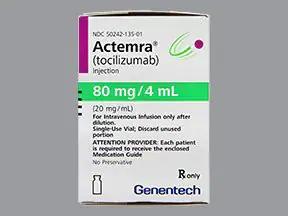
Actemra ACTPen
Generic name: tocilizumab [ TOE-si-LIZ-oo-mab ]
Brand names: Actemra, Actemra ACTPen
Drug class: Interleukin inhibitors
What is Actemra ACTPen?
Actemra ACTPen is used in adults to treat:
-
moderate to severe rheumatoid arthritis after at least one other medicine has been used and did not work;
-
giant cell arteritis, (inflammation in the lining of the blood vessels that carry blood from your heart to other parts of your body);
-
to slow the decline in lung function caused by scleroderma with interstitial lung disease; and
-
coronavirus disease 2019 (COVID-19) in hospitalized people who receive steroid medicine and require supplemental oxygen, a ventilator, or ECMO (a heart-lung machine that helps increase oxygen in the blood).
Actemra ACTPen is used in adults and children 2 years and older to treat:
-
polyarticular or systemic juvenile idiopathic arthritis ("Still disease"); and
-
severe cytokine release syndrome (CRS, an overactive immune response to certain blood cell treatments for cancer).
The US Food and Drug Administration (FDA) has authorized emergency use of tocilizumab with steroid medicine to treat children at least 2 years old who are hospitalized with COVID-19 and using supplemental oxygen, a ventilator, or ECMO (a heart-lung machine that helps increase oxygen in the blood).
Actemra ACTPen may also be used for purposes not listed in this medication guide.
Actemra ACTPen side effects
Get emergency medical help if you have signs of an allergic reaction: hives; chest pain, difficulty breathing, feeling like you might pass out; swelling of your face, lips, tongue, or throat.
Actemra ACTPen may cause serious side effects. Call your doctor at once if you have:
-
severe stomach cramps, bloating, diarrhea or constipation;
-
unusual bleeding--nosebleeds, bleeding gums, abnormal vaginal bleeding, any bleeding that will not stop, blood in your urine or stools, coughing up blood or vomit that looks like coffee grounds;
-
liver problems--loss of appetite, right-sided stomach pain, vomiting, confusion, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
signs of infection--fever, chills, aches, skin sores, diarrhea, burning when you urinate;
-
signs of tuberculosis: cough, shortness of breath, night sweats, loss of appetite, weight loss, and feeling very tired; or
-
signs of perforation (a hole or tear) in your stomach or intestines--fever, ongoing stomach pain, change in bowel habits.
Common side effects of Actemra ACTPen may include:
-
runny or stuffy nose, sinus pain, sore throat;
-
headache;
-
increased blood pressure;
-
abnormal liver function tests; or
-
pain, swelling, burning, or irritation where an injection was given.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
prednisone, naproxen, methotrexate, hydroxychloroquine, Humira, Paxlovid, Enbrel
Warnings
You may get infections more easily, even serious or fatal infections. Call your doctor if you have a fever, chills, aches, tiredness, cough, shortness of breath, skin sores, diarrhea, weight loss, or burning when you urinate.
Actemra ACTPen may also cause a perforation (a hole or tear) in your stomach or intestines. Tell your doctor if you have a fever and stomach pain with a change in your bowel habits.
Actemra ACTPen may also cause liver problems. Tell your doctor right away if you have right-sided stomach pain, vomiting, loss of appetite, tiredness, dark urine, clay-colored stools, or yellowing of your skin or eyes.
Before taking this medicine
You should not use Actemra ACTPen if you are allergic to it.
Tell your doctor if you have any signs of infection such as fever, chills, cough, body aches, tiredness, open sores or skin wounds, diarrhea, stomach pain, weight loss, painful urination, or coughing up blood.
Tell your doctor if you've had or been exposed to tuberculosis, or if you recently traveled. Some infections are more common in certain parts of the world, and you may have been exposed during travel.
Tell your doctor if you have ever had:
-
an active or chronic infection;
-
diverticulitis, ulcers in your stomach or intestines;
-
a nerve-muscle disease such as multiple sclerosis;
-
diabetes;
-
HIV, or a weak immune system;
-
hepatitis B (or if you are a carrier of the virus);
-
cancer; or
-
if you have received or are scheduled to receive any vaccines.
Using Actemra ACTPen may increase your risk of developing other cancers. Ask your doctor about this risk.
Tell your doctor if you are pregnant or breastfeeding.
Tell your baby's doctor if you used Actemra ACTPen during pregnancy. It could affect your baby's vaccination schedule during the first months of life. Your name may be listed on a pregnancy registry to track the effects of tocilizumab on the baby.
How is Actemra ACTPen given?
Before you use Actemra ACTPen, your doctor may test you for tuberculosis or other infections.
Follow all directions on your prescription label and read all medication guides or instruction sheets. Use the medicine exactly as directed.
Actemra ACTPen is injected under the skin or into a vein. Actemra ACTPen is usually given every 1 to 4 weeks for most conditions. For CRS, only one dose is usually given.
When injected into a vein, this medicine is given slowly for about 1 hour.
Read and carefully follow any Instructions for Use provided with the medicine. Ask your doctor or pharmacist if you don't understand how to use an injection.
Prepare an injection only when you are ready to give it. Call your pharmacist if the medicine looks cloudy, has changed colors, or has particles in it.
Your healthcare provider will show you where to inject Actemra ACTPen. Do not inject into the same place two times in a row.
Do not reuse a needle, syringe, or autoinjector. Place them in a puncture-proof "sharps" container and dispose of it following state or local laws. Keep out of the reach of children and pets.
You may get infections more easily, even serious or fatal infections. You will need frequent medical tests.
If you've had hepatitis B, it may come back or get worse. You may need liver function tests while using this medicine and for several months after you stop.
Tell your doctor if you have a planned surgery.
Use all your medications as directed. Do not change your dose or stop using a medicine without your doctor's advice.
Store this medicine in the original carton in a refrigerator. Protect from moisture and light. Do not freeze. Throw away any prefilled syringes not used before the expiration date on the medicine label.
After removed from the refrigerator, the prefilled syringe and autoinjector can be stored up to 2 weeks at or below 86 F (30 C). Throw away the prefilled syringe or autoinjector after one use, even if there is still medicine left inside.
Actemra ACTPen can have long-lasting effects on your body. You may need certain medical tests every 6 months after you stop using this medication.
What happens if I miss a dose?
Call your doctor for instructions if you miss a dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while receiving Actemra ACTPen?
Avoid receiving a "live" vaccine, or you could develop a serious infection. Live vaccines include measles, mumps, rubella (MMR), rotavirus, typhoid, yellow fever, varicella (chickenpox), and zoster (shingles).
You may still be able to receive a yearly flu shot, or an "inactivated" or other vaccine to prevent diseases such as hepatitis, meningitis, pneumonia, shingles, HPV, or whooping cough. Ask your doctor before getting any vaccine.
Avoid being near people who are sick or have infections. Tell your doctor at once if you develop signs of infection.
What other drugs will affect Actemra ACTPen?
Sometimes it is not safe to use certain medications at the same time. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective.
Tell your doctor about all your other medicines, especially other medicines to treat rheumatoid arthritis, such as:
-
abatacept, etanercept;
-
anakinra; or
-
adalimumab, certolizumab, golimumab, infliximab, or rituximab.
This list is not complete and many other drugs may affect Actemra ACTPen. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Popular FAQ
Most people take Actemra for up to 1 year to treat Giant cell arteritis (GCA), although the exact length of time you will take it for depends on how well you tolerate any side effects of Actemra, if it works for you, and how long it continues to work for. Actemra will work within 3 to 6 months, if it is going to work at all, although some people may experience some symptom relief as early as 2 weeks after starting treatment. Actemra is given by subcutaneous injection once every 1 to 2 weeks.
Actemra stays in your system for a very long time, up to 3.5 months or 107 days. This is calculated by using the half-life of Actemra (also called the t1/2), which is the time it takes for 50% of a medicine to leave the body. The t1/2 for Actemra is 21.5 days. Experts have determined that it takes 4 to 5 half-lives for a medicine to be completely eliminated by the body, which works out to be 86 to 107 days (2.9 to 3.5 months) for Actemra.
Actemra infusion may be used to treat several different conditions that have inflammation as a common characteristic, such as:
- Rheumatoid Arthritis
- Giant Cell Arteritis
- Systemic Sclerosis-Associated Interstitial Lung Disease
- Polyarticular Juvenile Idiopathic Arthritis
- Systemic Juvenile Idiopathic Arthritis
- Cytokine Release Syndrome
- COVID-19 in hospitalized adults who are receiving corticosteroids plus supplemental oxygen, on non-invasive or invasive mechanical ventilation, or receiving extracorporeal membrane oxygenation (ECMO).
Yes, Actemra (tocilizumab) can cause a small amount of weight gain; in one trial, the amount of weight gained ranged from 0kg to 2kg over 24 to 72 weeks.
Experts are unsure why Actemra causes people to gain weight, but this same study reported that the leptin–adiponectin ratio and levels of adiponectin, leptin, and resistin increased significantly after 24 weeks of tocilizumab treatment. Increased levels of pro-inflammatory adipokines such as interleukin (IL)-1β, IL-6, TNFα, and leptin, and decreased levels of anti-inflammatory adipokines, such as adiponectin, in obesity produce a chronic state of low-grade inflammation which promotes the development of insulin resistance and type-2 diabetes, hypertension, atherosclerosis, and other cardiovascular diseases, and some types of cancer.
If you’re prescribed antibiotics, speak to your rheumatology team or doctor right away and cancel your Actemra infusion or stop using your prefilled ACTPen autoinjector until you have finished the antibiotics and your infection has cleared up.
People treated with Actemra are more likely to develop serious infections than people not prescribed Actemra, and these infections are more likely to result in hospitalization, and in some cases, death. You are at an even higher risk if you are also taking other immunosuppressants such as methotrexate or corticosteroids.
Acetmra is not a TNF inhibitor it is an interleukin inhibitor. Actemra works by binding to interleukin-6 (IL-6) receptors. Interleukin 6 is considered one of the most important cytokines – these are signaling molecules that aid cell to cell communication during an immune response and stimulate the movement of cells towards sites of inflammation, infection, or trauma. IL-6 is also produced by synovial and endothelial cells within a joint. By binding to IL-6 receptors, Actemra decreases inflammation in conditions such as rheumatoid arthritis.
TNF inhibitors block the activity of a different, but equally as important, cytokine, called tumor necrosis factor-alpha (TNF-alpha). IL-6 and TNF-alpha are the main factors responsible for the induction of inflammatory proteins such as C-reactive protein and the inflammatory state.
Interleukin-6, TNF-alpha, and also interleukin-1 are known as proinflammatory cytokines and are elevated in most, if not all inflammatory states.
Actemra is used to treat several different conditions that have inflammation as a common characteristic, such as Rheumatoid arthritis (RA), Giant Cell Arteritis (GCA), Systemic Sclerosis-Associated Interstitial Lung Disease (SSc-ILD), Polyarticular Juvenile Idiopathic arthritis (PJIA), Systemic Juvenile Idiopathic arthritis (SJIA), Cytokine Release Syndrome (CRS), and COVID-19.
Continue readingBefore receiving Actemra, let your health care provider know if you have any of the following:
- An infection or symptoms of an infection, such as a fever, sweating or chills, shortness of breath, a rash or sores, fatigue, muscle aches, diarrhea, nausea or vomiting, a cough, or pain when urinating
- Diabetes, HIV, hepatitis B, or a weak immune system
- Tuberculosis (TB)
- Have lived in or recently traveled to certain parts of the U.S (such as the Ohio and Mississippi River valleys and the Southwest) where there is a higher risk of certain fungal infections such as histoplasmosis, coccidioidomycosis, or blastomycosis
- Diverticulitis, ulcers, or tears (perforations) of your stomach or intestines
- Liver problems or symptoms that may suggest liver problems, such as yellowing of your skin or the whites of your eyes (jaundice), appetite loss, abdominal swelling and pain on the right side of your stomach area, light-colored stools, or dark "tea-colored" urine
- Cancer of any type
- Multiple sclerosis or any other condition that affects your nervous system.
Also, let your doctor know if:
- You have recently received or are scheduled to receive a vaccine
- Recent laboratory tests detected low neutrophils, low platelets, or your liver function results were high
- You plan to have surgery or a medical procedure
- You are pregnant or plan to become pregnant or are breastfeeding
- You take any other medications, including prescription, over-the-counter medicines, vitamins, and herbal supplements.
More FAQ
More about Actemra (tocilizumab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (45)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- FDA approval history
- Drug class: interleukin inhibitors
- Breastfeeding
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 9.01.