Triptorelin (Monograph)
Brand names: Trelstar, Triptodur
Drug class: Gonadotropins
VA class: AN500
Chemical name: 6-d-Tryptophan luteinizing hormone-releasing factor (pig)
Molecular formula: C64H82N18O13
CAS number: 57773-63-4
Introduction
Antineoplastic agent; synthetic decapeptide analog of gonadotropin-releasing hormone (GnRH, luteinizing hormone-releasing hormone, gonadorelin); structurally related to leuprolide and goserelin.
Uses for Triptorelin
Prostate Cancer
Palliative treatment of advanced prostate cancer.
Precocious Puberty
Treatment of central precocious puberty (CPP) in pediatric patients ≥2 years of age (designated an orphan drug by FDA for this use).
GnRH analogs are considered the therapy of choice for this condition and generally have supplanted medroxyprogesterone in this form of precocity.
GnRH analogs are ineffective as primary therapy in the treatment of GnRH-independent† [off-label] (peripheral; gonadal steroid secretion is independent of gonadotropin secretion) precocious puberty, including familial male precocious puberty (testotoxicosis), congenital virilizing adrenal hyperplasia (e.g., secondary to steroid 21-hydroxylase, 11β-hydroxylase, or 3β-hydroxysteroid dehydrogenase deficiency), and McCune-Albright syndrome.
Breast Cancer
Use of ovarian suppression in combination with endocrine therapy (i.e., anastrozole, exemestane, letrozole, tamoxifen)† [off-label] as adjuvant therapy in premenopausal women with early-stage hormone receptor-positive breast cancer† [off-label] may be considered a reasonable choice (accepted).
Related/similar drugs
Erleada, Lupron Depot, estradiol, tamoxifen, Xtandi, leuprolide, Zytiga
Triptorelin Dosage and Administration
Administration
IM Administration
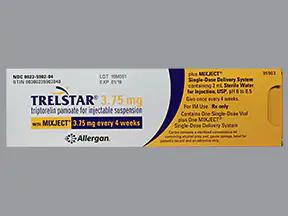
Administer 3.75-mg formulation of triptorelin pamoate (Trelstar) by IM injection every 4 weeks (28 days), 11.25-mg formulation (Trelstar) every 12 weeks, or the 22.5-mg extended-release formulation (Trelstar, Triptodur) every 24 weeks.
Inject IM into either buttock; manufacturer of Triptodur also states that the drug may be injected into either thigh. Alternate injection sites periodically. Administer under the supervision of a qualified clinician.
Reconstitution
Reconstitute powder just prior to administration.
Add contents of prefilled syringe (2 mL of sterile water for injection) supplied by manufacturer to a vial containing the powder according to the manufacturer’s instructions; do not reconstitute with other diluents. Mix well to disperse particles and obtain a uniform, milky suspension.
Withdraw entire contents of vial and use immediately.
Dosage
Available as triptorelin pamoate; dosage is expressed in terms of triptorelin.
Pediatric Patients
Central Precocious Puberty
IM
≥2 years of age: 22.5 mg every 24 weeks as the 22.5-mg formulation.
Adults
Prostate Cancer
IM
3.75 mg every 4 weeks (28 days) as the 3.75-mg formulation, 11.25 mg every 12 weeks as the 11.25-mg formulation, or 22.5 mg every 24 weeks as the 22.5-mg formulation. Dosage strengths are not additive; select dosage and formulation based on desired dosing schedule.
Periodically determine serum testosterone concentrations to monitor therapeutic response.
Early-stage Breast Cancer† [off-label]
IM
3.75 mg every 4 weeks has been used in combination with endocrine therapy† [off-label].
Special Populations
Hepatic Impairment
No special population recommendation at this time.
Renal Impairment
No special population recommendation at this time.
Cautions for Triptorelin
Contraindications
-
Known hypersensitivity to triptorelin or any other ingredient in the formulation, other GnRH agonists, or GnRH.
-
Known or suspected pregnancy. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Warnings/Precautions
Sensitivity Reactions
Hypersensitivity Reactions
Anaphylactic shock, hypersensitivity, and angioedema reported. If such reactions occur, discontinue the drug immediately and provide supportive and symptomatic care.
Initial Worsening of Hormone-dependent Disease
Increased gonadotropin and sex steroid concentrations and subsequent transient increase in clinical signs and symptoms of puberty (e.g., vaginal bleeding) may occur during initial weeks of therapy or following subsequent doses in pediatric patients with precocious puberty.
Possible worsening of signs and/or symptoms of prostate cancer and/or development of new manifestations (e.g., bone pain, neuropathy, hematuria, urethral or bladder outlet obstruction) due to transient increase in serum testosterone concentrations during initial weeks of therapy.
Possible spinal cord compression contributing to weakness or paralysis in patients with prostate cancer; possibly fatal. If spinal cord compression or renal impairment develops, institute standard treatment of these complications; consider immediate orchiectomy in extreme cases.
Increased risk of neurologic and/or GU complications during initial therapy in patients with prostate cancer and metastatic vertebral lesions and/or urinary tract obstruction. Observe such patients closely during initial weeks of therapy.
Hyperglycemia
Possible hyperglycemia and increased risk of diabetes in patients receiving GnRH agonists for treatment of prostate cancer. Studies evaluating risk of diabetes in women and children receiving GnRH agonists not performed to date.
Evaluate patients for risk factors for diabetes and carefully weigh benefits and risks of GnRH agonist therapy before selecting treatment for prostate cancer.
Periodically monitor blood glucose and/or HbA1c in patients receiving GnRH agonists for treatment of prostate cancer. Manage hyperglycemia or diabetes according to current standards of care.
Concomitant Diseases
Patients with metastatic vertebral lesions and/or upper or lower urinary tract obstruction should be observed closely during the first few weeks of therapy.
Cardiovascular Effects
Thromboembolic events (e.g., PE, cerebrovascular accidents, MI, DVT, TIA, thrombophlebitis) reported. Possible increased risk of cardiovascular disease (e.g., MI, sudden cardiac death, stroke) in patients receiving GnRH agonists for treatment of prostate cancer. Studies evaluating risk of cardiovascular disease in women and children receiving GnRH agonists not performed to date.
Evaluate patients for cardiovascular risk factors and carefully weigh benefits and risks of GnRH agonist therapy before selecting treatment for prostate cancer.
Monitor patients receiving GnRH agonists for manifestations of cardiovascular disease; manage cardiovascular disease according to current standards of care.
Risk of prolonged QT interval associated with long-term androgen deprivation therapy. Carefully weigh benefits and risks of androgen deprivation therapy in patients with congenital long QT syndrome, electrolyte abnormalities, or CHF and in patients taking drugs known to prolong the QT interval.
Nervous System Effects
Emotional lability (e.g., crying, irritability, impatience, anger, aggression) has been reported during postmarketing experience in pediatric patients with precocious puberty. Depression (including rare reports of suicidal ideation and suicide attempts) also reported during postmarketing experience in pediatric patients; most patients had a history of psychiatric illness or comorbidities associated with an increased risk of depression. Monitor for new or worsening neuropsychiatric symptoms during therapy.
Convulsions also reported during postmarketing experience in pediatric patients with precocious puberty. Convulsions occurred in patients with or without predisposing factors for convulsions.
Laboratory Test Interferences
Suppression of pituitary gonadal system may occur following chronic or continuous administration of triptorelin. Erroneous results may occur when diagnostic tests of pituitary gonadotropic and gonadal function are obtained during or after discontinuance of therapy with triptorelin. Normal function of the pituitary gonadal system usually restored within 6–12 months after discontinuance of drug.
Fetal/Neonatal Morbidity and Mortality
Expected hormonal changes increase the risk for pregnancy loss and fetal harm when administered to a pregnant woman. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Pituitary Apoplexy
Pituitary apoplexy, a clinical syndrome resulting from infarction of the pituitary gland, reported rarely. Most cases occur within 2 weeks of the first dose, sometimes within the first hour. If manifestations (e.g., sudden headache, vomiting, visual changes, ophthalmoplegia, altered mental status, sometimes cardiovascular collapse) occur, immediate medical attention required. In most cases, pituitary adenoma diagnosed.
Impairment of Fertility
May impair male fertility.
Specific Populations
Pregnancy
May cause fetal harm. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Not known whether distributed into milk, affects milk production, or affects nursing infants. Consider known benefits of breast-feeding along with mother's clinical need for triptorelin and any potential adverse effects of the drug or the underlying maternal condition on the infant.
Pediatric Use
Safety and efficacy not established in children <2 years of age.
Safety and efficacy in pediatric patients with CPP established in an open-label, noncomparative study that included 44 pediatric patients 2–9 years of age.
Geriatric Use
Men with metastatic prostate cancer: Studies conducted principally in patients ≥65 years of age, since prostate cancer occurs mainly in an older patient population.
Common Adverse Effects
Men with metastatic prostate cancer (Trelstar): Hot flushes (flashes), skeletal pain, neuropathy, hematuria, urethral or bladder outlet obstruction, impotence, headache, pain at injection site, leg pain and edema, dysuria, hypertension.
Also observed in adults receiving 11.25-mg formulation (Trelstar): Decreased hemoglobin concentrations and erythrocyte counts, increased BUN, increased serum concentrations of glucose, AST, ALT, and alkaline phosphatase.
Also observed in adults receiving 22.5-mg formulation (Trelstar): Decreased hemoglobin concentrations, increased serum glucose and hepatic aminotransferase (transaminase) concentrations.
Pediatric patients ≥2 years of age with precocious puberty (Triptodur): Injection site reactions, vaginal bleeding, hot flush, headache, cough, infection (i.e., bronchitis, gastroenteritis, influenza, nasopharyngitis, otitis externa, pharyngitis, sinusitis, upper respiratory infection).
Drug Interactions
Metabolism unlikely to involve CYP enzymes.
In vitro, does not inhibit CYP isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A4/5 or induce CYP isoenzymes 1A2 or 3A4/5.
Poor substrate of P-glycoprotein (P-gp). In vitro, does not inhibit P-gp.
Drugs That Induce Hyperprolactinemia
Potential pharmacologic interaction (possible decrease in triptorelin efficacy due to decreased number of GnRH receptors) with drugs such as antipsychotic agents, methyldopa, metoclopramide, and reserpine. Concomitant use not recommended.
Triptorelin Pharmacokinetics
Absorption
Bioavailability
Men with prostate cancer: Following IM administration, peak plasma concentrations usually are attained within 1–3 hours.
Children 2–9 years of age with CPP: Following IM administration, peak plasma concentrations are attained in 4 hours.
Distribution
Extent
Not known whether triptorelin is distributed into milk.
Plasma Protein Binding
No evidence that triptorelin binds to plasma proteins.
Elimination
Metabolism
Metabolism is unknown; involvement of CYP enzymes is unlikely. No metabolites identified to date.
Elimination Route
Hepatic and renal elimination.
Half-life
Approximately 3 hours.
Special Populations
In men with hepatic impairment or moderate or severe renal impairment, AUC increased 2- to 4-fold compared with healthy males.
Stability
Storage
Parenteral
Powder for Injection (Trelstar, Triptodur)
20–25°C. Do not freeze.
Actions
-
Potent inhibitor of gonadotropin secretion when given continuously in therapeutic doses; greater activity than naturally occurring GnRH.
-
Transient surge in circulating levels of LH, FSH, testosterone, and estradiol observed after initial administration. Sustained decreases in LH and FSH secretion and reduced testicular and ovarian steroidogenesis observed following chronic, continuous administration (generally 2–4 weeks after initiation of therapy).
-
Reduction of serum testosterone in males comparable to effects achieved after surgical castration; results in inactivation of physiologic functions and tissues dependent on testosterone. These effects usually are reversible after cessation of therapy.
Advice to Patients
-
Importance of taking triptorelin exactly as prescribed.
-
Importance of informing patients with prostate cancer that serum testosterone concentrations may increase after the initial dose. Risk of worsening symptoms (e.g., bone pain, spinal cord injury, hematuria, urethral or bladder outlet obstruction) of prostate cancer during initial weeks of therapy. Increased serum testosterone concentrations and associated symptoms should decline 3–4 weeks later. Importance of promptly reporting weakness or paresthesia of the lower limbs and/or worsening of urinary symptoms to clinicians.
-
Importance of informing caregivers of patients with CPP that signs of puberty (e.g., vaginal bleeding) may occur during the initial weeks of therapy. Importance of reporting these symptoms to clinicians if they persist beyond the second month.
-
Importance of informing caregivers of patients with CPP that symptoms of emotional lability (e.g., crying, irritability, impatience, anger, aggression) may occur in pediatric patients receiving GnRH agonists.
-
Importance of informing caregivers of patients with CPP that convulsions may occur in pediatric patients receiving GnRH agonists. Risk may be increased in patients with a history of convulsions, epilepsy, cerebrovascular disorders, CNS anomalies or tumors, and those receiving concomitant drugs known to lower seizure threshold.
-
Risk of anaphylactoid and other sensitivity reactions.
-
Risk of diabetes or loss of glycemic control in adults with preexisting diabetes. Importance of undergoing recommended monitoring of blood glucose or HbA1c concentrations.
-
Possibility of increased risk of MI, sudden cardiac death, and stroke in men receiving GnRH agonists for the treatment of prostate cancer. Importance of being monitored for manifestations of cardiovascular disease.
-
Possibility of impotence in men with prostate cancer.
-
Risk of impaired male fertility.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of avoiding use of the drug during pregnancy. If used during pregnancy, apprise of potential fetal hazard.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, for IM use only |
3.75 mg (of triptorelin) |
Trelstar (with Mixject) |
Allergan |
|
11.25 mg (of triptorelin) |
Trelstar (with Mixject) |
Allergan |
||
|
22.5 mg (of triptorelin) |
Trelstar (with Mixject) |
Allergan |
||
|
Triptodur |
Arbor |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions January 11, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
- How long can I take Trelstar (triptorelin) for prostate cancer?
- Why is triptorelin used for prostate cancer?
More about triptorelin
- Check interactions
- Compare alternatives
- Reviews (7)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: gonadotropin releasing hormones
- En español