Niacin (Vitamin) (Monograph)
Drug class: Vitamin B Complex
ATC class: A11HA01
VA class: VT103
CAS number: 98-92-0
Introduction
Niacin and niacinamide are water-soluble, B complex vitamins.
Uses for Niacin (Vitamin)
Niacin Deficiency and Pellagra
Niacin and niacinamide are used to prevent niacin deficiency and to treat pellagra. Some clinicians prefer niacinamide for the treatment of pellagra because it lacks vasodilating effects. Pellagra may result from dietary deficiency, isoniazid therapy, or from decreased conversion of tryptophan to niacin in Hartnup disease or carcinoid tumors. Whenever possible, poor dietary habits should be corrected, and many clinicians recommend administration of multivitamin preparations containing niacin in patients with vitamin deficiencies since poor dietary habits often result in concurrent deficiencies. Increased niacin requirements may be associated with hyperthyroidism, diabetes mellitus, cirrhosis, pregnancy, and lactation, but dietary niacin deficiency is rare in these patients.
Diagnosis of niacin deficiency can be aided by measuring urinary N-methylnicotinamide concentrations. Less than 0.5 mg of N-methylnicotinamide per gram of creatinine is excreted in niacin-deficient patients. In 24 hours, less than 2 mg of N-methylnicotinamide and its 6-pyridone derivative is excreted in urine in niacin-deficient patients. Occasionally, when a patient’s diagnosis is not clear, a trial of niacin may be used to diagnose niacin deficiency.
Dietary Requirements
The National Academy of Sciences (NAS) has issued a comprehensive set of Recommended Dietary Allowances (RDAs) as reference values for dietary nutrient intakes since 1941. In 1997, the NAS Food and Nutrition Board (part of the Institute of Medicine [IOM]) announced that they would begin issuing revised nutrient recommendations that would replace RDAs with Dietary Reference Intakes (DRIs). DRIs are reference values that can be used for planning and assessing diets for healthy populations and for many other purposes and that encompass the Estimated Average Requirement (EAR), the Recommended Dietary Allowance (RDA), the Adequate Intake (AI), and the Tolerable Upper Intake Level (UL).
The NAS has established an EAR and RDA for niacin for adults based principally on urinary excretion of niacin metabolites. The EAR and RDA for children and adolescents 1–18 years of age were established based on data in adults, since specific data in children and adolescents currently are unavailable. An AI has been set for infants up to 6 months of age based on the observed mean niacin intake of infants fed principally human milk. An AI for infants 6–12 months of age has been set based on the AI for younger infants and data from adults.
The principal goal of maintaining an adequate intake of niacin in the US and Canada is to prevent pellagra. While pellagra was common in the US in the early twentieth century in areas where corn or maize was the dietary staple, pellagra is no longer common in industrialized countries. In industrialized countries, pellagra occurs mainly in alcoholics and individuals with conditions that disrupt tryptophan pathways. Pellagra still occurs in India, China, and Africa. Adequate intake of niacin can be accomplished through consumption of foodstuffs. In the US, niacin principally is obtained from mixed dishes containing substantial portions of meat, fish, or poultry; poultry as an entree; enriched and whole grain breads and bread products; and fortified ready-to-eat cereals. Conversion of dietary tryptophan to niacin also contributes to niacin intake.
For specific information on currently recommended AIs and RDAs of niacin for various life-stage and gender groups, see Dosage: Dietary and Replacement Requirements, under Dosage and Administration.
Other Uses
Large doses of niacin are used as an antilipemic agent.
Large doses of niacin also have been used as adjunctive therapy for the treatment of conditions associated with deficient circulation (e.g., peripheral vascular disease, vascular spasm, migraine headache, Ménière’s syndrome, vertigo); however, the drug is not a substitute for appropriate medical or surgical treatments of these disorders. The efficacy of niacin in the treatment of these conditions has not been established, and well-controlled clinical studies demonstrating the usefulness of vasodilators, such as niacin, in the treatment of these disorders are not available. Because niacin causes flushing associated with warmth and tingling, the drug has a strong placebo effect.
Although niacin and niacinamide have not been shown by well-controlled trials to have therapeutic value, the drugs have been used for the management of schizophrenic disorder, drug-induced hallucinations, chronic brain syndrome, hyperkinesis, unipolar depression, motion sickness, alcohol dependence, livedoid vasculitis, acne, and leprosy.
Related/similar drugs
atorvastatin, rosuvastatin, ezetimibe, simvastatin, Lipitor, fenofibrate, Crestor
Niacin (Vitamin) Dosage and Administration
Administration
Niacin and niacinamide are administered orally.
Dosage
Dietary and Replacement Requirements
Because dietary tryptophan contributes to niacin intake, reference values for dietary intake in all life-stage groups except infants up to 6 months of age are expressed in terms of niacin equivalents. Niacin equivalents (NEs) are calculated as follows: 1 mg of NE = 1 mg of niacin = 60 mg of tryptophan.
The Adequate Intake (AI) (see Uses: Dietary Requirements) of niacin currently recommended by the National Academy of Sciences (NAS) for healthy infants up to 6 months of age is 2 mg of preformed niacin (0.3 mg/kg) daily. For infants 6–12 months of age, the NAS currently recommends an AI of 4 mg of NE (0.4 mg/kg) daily. The Recommended Dietary Allowance (RDA) of niacin currently recommended by NAS for healthy children 1–3, 4–8, or 9–13 years of age is 6, 8, or 12 mg of NE daily, respectively. In establishing the niacin dietary requirement in individuals 14 years of age or older, the NAS considered the requirement to be lower in women than men, based on women’s size and average energy utilization. The RDA of niacin recommended for boys 14–18 years of age is 16 mg of NE daily, and the RDA for girls 14–18 years of age is 14 mg of NE daily. The RDA for healthy men of all ages is 16 mg of NE daily, and the RDA for healthy women of all ages is 14 mg of NE daily.
The NAS states that these RDAs are not expected to be sufficient to meet the needs of persons with Hartnup disease, cirrhosis of the liver, or carcinoid syndrome, or those receiving long-term isoniazid therapy. Additional niacin also may be required in individuals with malabsorption syndrome and individuals undergoing hemodialysis or peritoneal dialysis.
During pregnancy, the need for niacin increases by about 10% to cover increased energy utilization and about 2 mg of NE daily to cover growth in maternal and fetal compartments. The RDA of niacin recommended by the NAS for pregnant women is 18 mg of NE daily. Niacin requirements in lactating women include the amount required to maintain niacin status, including the increased energy expenditure involved in milk production, and the amount required to replace the niacin secreted daily in human milk. The RDA of niacin recommended by NAS for lactating women is 17 mg of NE daily. Niacin intake higher than these RDAs may be needed by women who are pregnant with more than one fetus and mothers nursing more than one infant.
Pellagra and Hartnup Disease
For the treatment or prevention of pellagra, dosages of niacin and niacinamide are considered equivalent.
For the treatment of pellagra, the usual adult oral dosage of niacin or niacinamide is 300–500 mg daily in divided doses. For the management of Hartnup disease, the usual oral dosage of niacin is 50–200 mg daily. For the treatment of pellagra in children, the usual oral dosage of niacin or niacinamide is 100–300 mg daily in divided doses. In patients with pellagra, redness and swelling of the tongue disappear within 24–72 hours after initiation of niacin or niacinamide therapy. Mental symptoms and infections of the mouth and other mucous membranes clear rapidly. GI symptoms disappear within 24 hours; however, dermal lesions blanch and heal more slowly. Niacin and niacinamide do not affect the polyneuritis or cheilosis that frequently accompanies pellagra; these conditions are believed to be caused by concurrent deficiency of thiamine or riboflavin.
Vasodilation
As a vasodilator, oral niacin dosages of 100–150 mg 3–5 times daily have been used. Alternatively, niacin dosages of 300–400 mg as extended-release preparations every 12 hours have been given.
Cautions for Niacin (Vitamin)
Adverse Effects
Small oral doses of niacin or niacinamide are usually nontoxic. However, following larger doses of niacin, such as those used to treat pellagra and other disorders, flushing (especially of the face and neck), pruritus, sensation of burning, stinging or tingling of the skin, nausea, bloating, flatulence, hunger pains, vomiting, heartburn, diarrhea, increased sebaceous gland activity, hypotension, dizziness, tachycardia, syncope (perhaps psychogenic), vasovagal attacks, headache, and blurred vision have occurred. Within 2 weeks after initiating long-term, high-dose, oral niacin therapy, the flushing and skin sensations, increased sebaceous gland activity, and increased GI motility disappear in most patients. Some clinicians suggest that initiating therapy with low doses and then gradually increasing the dose will lessen these transient adverse effects; however, this is controversial. When high dosages are used, some manufacturers recommend the use of extended-release preparations to lessen adverse effects; however, there is no evidence that these preparations offer an advantage over conventional dosage forms.
During long-term use of large doses of niacin, rash, hyperpigmentation sometimes resembling acanthosis nigricans, dry skin, xerostomia, hyperuricemia occasionally precipitating gout, activation of peptic ulcer, toxic amblyopia, blurred vision, proptosis, loss of central vision secondary to an atypical form of cystoid macular edema, nervousness, panic, hyperglycemia and abnormal glucose tolerance, and glycosuria have occurred.
Abnormal liver function test results (including increased serum concentrations of bilirubin, AST [SGOT], ALT [SGPT], and LDH), jaundice, and chronic liver damage have occurred during niacin and niacinamide therapy. Abnormal prothrombin time and hypoalbuminemia have also been reported.
Precautions and Contraindications
Blood glucose concentration should be monitored periodically in patients receiving niacin or niacinamide, especially early in the course of therapy. Dosage requirements for antidiabetic agents (e.g., insulin, oral sulfonylureas) may change in diabetic patients.
Liver function should be determined periodically (especially early in the course of therapy) in patients receiving long-term niacin or niacinamide therapy in dosages that greatly exceed the physiologic requirement. Large doses of niacin should be used with caution in patients with coronary artery disease, since an increased incidence of atrial and other cardiac arrhythmias has been reported in one study in patients who received the drug to lower serum lipid concentrations.
Large doses of niacin or niacinamide should be administered with caution to patients with gallbladder disease or a history of jaundice or liver disease, diabetes mellitus, gout, peptic ulcer, or allergy.
Niacin and niacinamide are contraindicated in patients with liver disease, active peptic ulcer, or hypersensitivity to the drugs. Niacin is also contraindicated in patients with arterial hemorrhaging or severe hypotension.
Pregnancy and Lactation
Pregnancy
Administration of supplementary doses of niacin during pregnancy has not been associated with any adverse effects to the mother or fetus. However, toxicologic studies have not been performed with large doses of niacin, and large doses of the drug should not be used in women who are or may become pregnant unless the possible benefits outweigh the potential risks to the fetus.
Lactation
Administration of supplementary doses of niacin during lactation has not been associated with any adverse effects to the mother or fetus.
Drug Interactions
Niacin reportedly potentiates the hypotensive effect of ganglionic blocking drugs.
Long-term administration of isoniazid may interfere with the conversion of dietary tryptophan to niacin and increase the requirement of niacin.
Laboratory Test Interferences
Niacin may produce fluorescent substances that cause false elevations in some fluorometric determinations of urinary catecholamines. Niacin may also give false-positive reactions with cupric sulfate solution (Benedict’s reagent) used for urinary glucose determination.
Pharmacology
In humans, niacinamide is required for lipid metabolism, tissue respiration, and glycogenolysis. In vivo, niacinamide is formed from conversion of niacin. In addition, some dietary tryptophan is oxidized to niacin and then to niacinamide in vivo. Niacinamide is incorporated into 2 coenzymes: nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP). NAD and NADP act as hydrogen-carrier molecules in glycogenolysis, tissue respiration, and lipid metabolism.
Niacin deficiency results in pellagra. The organ systems principally affected by niacin deficiency are the GI tract, skin, and CNS. Administration of niacin or niacinamide completely reverses the symptoms of niacin deficiency.
In large doses, niacin has some pharmacologic properties not produced by niacinamide. Niacin produces peripheral vasodilation, predominantly of cutaneous vessels in the face, neck, and chest. Cutaneous vasodilation induced by the drug appears to be mediated by prostaglandins (e.g., prostacyclin). Although animal studies indicate that very large doses of niacin may cause transient decreases in blood pressure and some vasodilation in most vascular beds, niacin dosages of 300–800 mg daily in humans probably cause only cutaneous vasodilation. Tolerance to the vasodilating effects of niacin occurs in most patients within 2 weeks. Niacin dosages of 1 g or more daily also decrease serum low-density lipoprotein and very low-density lipoprotein concentrations. Niacin reportedly causes release of histamine, resulting in an increase in gastric motility and acid secretion; the drug also activates the fibrinolytic system. Large doses of niacin have been reported to decrease uric acid excretion and to impair glucose tolerance.
Niacin (Vitamin) Pharmacokinetics
Absorption
Niacin and niacinamide are readily absorbed from the GI tract following oral administration, and niacinamide (no longer commercially available in the US) is readily absorbed from subcutaneous and IM injection sites. Following oral administration, niacin-induced vasodilation occurs within 20 minutes and persists for about 20–60 minutes. Following oral administration of 400 mg of niacin in an extended-release preparation, vasodilation occurs within 1 hour and persists for 8–10 hours. In one study, vasodilation of the face and neck occurred 2–3 minutes after beginning an IV infusion of niacin (no longer commercially available as an injection) at a rate of 0.01–0.1 mg/kg per minute; the flush persisted as long as the plasma niacin concentration was increasing and disappeared after niacin concentrations reached a plateau.
Niacin is well absorbed from food sources such as liver, beans, meats, and niacin-enriched or niacin-fortified food. Because niacin in mature cereal is highly bound, niacin is not well absorbed from this food. Biosynthesis of niacin from dietary tryptophan contributes to niacin intake.
Distribution
Niacinamide is widely distributed into body tissues. Niacin is distributed into milk.
Elimination
In amounts needed for physiologic function as a coenzyme (12–18 mg daily), niacin is converted to niacinamide; larger doses of niacin are converted to niacinamide to only a minor degree.
Niacinamide is metabolized in the liver to N-methylniacinamide, other N-methylated derivatives, and nicotinuric acid (the glycine conjugate of niacin). These metabolites are excreted in urine. Following administration of physiologic doses of niacin or niacinamide, only a small amount of niacinamide is excreted unchanged in urine; however, following administration of larger doses, a greater proportion of niacin and niacinamide is excreted unchanged.
Chemistry and Stability
Chemistry
Niacin and niacinamide are water-soluble, B complex vitamins. Niacin and tryptophan (an amino acid that is converted to niacin in vivo) are present in many foods including yeast, meat, fish, milk, eggs, green vegetables, and cereal grains; however, some of the vitamin in cereal grains may be present in an unabsorbable form. Commercially available niacin and niacinamide are prepared synthetically.
Niacin occurs as white crystals or crystalline powder, is odorless or has a slight odor, and is sparingly soluble in water and freely soluble in boiling water and in boiling alcohol. Niacin has a pKa of 4.85.
Niacinamide occurs as a white, odorless or practically odorless, crystalline powder with a bitter taste and is freely soluble in water and in alcohol. Niacinamide has pKa values of 0.5 and 3.35.
Stability
Niacin is incompatible with oxidizing agents, and niacinamide is incompatible with alkalis and strong acids.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Bulk |
Powder* |
|||
|
Oral |
Tablets, extended-release |
250 mg* |
Slo-Niacin |
Upsher-Smith |
|
500 mg* |
Slo-Niacin |
Upsher-Smith |
||
|
750 mg* |
Slo-Niacin |
Upsher-Smith |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Bulk |
Powder* |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions January 1, 2006. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Frequently asked questions
More about niacin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (117)
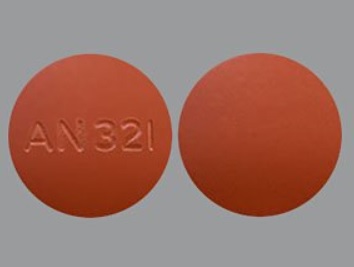
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: miscellaneous antihyperlipidemic agents
Patient resources
- Niacin drug information
- Niacin Capsules and Tablets
- Niacin Controlled-Release Capsules and Controlled-Release Tablets