The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
EPINEPHrine (Mydriatic) (EENT) (Monograph)
Drug class: Mydriatics
ATC class: S01EA01
VA class: OP105
CAS number: 51-42-3
Introduction
Epinephrine, an endogenous catecholamine that is the active principle of the adrenal medulla that may be obtained from the adrenal glands of animals and prepared synthetically, is a mydriatic.
Uses for EPINEPHrine (Mydriatic) (EENT)
In ophthalmology, topical epinephrine is used principally to reduce elevated IOP in the treatment of open-angle (chronic simple) glaucoma, generally as an adjunct to topical miotics, topical β-adrenergic blocking agents, osmotic agents, and/or systemically administered carbonic anhydrase inhibitors. When used in conjunction with these agents, the effect of epinephrine in lowering IOP may be additive. Use of epinephrine in conjunction with miotics may reduce miosis and ciliary spasm that often occur when miotics are used alone.
A diagnosis of open-angle glaucoma should be confirmed by careful gonioscopic and slit lamp studies prior to initiation of epinephrine therapy; use of the drug in patients with angle-closure glaucoma or those who may be predisposed to angle closure is contraindicated. Repeated tonometric readings are advisable during the course of treatment, especially in geriatric patients. Patient response to epinephrine is highly variable; some patients are unresponsive to the drug.
In normal eyes, epinephrine is less effective than other mydriatics; however, the drug produces effective mydriasis when the permeability of the eye is increased during surgery. Epinephrine may be applied topically to the conjunctiva or injected into the anterior chamber of the eye during surgery to provide rapid mydriasis, especially in patients undergoing cataract extraction. Although generally contraindicated in patients with angle-closure glaucoma, epinephrine may be used to produce mydriasis for ophthalmoscopy in patients predisposed to angle closure. These patients should receive a carbonic anhydrase inhibitor (e.g., acetazolamide) and an osmotic agent (e.g., glycerin) orally prior to the examination. However, even these measures may not prevent attacks of acute angle-closure glaucoma unresponsive to treatment; surgery may be required. Within 30 minutes after epinephrine is applied topically, the lower part of the pupil may be dilated enough to permit ophthalmoscopy. After the examination is completed, miosis should be achieved with a topical miotic and the patient carefully observed for signs of increased intraocular pressure. When epinephrine is used as a mydriatic, it is less effective in dark than in light colored eyes; higher concentrations may be needed in patients with brown or hazel eyes.
Epinephrine may break posterior synechiae if a cotton wick saturated with the drug is placed in the lower conjunctival cul-de-sac. Epinephrine may also be administered subconjunctivally concomitantly with atropine and cocaine to produce mydriasis and thereby break posterior synechiae in patients who are unresponsive to topical atropine or scopolamine.
For the systemic uses of epinephrine, see Epinephrine 12:12.12. For the use of epinephrine as a vasoconstrictor in the eye and mucosa, see Epinephrine 52:32.
EPINEPHrine (Mydriatic) (EENT) Dosage and Administration
Administration
Epinephrine solutions are applied topically to the conjunctiva. The drug also may be injected intracamerally (into the anterior chamber of the eye) or subconjunctivally (beneath Tenon’s capsule) to control hemorrhage or produce mydriasis. Epinephrine ophthalmic solutions are intended for topical use only and must not be injected.
Dosage
Dosage of epinephrine hydrochloride, epinephrine bitartrate, and epinephryl borate is expressed in terms of epinephrine.
For the treatment of open-angle glaucoma, the concentration and dosage of epinephrine must be adjusted to the requirements and responses of individual patients as determined by tonometric readings before and during therapy. The usual dosage is 1 or 2 drops of a 1 or 2% solution once or twice daily; however, the frequency of instillation may vary from once every 2–4 days to 4 times daily. To avoid visual disturbances resulting from mydriasis, the drug should be administered at bedtime whenever possible. When separate solutions of epinephrine and a topical miotic are used, the miotic should be instilled 2–10 minutes prior to the epinephrine because of the limited capacity of the conjunctival sac.
During ocular surgery, 1 or more drops of a 0.1% (1:1000) solution of epinephrine as the hydrochloride (no longer commercially available in the US) have been applied topically to the conjunctiva 1–3 times or as necessary to control bleeding or to provide a mydriatic effect. Intraocular injections of the drug in concentrations of 1:10,000 (0.01%) to 1:1000 (0.1%) can be used to control hemorrhage or provide mydriasis. In round-pupil cataract extraction, 0.2 mL (0.2 mg) of a 1:1000 injection may be injected intracamerally; in other cases of cataract extraction, 0.1 mL (0.1 mg) of a 1:1000 injection may be injected subconjunctivally. For use with local anesthetics in ocular surgery, epinephrine may be used in concentrations of 1:200,000 to 1:50,000.
When epinephrine is used to provide mydriasis for ophthalmoscopy in patients predisposed to angle closure, a carbonic anhydrase inhibitor (e.g., 250 mg of acetazolamide) and glycerin 1–1.5 g/kg are given orally 2 hours and 1 hour, respectively, prior to epinephrine. After the eye is anesthetized topically with a drug other than cocaine, the tip of a 1 × 5 mm strip of filter paper moistened with 1 or 2% epinephrine ophthalmic solution is inserted in the inferior cul-de-sac for 1–3 minutes.
To break posterior synechiae, 0.1 mL of a solution containing equal parts of 0.1% (1:1000) epinephrine, 4% cocaine, and 1% atropine may be injected at the limbus.
Cautions for EPINEPHrine (Mydriatic) (EENT)
Ocular Effects
Local adverse reactions occur frequently during topical ocular therapy with epinephrine and many patients are unable to tolerate prolonged use of the drug. Topical application of epinephrine to the conjunctiva frequently causes ocular discomfort and conjunctival irritation including transient burning or stinging, lacrimation, pain or ache around or in the eye, and rebound conjunctival hyperemia. Some of these effects may be reduced if a lower concentration of the drug is used. Compared with other commercially available preparations containing epinephrine salts, those containing epinephryl borate are less acidic and may be better tolerated by some patients. Use of epinephrine in the eye also may cause headache or browache; this effect frequently occurs at the beginning of therapy and may diminish with continued treatment. Rarely, a temporary but clinically important increase in IOP and impairment of outflow facility (even when the angle of the eye remained open) have occurred in patients with glaucoma when epinephrine was used initially without a miotic. Instillation of a miotic such as pilocarpine and/or administration of a carbonic anhydrase inhibitor may be necessary to combat this effect. Mydriasis, blurred vision, and sensitivity to light may occur in some patients being treated for glaucoma; inconvenience to these patients may be minimized if epinephrine is administered at bedtime or following a miotic. In patients with angle-closure glaucoma, dilation of the pupil may precipitate an acute attack. When combination products containing epinephrine and pilocarpine are used, miosis may occur. Prolonged ophthalmic use of epinephrine may cause corneal edema; after very prolonged use, superficial blood vessels in the eye may lose the ability to constrict. Loss of eyelashes occurred after 5 years of epinephrine therapy in one patient having no other symptoms of infection, trauma, irritation, or allergy. The eyelashes grew back within 10 months after the drug was discontinued.
Ophthalmic use of epinephrine may cause allergic reactions characterized by diffuse vascular engorgement, follicular hypertrophy, chemosis, conjunctivitis, and/or iritis. Allergic contact dermatitis of the eyelids, producing such symptoms as edema of the lower lids, thick yellow discharge, and crusting and fissuring of the skin of the eyelids, may also occur. In some instances, allergic reactions may be caused by the preservatives in the preparations.
After prolonged use of epinephrine, localized melanin-like pigmentary deposits may occur in the conjunctiva, eyelids, and/or roughened or edematous areas of the cornea. In geriatric patients, these deposits may occur within translucent conjunctival cysts. The pigmentary deposits may be composed of oxidation products of epinephrine such as adrenochrome; although usually innocuous, they may be mistaken for foreign bodies, nevi, or melanomas. In some patients, large brownish-black casts may form in the lacrimal sac and nasolacrimal duct, resulting in obstruction and epiphora. These casts may be removed by irrigation. Epinephrine may also cause pigment granules to be released from the iris.
Chronic ophthalmic application of epinephrine in aphakic patients may cause maculopathy characterized by macular edema, vascular spasm, and small cysts or fine hemorrhages. Blurring and distortion of vision, central scotoma, and/or loss of visual acuity may result. In some patients, visual impairment may be slight and may respond to a reduction in the concentration or frequency of administration of epinephrine. Maculopathy caused by epinephrine is usually reversible upon withdrawal of the drug but maximal return of vision may take 6 months or more; permanent visual impairment has occurred in some patients. Approximately 20–30% of aphakic patients experience maculopathy during epinephrine therapy.
Intracameral injection of epinephrine 1:1000 has been associated with endothelial damage, irreversible edema, and opacification of the cornea. Results of one study indicate that these effects are caused by sodium bisulfite in concentrations of 0.1% which are present in most commercially available products.
Systemic Effects
Ophthalmic use of epinephrine occasionally causes systemic sympathomimetic effects such as palpitation, tachycardia, extrasystoles, premature ventricular contractions, hypertension, occipital headaches, pallor, trembling, faintness, and increased perspiration. Systemic sympathomimetic effects occur very rarely after application to the conjunctiva but are more likely to occur if the drug is instilled after the corneal epithelium has been damaged or permeability is increased by tonometry, surgery, inflammation, or topical application of a local anesthetic.
Precautions and Contraindications
Patients should be instructed to discontinue using epinephrine and consult their physicians if signs of sensitivity develop or if irritation persists or increases during therapy with the drug. If epinephrine is used prior to ocular surgery, especially for injection with a local anesthetic, the patient should be warned of the possibility of systemic sympathomimetic effects; surgery should not be started until restlessness has subsided.
Some commercially available epinephrine ophthalmic formulations contain sulfites that may cause allergic-type reactions, including anaphylaxis and life-threatening or less severe asthmatic episodes, in certain susceptible individuals. The overall prevalence of sulfite sensitivity in the general population is unknown but probably low; such sensitivity appears to occur more frequently in asthmatic than in nonasthmatic individuals.
The cardiovascular status of the patient should be considered before initiating epinephrine therapy. The drug should be used with caution in patients with vascular hypertension or cardiac disorders, including arrhythmias and cardiovascular disease. Epinephrine should also be used with caution in diabetic, hyperthyroid, aphakic, or geriatric patients or those with cerebral arteriosclerosis, long-standing bronchial asthma, or a history of bronchial asthma. Epinephrine should be used with extreme caution in patients with long-standing bronchial asthma or emphysema who have developed degenerative heart disease.
Epinephrine must be used cautiously, if at all, prior to or during surgery with cyclopropane or halogenated hydrocarbon anesthetics such as halothane. The danger of ventricular arrhythmias such as ventricular premature contractions, tachycardia, or fibrillation may be increased.
Epinephrine ophthalmic preparations generally should not be used in conjunction with the wearing of soft contact lenses, since the drug may cause adrenochrome staining of the lenses.
Epinephrine is contraindicated in patients with angle-closure glaucoma or those predisposed to angle closure. The drug should be used cautiously, if at all, in patients with glaucoma if the nature of the glaucoma has not been established. Epinephrine also is contraindicated in patients with known sensitivity to the drug or to other components in the commercially available preparations and in individuals with organic brain syndrome or cardiac dilatation and coronary insufficiency.
Pediatric Precautions
Safety and efficacy of ophthalmic epinephrine in children have not been established.
Drug Interactions
Miotics and Carbonic Anhydrase Inhibitors
When used in conjunction with topical miotics, osmotic agents, and/or systemically administered carbonic anhydrase inhibitors, the effect of epinephrine in lowering IOP may be additive. However, some evidence suggests that combined therapy with a nonselective β-adrenergic agonist (e.g., epinephrine) and a nonselective β-adrenergic antagonist (e.g., timolol) generally has a less than additive effect. Use of epinephrine in conjunction with miotics may reduce miosis and/or ciliary spasm that often occur when miotics are used alone. In addition, the miotic may reduce mydriasis, blurred vision, and increases in IOP associated with epinephrine therapy. These effects are usually used to therapeutic advantage in the treatment of glaucoma.
General Anesthetics
Absorption of epinephrine in patients receiving cyclopropane or halogenated hydrocarbon general anesthetics may result in arrhythmias including ventricular premature contractions, tachycardia, or fibrillation. Epinephrine is contraindicated for use with chloroform, trichloroethylene, or cyclopropane and should be used cautiously, if at all, with other halogenated hydrocarbon anesthetics such as halothane. Prophylactic administration of lidocaine or prophylactic IV administration of propranolol 0.05 mg/kg may protect against ventricular irritability if epinephrine is used during anesthesia with a halogenated hydrocarbon anesthetic. In one study, arrhythmias occurring after parenteral use of epinephrine during general anesthesia responded promptly to IV propranolol 0.05 mg/kg.
Other Drugs
Epinephrine should not be used in patients receiving high dosage of other drugs such as digitalis glycosides which can sensitize the heart to arrhythmias.
Tricyclic antidepressants (e.g., imipramine), some antihistamines (especially diphenhydramine, tripelennamine, and dexchlorpheniramine) and thyroid hormones may potentiate the effects of epinephrine, especially on heart rhythm and rate. Potentiation by tricyclic antidepressants or antihistamines may result from inhibition of tissue uptake of epinephrine or norepinephrine or by increased adrenoreceptor sensitivity to epinephrine. Although monoamine oxidase (MAO) is one of the enzymes responsible for epinephrine metabolism, MAO inhibitors do not markedly potentiate the effects of epinephrine.
Pharmacology
Epinephrine constricts conjunctival blood vessels, contracts the dilator muscle of the pupil, and may dilate the pupil after topical application to the conjunctiva or injection into the anterior chamber of the eye. In normal eyes, epinephrine is a poor mydriatic. However, the drug produces effective mydriasis when the permeability of the eye is increased during surgery or trauma, after postganglionic sympathetic denervation (as in Horner’s syndrome or Raeder’s syndrome), and in patients with chronic renal hypertension, hyperthyroidism, or certain cases of glaucoma. Epinephrine produces only slight relaxation of the ciliary muscle so that cycloplegia does not occur.
Following topical application to the conjunctiva of patients with open-angle glaucoma, epinephrine lowers intraocular pressure (IOP) and causes brief mydriasis and vasoconstriction. The drug has only a slight effect in the normal eye. The exact mechanism has not been fully elucidated, but epinephrine appears to lower IOP principally by stimulating α- and/or β2-adrenergic receptors, resulting in an increase in both pressure-independent (uveoscleral) and, to a lesser extent, pressure-dependent (trabecular) aqueous humor outflow. In one study, IOP was lowered by the drug in concentrations as low as 0.12%; improvement in outflow facility occurred only when concentrations of 1% were used. Outflow facility may increase after only 1 dose of a 1 or 2% solution of the drug; however, it has also been reported that this effect may occur only after several months of continuous therapy. Rarely, a temporary but clinically important increase in IOP and impairment of outflow facility (even when the angle of the eye remained open) have occurred in patients with glaucoma when epinephrine was used initially without a miotic. This may result from release of pigment particles, presumably from the iris, into the aqueous humor. Although epinephrine has generally been thought to decrease aqueous humor formation, recent evidence suggests that the drug increases aqueous humor formation, an action that partially counteracts its IOP-lowering effect.
EPINEPHrine (Mydriatic) (EENT) Pharmacokinetics
Absorption
Following topical application of epinephrine to the conjunctiva, a reduction in IOP may occur within 1 hour, reach a maximum in 4–8 hours, and may persist for 12–24 hours or more. Mydriasis may occur within a few minutes and may persist for several hours. Vasoconstriction usually occurs within 5 minutes after topical administration or intraocular injection of epinephrine and generally lasts less than 1 hour.
Occasionally, enough epinephrine may be absorbed following topical application to the conjunctiva or intraocular injection to cause systemic sympathomimetic effects.
Distribution
Following topical application of radiolabeled epinephrine to the eye in rabbits, highest concentrations of the drug in tissues and fluids other than the eye occurred in the pituitary gland, with lower concentrations in the intestine, fat, adrenal gland, kidney, heart, lung, spleen, ovary, pancreas, liver, uterus, muscle, brain, and serum. In humans, systemically absorbed epinephrine crosses the placenta but not the blood-brain barrier. Systemically absorbed epinephrine distributes into milk.
Elimination
The pharmacologic actions of epinephrine are terminated mainly by uptake and metabolism in sympathetic nerve endings. Circulating drug is metabolized in the liver and other tissues by a combination of reactions involving the enzymes catechol-O-methyltransferase (COMT) and monoamine oxidase (MAO). The major metabolites are metanephrine and 3-methoxy-4-hydroxymandelic acid (vanillylmandelic acid, VMA), both of which are inactive. Epinephrine and its metabolites are excreted by the kidneys.
Chemistry and Stability
Chemistry
Epinephrine is an endogenous catecholamine which is the active principle of the adrenal medulla. Both the endogenous substance and the official preparation are the levorotatory isomer which is 15 times more active than is the dextrorotatory isomer.
Epinephrine may be obtained from the adrenal glands of animals or prepared synthetically; drug obtained from animals may contain up to 4% norepinephrine. Epinephrine occurs as a white to nearly white, microcrystalline powder or granules. Epinephrine is only very slightly soluble in water but readily forms water soluble salts (such as the hydrochloride and bitartrate) with acids. Epinephrine also forms a soluble epinephryl borate complex. Epinephrine injection is a nearly colorless, slightly acidic aqueous solution prepared with the aid of hydrochloric acid and contains the drug as the hydrochloride salt. The injection has a pH of 2.5–5. Ophthalmic solutions of epinephrine hydrochloride or bitartrate are acidic; those containing epinephryl borate have a pH of 5.5–7.6.
Stability
Epinephrine, epinephrine salts, and solutions containing the drugs gradually darken on exposure to light and air and must be stored in tight, light-resistant containers. In some commercially available injections, the air has been replaced with nitrogen to avoid oxidation. Withdrawal of doses from multiple-dose vials introduces air into the vials, subjecting the remaining epinephrine to oxidation. Oxidation of epinephrine imparts first a pink, then a brown color. Epinephrine preparations must not be used if they are discolored or contain a precipitate. Commercially available epinephrine preparations contain a variety of preservatives including antioxidants, bacteriostatic agents, and chelating agents. These preparations vary in stability, depending on the form in which epinephrine is present and on the preservatives used. The manufacturer’s directions should be followed with respect to storage requirements for each product.
Epinephrine is readily destroyed by oxidizing agents or alkalies including sodium bicarbonate, halogens, permanganates, chromates, nitrates, nitrites, and salts of easily reducible metals such as iron, copper, and zinc. Epinephrine solutions have been reported to be physically incompatible with many drugs, but the compatibility depends on several factors (e.g., concentration of the drugs, specific diluents used, resulting pH, temperature). Specialized references should be consulted for specific compatibility information. Epinephrine may be mixed with 0.9% sodium chloride injection but is incompatible with 5% sodium chloride injection.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Ophthalmic |
Solution |
0.5% (of epinephrine) |
Epifrin |
Allergan |
|
1% (of epinephrine) |
Epifrin |
Allergan |
||
|
Glaucon |
Alcon |
|||
|
2% (of epinephrine) |
Epifrin |
Allergan |
||
|
Glaucon |
Alcon |
|||
|
Parenteral |
Injection |
0.1 mg/mL (1:10,000) (of epinephrine)* |
Epinephrine Hydrochloride Injection |
|
|
1 mg/mL (0.1% or 1:1000) (of epinephrine)* |
Adrenalin Chloride Solution |
Monarch |
||
|
Epinephrine Hydrochloride Injection |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Ophthalmic |
Solution |
1% (approximately equivalent to epinephrine 0.5%) with Pilocarpine Hydrochloride 1% |
E-Pilo-1 |
Novartis |
|
P1E1 |
Alcon |
|||
|
1% (approximately equivalent to epinephrine 0.5%) with Pilocarpine Hydrochloride 2% |
E-Pilo-2 |
Novartis |
||
|
P2E1 |
Alcon |
|||
|
1% (approximately equivalent to epinephrine 0.5%) with Pilocarpine Hydrochloride 3% |
P3E1 |
Alcon |
||
|
1% (approximately equivalent to epinephrine 0.5%) with Pilocarpine Hydrochloride 4% |
E-Pilo-4 |
Novartis |
||
|
P4E1 |
Alcon |
|||
|
1% (approximately equivalent to epinephrine 0.5%) with Pilocarpine Hydrochloride 6% |
E-Pilo-6 |
Novartis |
||
|
P6E1 |
Alcon |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Ophthalmic |
Solution |
0.5% (of epinephrine) |
Epinal |
Alcon |
|
1% (of epinephrine) |
Epinal |
Alcon |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions January 20, 2020. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Frequently asked questions
- Can you use an expired EpiPen in an emergency?
- Norepinephrine vs epinephrine: what's the difference?
- Can you bring an EpiPen on a plane?
- What's the mechanism of action for epinephrine?
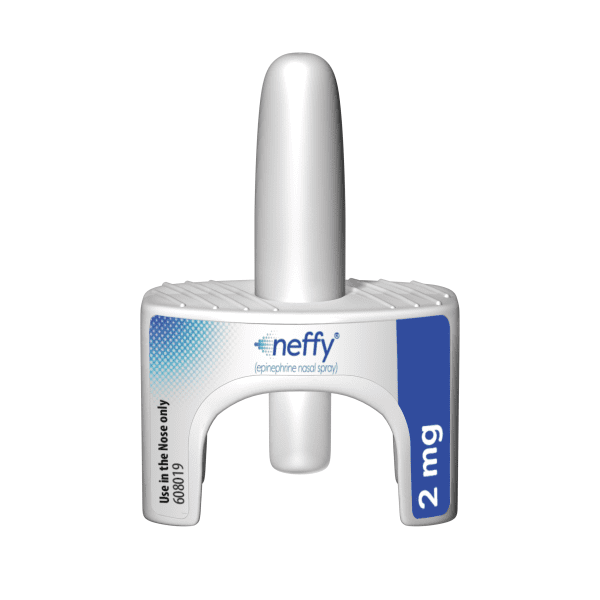
- What is Neffy (nasal epinephrine)?
- How much does Auvi-Q cost compared to EpiPen?
More about epinephrine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (57)
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: adrenergic bronchodilators
- Breastfeeding
Patient resources
Professional resources
- EPINEPHrine Bitartrate, EPINEPHrine Hydrochloride, Epinephryl Borate (Mydriatic) (EENT) monograph
- EPINEPHrine Hydrochloride (Vasoconstrictor) (EENT) (AHFS Monograph)
- Epinephrine (AHFS Monograph)
- Epinephrine Concentrate Injection (FDA)
- Epinephrine Injection (FDA)
Other brands
EpiPen, Adrenalin, Auvi-Q, Primatene Mist, ... +4 more