic malignant syndrome: A symptom complex resembling neuroleptic malignant syndrome (NMS) has been reported in association with rapid dose reduction, or abrupt withdrawal. Identification of more severe NMS-like reactions (eg, altered consciousness, hyperthermia, involuntary movements, muscle rigidity, autonomic instability, mental status changes) can be complex; monitor patients closely for this reaction and when the dosage of levodopa is reduced abruptly or discontinued. Discontinue treatment immediately if signs/symptoms arise.
• Orthostatic hypotension: May cause orthostatic hypotension; Parkinson disease patients appear to have an impaired capacity to respond to a postural challenge. Use with caution in patients at risk of hypotension (such as those receiving antihypertensive drugs) or where transient hypotensive episodes would be poorly tolerated (cardiovascular disease or cerebrovascular disease). Parkinson patients being treated with dopaminergic agonists ordinarily require careful monitoring for signs and symptoms of postural hypotension, especially during dose escalation, and should be informed of this risk.
• Somnolence: Somnolence and falling asleep while engaged in activities of daily living (including operation of motor vehicles) have been reported; some cases reported that there were no warning signs for the onset of symptoms. Symptom onset may occur well after initiation of treatment; some events have occurred more than 1 year after start of therapy. Prior to treatment initiation, evaluate for factors that may increase these risks such as concomitant sedating medications, and the presence of sleep disorders. Monitor for drowsiness or sleepiness. If significant daytime sleepiness or episodes of falling asleep during activities that require active participation occurs (eg, driving, conversations, eating), discontinue the medication. There is insufficient information to suggest that dose reductions will eliminate these symptoms. If therapy is continued, advise patient to avoid driving and other potentially dangerous activities.
Disease-related concerns:
• Cardiovascular disease: Use with caution in patients with severe cardiovascular disease, including a history of myocardial infarction who have residual atrial, nodal, or ventricular arrhythmias.
• Endocrine disease: Use with caution in patients with endocrine disease and when interpreting plasma/urine catecholamine levels; falsely diagnosed pheochromocytoma has been rarely reported.
• Glaucoma: Use with caution in patients with glaucoma; monitor IOP carefully; some formulations are contraindicated in patients with narrow-angle glaucoma.
• Hepatic impairment: Use with caution in patients with hepatic impairment.
• Neuropathy: Peripheral neuropathy has been reported with use; prior to initiation, evaluate patients for history of neuropathy and known risk factors (eg, deficiency of vitamin B6 and/or B12, diabetes mellitus, hypothyroidism). Assess patients for peripheral neuropathy periodically during therapy.
• Peptic ulcer disease: Oral products: Use with caution in patients with a history of peptic ulcer disease; risk of GI hemorrhage may be increased.
• Psychotic disorders: Avoid use in patients with a major psychotic disorder. Use with extreme caution in patients with psychotic disorders because of the risk of exacerbating psychosis; observe patients closely for development of depression with concomitant suicidal tendencies.
• Renal impairment: Use with caution in patients with renal impairment.
• Respiratory disease: Use with caution in patients with respiratory disease.
Special populations:
• Elderly: Use with caution in elderly patients; may be more sensitive to CNS effects (eg, hallucinations) of levodopa.
Dosage forms specific issues:
• Intestinal suspension (Duopa): GI complications (eg, bezoar, ileus, implant-site erosion/ulcer, intestinal hemorrhage, intestinal ischemia, intestinal obstruction, intestinal perforation, pancreatitis, peritonitis, pneumoperitoneum, postoperative wound infection) may occur (may be fatal). Patients should notify their health care provider immediately if abdominal pain, prolonged constipation, nausea, vomiting, fever, and/or melanotic stool occur.
• Intestinal gel (Duodopa [Canadian product]): Product should be prescribed only by neurologists experienced in the treatment of Parkinson disease and who have completed the Duodopa Education Program. Response to levodopa/carbidopa intestinal gel therapy should be assessed with a short-term test period of administration via a temporary nasojejunal tube prior to placement of a percutaneous endoscopic gastrostomy-jejunostomy (PEG-J) tube for permanent access and administration. Sudden deterioration in therapy response with recurring motor symptoms may indicate PEG-J tube complications (eg, displacement) or obstruction of the infusion device. Tube or infusion device complications may require initiation of oral levodopa/carbidopa therapy until complications are resolved.
Other warnings/precautions:
• Body fluid discoloration: Urine, saliva, or sweat may appear dark in color (red, brown, black) during therapy.
• Dietary protein: Distribute dietary protein throughout the day to avoid fluctuations in levodopa absorption. A high-protein diet may reduce the effectiveness of the enteral formulations.
• Discontinuation of therapy: Dopaminergic agents have been associated with a syndrome resembling neuroleptic malignant syndrome on abrupt withdrawal, rapid dose reduction, significant dosage reduction after long-term use, or changes in dopaminergic therapy. Avoid sudden discontinuation or rapid dose reduction; taper dose to reduce the risk of hyperpyrexia and confusion.
Monitoring Parameters
Signs and symptoms of Parkinson disease; periodic hepatic function tests, BUN, creatinine, and CBC; periodic skin examinations; blood pressure, standing and sitting/supine; symptoms of dyskinesias, mental status changes; cardiac function (particularly during initial dosage adjustment), IOP (in patients with glaucoma); signs and symptoms of neuroleptic malignant syndrome if abrupt discontinuation required (as with surgery); drowsiness or sleepiness; signs of depression (including suicidal thoughts); signs and symptoms of peripheral neuropathy prior to therapy and periodically during therapy.
Additional Canadian labeling recommendations include vitamin B12, vitamin B6, folic acid, homocysteine, and methylmalonic acid levels prior to initiation and regularly thereafter (Duodopa Canadian product monograph).
Pregnancy Considerations
Carbidopa can be detected in the umbilical cord, but absorption in fetal tissue is minimal. Levodopa crosses the placenta and can be metabolized by the fetus and detected in fetal tissue (Merchant 1995).
The incidence of Parkinson disease in pregnancy is relatively rare, and although information related to the use of carbidopa/levodopa in pregnant women is limited (Ball 1995; Cook 1985; Golbe 1987; Serikawa 2011; Shulman 2000; Tüfekçioğlu 2018; Zlotnik 2014), this combination has the most outcome information available for the treatment of pregnant women (Seier 2017). Current guidelines note that the available information is insufficient to make a recommendation for the treatment of restless legs syndrome in pregnant women (Aurora 2012).
Patient Education
What is this drug used for?
• It is used to treat Parkinson's disease.
• It is used to treat signs like Parkinson's disease caused by other health problems.
• It may be given to you for other reasons. Talk with the doctor.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Nightmares
• Fatigue
• Dry mouth
• Trouble sleeping
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
• Confusion
• Behavioral changes
• Sensing things that seem real but are not
• Uncontrollable urges
• Narcolepsy
• Skin growth
• Mole changes
• Abnormal movements
• Severe headache
• Dark urine
• Yellow skin or eyes
• Vision changes
• Eye pain
• Severe eye irritation
• Shortness of breath
• Burning or numbness feeling
• Swelling of arms or legs
• Vomiting blood
• Black, tarry, or bloody stools
• Persistent constipation
• Nausea
• Vomiting
• Abdominal pain
• Chest pain
• Fast heartbeat
• Abnormal heartbeat
• Chills
• Sore throat
• Bruising
• Bleeding
• Severe dizziness
• Passing out
• Severe loss of strength and energy
• Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
Frequently asked questions
- How long does it take carbidopa levodopa to work?
- How often should carbidopa/levodopa be taken?
- Can carbidopa/levodopa cause high blood pressure?
- What foods should be avoided when taking levodopa?
- Is Rytary better than Sinemet?
- What is the difference between carbidopa, levodopa, and Rytary?
- How long does it take for Rytary to start working?
- How long does Rytary stay in your system?
More about carbidopa / levodopa
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (92)
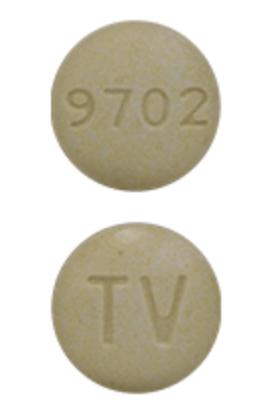
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: dopaminergic antiparkinsonism agents
Patient resources
- Carbidopa and levodopa drug information
- Carbidopa and levodopa enteral
- Carbidopa and levodopa () (Advanced Reading)
- Carbidopa and levodopa (Oral) (Advanced Reading)
- Carbidopa and Levodopa Extended-Release Tablets
Other brands
Sinemet, Rytary, Sinemet CR, Dhivy, ... +2 more
Professional resources
- Levodopa/Carbidopa monograph
- Carbidopa and Levodopa (FDA)
- Carbidopa and Levodopa ODT (FDA)
- Carbidopa and Levodopa Tablets (FDA)
Other brands
Sinemet, Rytary, Sinemet CR, Dhivy, ... +2 more
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.