Metoclopramide (Monograph)
Brand names: Gimoti, Reglan
Drug class: Prokinetic Agents
- Antiemetic Agents
- Benzamides
VA class: AU300
Molecular formula: C14H22ClN3O22O
CAS number: 54143-57-6
Warning
- Tardive Dyskinesia
-
May result in tardive dyskinesia. Risk increases with increasing duration of therapy and total cumulative dose. (See Tardive Dyskinesia under Cautions.)
-
Discontinue metoclopramide in patients who develop signs or symptoms of tardive dyskinesia. Symptoms may lessen or resolve in some patients after discontinuance.
-
Avoid treatment durations >12 weeks because of increased risk of developing tardive dyskinesia with longer-term use.
Introduction
Antiemetic; stimulant of upper GI motility (prokinetic agent); potent dopamine-receptor antagonist.
Uses for Metoclopramide
Diabetic Gastric Stasis
Symptomatic treatment of acute and recurrent diabetic gastric stasis (gastroparesis).
Symptomatic treatment may include dietary modifications, optimization of glycemic control, avoidance of drugs that adversely affect GI motility, antiemetics for relief of associated nausea and vomiting, and, in more severe cases, prokinetic agents to improve gastric emptying. The American Diabetes Association states that metoclopramide should be reserved for use in patients with severe diabetic gastric stasis that is unresponsive to other therapies, since evidence of benefit is weak and the drug is associated with serious adverse effects.
Postsurgical Gastric Stasis
Has been used for the symptomatic treatment of acute and chronic postsurgical gastric stasis† [off-label] following vagotomy and gastric resection or vagotomy and pyloroplasty.
Prevention of Postoperative Nausea and Vomiting
Prevention of postoperative nausea and vomiting when nasogastric suction is considered undesirable.
Prevention of Cancer Chemotherapy-induced Emesis
Used parenterally in high doses for the prevention of nausea and vomiting associated with emetogenic cancer chemotherapy including cisplatin alone or in combination with other antineoplastic agents.
Prevention of nausea and vomiting associated with other antineoplastic agents (e.g., cyclophosphamide, dacarbazine, doxorubicin, methotrexate) and with cancer chemotherapy regimens that do not include cisplatin.
ASCO does not consider metoclopramide an appropriate first-line antiemetic for any group of patients receiving chemotherapy of high emetic risk and states that this drug should be reserved for patients unable to tolerate or refractory to first-line agents (i.e., a type 3 serotonin [5-HT3] receptor antagonist [e.g., dolasetron, granisetron, ondansetron, palonosetron] with dexamethasone and aprepitant).
ASCO states that the combination of a 5-HT3 receptor antagonist, dexamethasone, and aprepitant is preferred in patients receiving combination chemotherapy with an anthracycline and cyclophosphamide; ASCO recommends combined therapy with a 5-HT3 receptor antagonist and dexamethasone for other chemotherapy regimens of moderate emetic risk (i.e., 31–90% incidence of emesis without antiemetics) and dexamethasone alone for chemotherapy regimens of low emetic risk (i.e., 11–30% incidence).
In patients experiencing nausea and vomiting despite recommended prophylaxis regimens, ASCO recommends that clinicians consider adding a benzodiazepine (e.g., alprazolam, lorazepam), butyrophenone, or phenothiazine to the regimen or substituting high-dose IV metoclopramide for the 5-HT3 receptor antagonist in the regimen.
Antiemetics can be prescribed on an as-needed basis for chemotherapy regimens with minimal emetic risk (<10% incidence of emesis without antiemetics).
Metoclopramide has been used orally† [off-label] for the prevention of chemotherapy-induced nausea and vomiting.
Oral† [off-label] metoclopramide has been effective when given in combination with dexamethasone for the prevention of delayed emesis in patients receiving chemotherapy. For prevention of delayed emesis in patients receiving cisplatin or other chemotherapy of high emetic risk, ASCO recommends the combination of dexamethasone and aprepitant.
Intubation of the Small Intestine
Used parenterally to facilitate small intestine intubation when the tube (e.g., endoscope, biopsy tube) does not pass through the pylorus during 10 minutes of conventional maneuvers.
Radiographic Examination of the Upper GI Tract
Used parenterally to stimulate gastric emptying and intestinal transit of barium when delayed emptying interferes with radiographic examination of the stomach and/or small intestine.
Gastroesophageal Reflux
Short-term (4–12 weeks) relief of symptomatic, documented gastroesophageal reflux in adults who are unresponsive to conventional therapy (e.g., changes in lifestyle, habits, or diet; weight reduction; acid-suppressive therapy).
Regular use for this purpose has declined; proton-pump inhibitors provide greater control of acid reflux and heartburn. Some experts recommend against use of metoclopramide for this purpose based on the drug’s adverse effect profile and lack of high-quality supporting data.
Migraine
Has been used for the management of migraine† [off-label]. Some experts state that metoclopramide may be considered as adjunctive therapy for control of nausea in patients with acute migraine attacks and that the IV drug may be considered for relief of migraine pain.
Metoclopramide Dosage and Administration
Administration
Administer orally, intranasally, by direct IV injection or IV infusion, or IM.
Metoclopramide therapy, including all dosage forms and routes of administration, should not exceed 12 weeks’ duration because of risk of tardive dyskinesia with longer-term use. (See Tardive Dyskinesia under Cautions.)
Oral Administration
Oral formulations of metoclopramide are recommended for use in adults only. (See Pediatric Use under Cautions.)
Administer orally on an empty stomach as conventional tablets, oral solution, or orally disintegrating tablets. At least one manufacturer states that dose should not be repeated if inadvertently administered with food. (See Food under Pharmacokinetics.)
Orally Disintegrating Tablets
Remove tablet from the blister packaging with dry hands and immediately place it on the tongue. Tablet should disintegrate in approximately one minute (range: 10 seconds to 14 minutes). Discard any tablet that breaks or crumbles during handling.
Intended to be taken without liquid; not known whether administration with liquid affects pharmacokinetics.
Intranasal Administration
Metoclopramide nasal spray is recommended for use in adults only. (See Pediatric Use under Cautions.)
Administer by nasal inhalation using a metered-dose spray pump. For information on administration technique, consult manufacturer's instructions for use.
Prime the pump prior to first use or if not used for ≥2 weeks.
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Dilution
For direct IV injection, use without further dilution.
If dose is >10 mg, dilute in 50 mL of a compatible IV solution.
For IV infusion, manufacturer recommends dilution in 50 mL of 5% dextrose, 0.9% sodium chloride, 5% dextrose and 0.45% sodium chloride, Ringer’s, or lactated Ringer’s injection.
Manufacturer states that 0.9% sodium chloride injection is preferred because metoclopramide hydrochloride is most stable in this solution.
Rate of Administration
Direct IV injection: Administer each 10 mg slowly over 1–2 minutes. Rapid IV injection may cause transient but intense feelings of anxiety and restlessness, followed by drowsiness.
IV infusion: Administer slowly over ≥15 minutes.
IM Administration
Inject without further dilution.
Dosage
Available as metoclopramide hydrochloride; dosage expressed in terms of metoclopramide.
Nasal spray delivers 15 mg of metoclopramide per 70-µL metered spray. Each bottle contains 9.8 mL of solution, which is sufficient for administration 4 times daily over a period of 4 weeks.
Dosage adjustment required in patients receiving concomitant therapy with potent CYP2D6 inhibitors. (See Drugs Affecting Hepatic Microsomal Enzymes under Interactions.)
Pediatric Patients
Intubation of the Small Intestine
IV
Children <6 years of age: Usually, one 0.1-mg/kg dose given by direct IV injection.
Children 6–14 years of age: Usually, one 2.5- to 5-mg dose given by direct IV injection.
Children >14 years of age: Usually, one 10-mg dose given by direct IV injection.
Adults
Diabetic Gastric Stasis
Use lowest effective dosage to reduce risk of adverse effects.
Oral
10 mg 4 times daily, given 30 minutes before meals and at bedtime. Continue for 2–8 weeks, depending on response.
Intranasal
15 mg (one spray in one nostril) administered 30 minutes before meals and at bedtime. Continue for 2–8 weeks, depending on response.
IV, then Oral
If symptoms are severe or oral use is not feasible, 10 mg 4 times daily, given by direct IV injection 30 minutes before meals and at bedtime. Continued use for up to 10 days may be required until symptoms subside enough to allow oral administration; however, thoroughly assess the risks and benefits prior to continuing therapy.
IM, then Oral
If symptoms are severe or oral use is not feasible, 10 mg 4 times daily, given by IM injection 30 minutes before meals and at bedtime. Continued use for up to 10 days may be required until symptoms subside enough to allow oral administration; however, thoroughly assess the risks and benefits prior to continuing therapy.
Prevention of Postoperative Nausea and Vomiting
IM
Manufacturer states that usual dose is 10 mg administered near the end of the surgical procedure; 20 mg also may be used.
Prevention of Cancer Chemotherapy-induced Emesis
Oral† [off-label]
When given in combination with dexamethasone in clinical trials for the prevention of delayed emesis (i.e., vomiting occurring ≥24 hours after chemotherapy), 20–40 mg (or 0.5 mg/kg) of metoclopramide has been given 2–4 times daily for 3 or 4 days.
IV
Manufacturer states that metoclopramide usually is given by IV infusion 30 minutes before administration of chemotherapy, and then repeated every 2 hours for 2 additional doses followed by every 3 hours for 3 additional doses. Manufacturer states that initial 2 doses should be 2 mg/kg if highly emetogenic chemotherapy used; for less emetogenic drugs or regimens, initial 1-mg/kg dose may be sufficient. However, combinations of other antiemetic agents generally are preferred as first-line regimens in patients receiving chemotherapy of moderate or high emetic risk (see Prevention of Cancer Chemotherapy-induced Emesis under Uses).
Intubation of the Small Intestine
IV
Usually, one 10-mg dose given by direct IV injection.
Radiographic Examination of the Upper GI Tract
IV
Usually, one 10-mg dose given by direct IV injection.
Gastroesophageal Reflux
Oral
If continuous dosing is required, 10–15 mg 4 times daily, given 30 minutes before meals and at bedtime for 4–12 weeks; base treatment duration on endoscopic evaluation of response.
For intermittent symptoms or symptoms at specific times of the day, one 20-mg dose before the provocative situation may be preferred to daily administration of multiple doses.
Prescribing Limits
Adults
Maximum 12 week's duration, including all dosage forms and routes of administration. (See Boxed Warning and see Tardive Dyskinesia under Cautions.)
Diabetic Gastric Stasis
Oral
Maximum 40 mg daily.
Intranasal
Maximum 4 times daily (i.e., maximum 60 mg daily).
Gastroesophageal Reflux
Oral
Maximum 60 mg daily.
Special Populations
Hepatic Impairment
Diabetic Gastric Stasis
Oral
Moderate or severe hepatic impairment (Child-Pugh class B or C): 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).
Mild hepatic impairment (Child-Pugh class A): Patient may receive usual recommended dosage.
Intranasal
Moderate or severe hepatic impairment: Not recommended because dosage cannot be adjusted.
Mild hepatic impairment: Patient may receive usual recommended dosage.
Gastroesophageal Reflux
Oral
Moderate or severe hepatic impairment: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).
Mild hepatic impairment: Patient may receive usual recommended dosage.
Renal Impairment
Modify dosage according to degree of renal impairment.
In patients with Clcr <40 mL/minute, manufacturers recommend an initial parenteral dosage of approximately 50% of the usual dosage. Subsequently, increase or decrease dosage according to response and tolerance.
Diabetic Gastric Stasis
Oral
Moderate or severe renal impairment (Clcr <60 mL/minute): 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).
End-stage renal disease, including hemodialysis or continuous ambulatory peritoneal dialysis (CAPD): 5 mg twice daily (maximum 10 mg daily).
Intranasal
Moderate or severe renal impairment (Clcr <60 mL/minute): Not recommended because dosage cannot be adjusted.
Mild renal impairment (Clcr ≥60 mL/minute): Patient may receive usual recommended dosage.
Gastroesophageal Reflux
Oral
Moderate or severe renal impairment (Clcr ≤60 mL/minute): 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).
End-stage renal disease, including hemodialysis or CAPD: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg twice daily (maximum 20 mg daily).
Geriatric Patients
Reduce initial dosage. (See Geriatric Use under Cautions.)
Administer lowest effective dosage.
Diabetic Gastric Stasis
Oral: Initially, 5 mg 4 times daily, given 30 minutes before meals and at bedtime. May titrate to 10 mg 4 times daily based on response and tolerability (maximum 40 mg daily).
Intranasal: Metoclopramide nasal spray not recommended as initial therapy in patients ≥65 years of age. May switch from an alternative metoclopramide preparation given at a stable dosage of 10 mg 4 times daily to the nasal formulation given at a dosage of 15 mg (one spray in one nostril) given 30 minutes before meals and at bedtime (maximum 4 times daily).
Gastroesophageal Reflux
Oral: Initially, 5 mg 4 times daily, given 30 minutes before meals and at bedtime. May titrate to 10–15 mg 4 times daily based on response and tolerability (maximum 60 mg daily).
Poor CYP2D6 Metabolizers
IV or IM: Manufacturers make no specific dosage recommendations.
Diabetic Gastric Stasis
Oral: 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).
Intranasal: Metoclopramide nasal spray not recommended because dosage cannot be adjusted.
Gastroesophageal Reflux
Oral: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).
Cautions for Metoclopramide
Contraindications
-
History of tardive dyskinesia or dystonic reaction to metoclopramide.
-
Mechanical obstruction or perforation or other situations in which stimulation of GI motility might be dangerous.
-
GI hemorrhage (however, has been used to empty the stomach of blood prior to endoscopy in patients with acute upper GI hemorrhage).
-
Pheochromocytoma or other catecholamine-releasing paragangliomas (due to potential for hypertensive/pheochromocytoma crisis).
-
History of seizure disorders.
-
Known hypersensitivity to metoclopramide.
Warnings/Precautions
Warnings
Tardive Dyskinesia
May cause tardive dyskinesia, a potentially irreversible disorder manifested by involuntary movements of the tongue, face, mouth, or jaw, and sometimes by involuntary movements of the trunk and/or extremities; movements may be choreoathetotic in appearance. (See Boxed Warning.)
Risk of developing tardive dyskinesia is increased in geriatric patients, especially older women, and patients with diabetes mellitus.
Risk of developing tardive dyskinesia and likelihood that it will become irreversible increase with duration of therapy and total cumulative dose; tardive dyskinesia occurs in about 20% of patients receiving the drug for >12 weeks.
Avoid treatment durations >12 weeks, including all dosage forms and routes of administration, and reduce dosage in geriatric patients.
Avoid use in patients receiving other drugs that are likely to cause tardive dyskinesia (e.g., antipsychotic agents).
Discontinue metoclopramide immediately in patients who develop signs or symptoms of tardive dyskinesia. Tardive dyskinesia may remit, either partially or completely, in some patients within several weeks to months after discontinuance.
Metoclopramide may suppress or partially suppress signs of tardive dyskinesia, thereby masking the underlying disease process; effect of this suppression on the long-term course of tardive dyskinesia is unknown. Do not use metoclopramide for symptomatic control of tardive dyskinesia.
Vesicular monoamine transporter 2 (VMAT2) inhibitors (e.g., deutetrabenazine, valbenazine) shown to be effective in reducing symptoms of tardive dyskinesia in controlled clinical studies.
Sensitivity Reactions
Tartrazine Sensitivity
Some formulations of metoclopramide oral solution may contain tartrazine (FD&C yellow No. 5), which may cause allergic reactions including bronchial asthma in susceptible individuals. Incidence of tartrazine sensitivity is low, but it frequently occurs in patients who are sensitive to aspirin.
Procainamide Cross-sensitivity
Theoretical potential for patients who are allergic to procainamide to exhibit cross-sensitivity to metoclopramide (since the drugs are structurally similar).
Other Warnings and Precautions
Extrapyramidal Symptoms
Potential for extrapyramidal reactions, especially in pediatric patients and adults <30 years of age or when high doses (e.g., IV doses for prophylaxis of cancer chemotherapy-induced nausea and vomiting) are administered.
Avoid use in patients receiving other drugs that are likely to cause extrapyramidal reactions (e.g., antipsychotic agents).
Commonly manifested as acute dystonic reactions or akathisia; stridor and dyspnea (possibly due to laryngospasm) reported rarely.
Generally occur within 24–48 hours after starting therapy and usually subside within 24 hours following drug discontinuance.
Most patients respond rapidly to treatment with diazepam or an agent with central anticholinergic activity (e.g., diphenhydramine hydrochloride 20–50 mg orally, IM, or IV; benztropine 1–2 mg IM ).
Akathisia appears to be related to peak drug concentration. If akathisia resolves, may consider reinitiating metoclopramide at a lower dosage.
Parkinsonian Symptoms
Parkinsonian symptoms (e.g., tremor, rigidity, bradykinesia, akinesia, mask-like facies) have occurred.
Possible exacerbation of parkinsonian symptoms; avoid use in patients with parkinsonian syndrome and in other patients receiving antiparkinsonian drugs.
More common during first 6 months of therapy but occur occasionally after longer periods.
Symptoms generally subside within 2–3 months following drug discontinuance.
Neuroleptic Malignant Syndrome (NMS)
NMS, a potentially fatal symptom complex characterized by hyperpyrexia, muscular rigidity, altered mental status, and autonomic dysfunction, reported with dopamine antagonists.
Has occurred following metoclopramide overdosage in patients receiving concomitant therapy with other drugs associated with NMS.
Avoid use in patients receiving other drugs associated with NMS (e.g., typical or atypical antipsychotic agents).
Important to determine whether untreated or inadequately treated extrapyramidal reactions and serious medical illness (e.g., pneumonia, systemic infection) may coexist. Also consider the possibility of central anticholinergic toxicity, heat stroke, malignant hyperthermia, drug fever, serotonin syndrome, and primary CNS pathology.
Immediately discontinue metoclopramide and other drugs not considered essential, provide intensive symptomatic treatment, monitor patient, and treat any concomitant serious medical condition for which specific therapies are available.
Depression
Mild to severe depression (including suicidal ideation and suicide) has occurred in patients with or without history of depression.
Avoid use in patients with a history of mental depression.
Hypertension
May increase BP; increase in circulating catecholamines reported in hypertensive patients. Avoid use in patients with hypertension and in those receiving MAO inhibitors.
Hypertensive crisis reported in patients with undiagnosed pheochromocytoma; discontinue metoclopramide in any patient who has a rapid increase in BP. (See Contraindications under Cautions.)
Fluid and Electrolyte Effects
Possible transient increases in plasma aldosterone concentrations and sodium retention; closely monitor patients (e.g., those with hepatic impairment, CHF, or cirrhosis) at risk of developing fluid retention and volume overload or hypokalemia.
Discontinue metoclopramide if fluid retention or volume overload occurs at any time during therapy.
Hyperprolactinemia
Stimulates prolactin secretion. Hyperprolactinemia may result in impaired gonadal steroidogenesis and inhibition of reproductive function in both females and males. Galactorrhea, gynecomastia, menstrual disorders (e.g., amenorrhea), and impotence reported.
Hyperprolactinemia may potentially stimulate prolactin-dependent breast cancer. However, some clinical and epidemiologic studies have not shown an association between dopamine D2-receptor antagonists and tumorigenesis in humans.
CNS Depression
Drowsiness may occur, particularly at higher dosages.
Performance of activities requiring mental alertness and physical coordination (operating machinery, driving a motor vehicle) may be impaired. Concomitant use of CNS depressants and drugs that cause extrapyramidal reactions may increase mental and/or physical impairment; avoid such concomitant use.
Pharmacogenomics
Metoclopramide elimination may be slower in poor CYP2D6 metabolizers than in intermediate, extensive, or ultra-rapid CYP2D6 metabolizers; poor metabolizers may be at increased risk of dystonic and other adverse reactions. Reduced dosage recommended. (See Poor CYP2D6 Metabolizers under Dosage and Administration.)
Patients with Cytochrome-b5 Reductase Deficiency
Patients with cytochrome-b5 reductase deficiency have an increased risk of methemoglobinemia and/or sulfhemoglobinemia when metoclopramide is administered.
Patients with Glucose-6-phosphate Dehydrogenase Deficiency
Methylene blue is not recommended for treatment of metoclopramide-induced methemoglobinemia in patients with glucose-6-phosphate dehydrogenase (G-6-PD) deficiency.
Phenylketonuria
Each 5- or 10-mg orally disintegrating tablet of metoclopramide contains aspartame, which is metabolized in the GI tract to provide 4.7 mg of phenylalanine per tablet.
GI Anastomosis or Closure
When deciding whether to use metoclopramide or NG suction to prevent postoperative nausea and vomiting, consider the possibility that metoclopramide theoretically could produce increased pressure on suture lines following GI anastomosis or closure.
Withdrawal Effects
Adverse reactions, particularly CNS reactions, may occur following discontinuance of drug. Some patients may experience withdrawal symptoms including dizziness, nervousness, and/or headaches following discontinuance.
Specific Populations
Pregnancy
Published studies, including retrospective cohort studies, national registry studies, and meta-analyses, have not revealed an increased risk of adverse pregnancy-related outcomes with metoclopramide use during pregnancy.
No adverse developmental effects observed in animal studies.
Crosses the placenta and may cause extrapyramidal reactions and methemoglobinemia in neonates whose mothers received the drug during delivery; monitor for extrapyramidal effects. (See Extrapyramidal Symptoms under Cautions.)
Lactation
Distributed into milk. Estimated dose received by breast-fed infants is <10% of the maternal weight-adjusted dose. In one study, estimated dose from breast milk was 6–24 mcg/kg daily at 3–9 days postpartum and 1–13 mcg/kg daily at 8–12 weeks postpartum. Exposure expected to be similar following maternal doses of 10 mg administered orally or 15 mg administered intranasally.
Adverse GI effects (e.g., intestinal discomfort, increased intestinal gas formation) reported in breast-fed infants exposed to metoclopramide.
Although metoclopramide increases prolactin concentrations, data are inadequate to support drug-related effects on milk production.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for metoclopramide and any potential adverse effects on the breast-fed child from the drug or underlying maternal condition.
Monitor nursing neonates for extrapyramidal effects (dystonias) and methemoglobinemia. (See Pediatric Use under Cautions.)
Pediatric Use
Safety profile in adults cannot be extrapolated to pediatric patients. Dystonias and other extrapyramidal reactions are more common in pediatric patients than in adults.
Safety and efficacy of oral and intranasal metoclopramide not established in pediatric patients; these formulations are not recommended for use in pediatric patients because of risk of tardive dyskinesia and other extrapyramidal reactions, as well as risk of methemoglobinemia in neonates.
Safety and efficacy of metoclopramide injection in pediatric patients is established only for use to facilitate intubation of the small intestine. Use metoclopramide injection with caution; incidence of extrapyramidal reactions is increased in children.
Use metoclopramide injection with caution in neonates. Neonatal susceptibility to methemoglobinemia is increased due to prolonged clearance (may cause excessive serum concentrations) in combination with decreased neonatal levels of cytochrome-b5 reductase.
Geriatric Use
Geriatric patients are more likely to have decreased renal function and may be more sensitive to therapeutic or adverse effects of metoclopramide.
Geriatric patients, especially older women, are at increased risk for tardive dyskinesia.
Risk of adverse parkinsonian effects increases with increasing dosage; administer lowest effective dosage in geriatric patients. If parkinsonian symptoms develop, generally should discontinue metoclopramide before initiating specific antiparkinsonian therapy.
Confusion and oversedation may occur.
Substantially eliminated by the kidneys; risk of adverse reactions, including tardive dyskinesia, may be greater in patients with impaired renal function. (See Renal Impairment under Cautions.)
Consider reduced dosage. Select dosage with caution, usually initiating therapy at the low end of the dosage range, because of age-related decreases in renal function and concomitant disease and drug therapy. (See Geriatric Patients under Dosage and Administration).
Hepatic Impairment
Clearance may be reduced, resulting in increased exposure. (See Elimination: Special Populations, under Pharmacokinetics.) Possible increased risk of adverse effects. Reduced dosage recommended, depending on degree of hepatic impairment. (See Hepatic Impairment under Dosage and Administration.)
Possible increased risk of fluid retention and hypokalemia in patients with cirrhosis. (See Fluid and Electrolyte Effects under Cautions.) Discontinue if fluid retention or volume overload occurs at any time during therapy.
Renal Impairment
Clearance may be reduced, resulting in increased exposure. (See Absorption: Special Populations, under Pharmacokinetics.) Possible increased risk of adverse effects, including tardive dyskinesia. Use with caution; reduced dosage recommended, depending on degree of renal impairment. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Restlessness, drowsiness, fatigue, lassitude, nausea, bowel disturbances (principally diarrhea).
Adverse effects with orally disintegrating tablets and nasal spray are similar to those observed with conventional tablets, but dysgeusia is the most common adverse effect with the nasal spray.
Drug Interactions
Metabolized by CYP2D6; also conjugated with glucuronic acid and sulfuric acid.
Orally Administered Drugs
Possible decreased absorption of certain drugs that disintegrate, dissolve, and/or are absorbed mainly in the stomach.
Possible enhanced rate and extent of absorption of drugs mainly absorbed in the small intestine.
Drugs that Impair GI Motility
Possible reduced oral absorption of metoclopramide; monitor for reduced metoclopramide efficacy.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP2D6 inhibitors: Possible increased systemic exposure to metoclopramide and exacerbation of extrapyramidal symptoms. Reduce metoclopramide dosage (see Table 1). Examples of potent CYP2D6 inhibitors include, but are not limited to, bupropion, fluoxetine, paroxetine, and quinidine.
|
Metoclopramide Route of Administration |
Adult Dosage Recommendation |
|---|---|
|
Oral |
Diabetic gastric stasis: 5 mg given 4 times daily (maximum 20 mg daily) Gastroesophageal reflux: 5 mg given 4 times daily or 10 mg given 3 times daily (maximum 30 mg daily) |
|
Parenteral |
Manufacturers make no specific recommendations |
|
Intranasal |
Not recommended; dosage cannot be adjusted to reduce exposure |
Drugs Metabolized by Hepatic Microsomal Enzymes
CYP2D6 substrates: In vitro studies suggest metoclopramide can inhibit CYP2D6, but interactions considered unlikely in vivo at clinically relevant concentrations.
Drugs with Similar Adverse Effect Profiles
Drugs that are likely to cause extrapyramidal reactions: Possible additive effects; avoid concomitant use.
Drugs known to cause tardive dyskinesia or NMS: Possible additive effects; avoid concomitant use.
Dopaminergic Agents
Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine. Avoid concomitant use; if concomitant use is required, monitor therapeutic effects.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
Possible enhanced rate and extent of acetaminophen absorption |
|
|
Anesthetic agents |
Acute hypotension reported with concomitant IV metoclopramide and hypotensive anesthetic agents (with or without ganglionic blocking agents) during neurosurgical procedures |
Clinical importance not known |
|
Anticholinergic agents (e.g., atropine) |
Antagonism of GI motility effects of metoclopramide Impairment of GI motility by anticholinergic agent may reduce oral absorption of metoclopramide |
Monitor for reduced metoclopramide efficacy |
|
Antidiarrheal agents, antiperistaltic |
Impairment of GI motility by antiperistaltic agent may reduce oral absorption of metoclopramide |
Monitor for reduced metoclopramide efficacy |
|
Antipsychotic agents (e.g., butyrophenones, phenothiazines) |
Possible additive adverse effects, including increased frequency and severity of tardive dyskinesia, parkinsonian or other extrapyramidal symptoms, and NMS |
Avoid concomitant use |
|
Aspirin |
Possible enhanced rate and extent of aspirin absorption |
|
|
Atovaquone |
Possible decreased atovaquone absorption |
Monitor for reduced atovaquone efficacy |
|
CNS depressants (alcohol, opiates or other analgesics, sedatives or hypnotics, anxiolytic agents, anesthetics) |
Increased CNS depressant effects; possible enhanced rate and extent of alcohol absorption |
Avoid concomitant use |
|
Cyclosporine |
Possible enhanced rate and extent of cyclosporine absorption |
Monitor cyclosporine concentrations and adjust cyclosporine dosage as needed |
|
Diazepam |
Possible enhanced rate and extent of diazepam absorption |
|
|
Digoxin |
Possible decreased digoxin absorption |
Monitor digoxin concentrations and adjust digoxin dosage as needed |
|
Dopamine agonists (e.g., apomorphine, bromocriptine, cabergoline, pramipexole, ropinirole, rotigotine) |
Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine |
Avoid concomitant use; if concomitant use required, monitor therapeutic effects |
|
Fluoxetine |
Increased peak concentration and AUC of metoclopramide by 40 and 90%, respectively; possible exacerbation of extrapyramidal symptoms |
Reduce metoclopramide dosage (see Table 1) |
|
Fosfomycin |
Possible decreased fosfomycin absorption |
Monitor for reduced fosfomycin efficacy |
|
Insulin |
Possible alteration of glycemic control secondary to metoclopramide-related changes in the delivery of food to and the rate of absorption in the intestine |
Monitor blood glucose; adjustment of insulin dose or timing may be necessary |
|
Levodopa |
Possible enhanced rate and extent of levodopa absorption Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine |
Avoid concomitant use; if concomitant use required, monitor therapeutic effects |
|
Lithium |
Possible enhanced rate and extent of lithium absorption |
|
|
MAO inhibitors |
Possible hypertensive reaction due to metoclopramide-induced release of catecholamines |
Avoid concomitant use |
|
Neuromuscular blocking agents |
Enhanced neuromuscular blockade due to metoclopramide inhibition of plasma cholinesterase |
Monitor for prolonged neuromuscular blockade |
|
Opiate analgesics |
Antagonism of GI motility effects of metoclopramide Impairment of GI motility by opiate may reduce oral absorption of metoclopramide |
Monitor for reduced metoclopramide efficacy |
|
Posaconazole |
Posaconazole oral suspension: Possible decreased posaconazole absorption Posaconazole delayed-release tablets: Absorption not affected |
Posaconazole oral suspension: Monitor for reduced posaconazole efficacy |
|
Sirolimus |
Possible enhanced sirolimus absorption |
Monitor sirolimus concentrations and adjust sirolimus dosage as needed |
|
Tacrolimus |
Possible enhanced tacrolimus absorption |
Monitor tacrolimus concentrations and adjust tacrolimus dosage as needed |
|
Tetracycline |
Possible enhanced rate and extent of tetracycline absorption |
Metoclopramide Pharmacokinetics
Absorption
Bioavailability
Following oral administration, rapidly and almost completely absorbed; limited data indicate that 30–100% of an oral dose reaches systemic circulation as unchanged metoclopramide. Peak plasma concentration usually attained at 1–2 hours.
Orally disintegrating tablets are bioequivalent to the conventional tablets under fasting conditions.
Following IM administration, absolute bioavailability is 74–96%.
Following intranasal administration, absolute bioavailability is 47%. Absorption is reduced following intranasal versus oral administration; peak concentration, AUC, and time to reach peak concentration are similar following a 15-mg intranasal dose or a 10-mg oral dose.
Over an intranasal dose range of 10–80 mg, systemic exposure is proportional to dose.
Onset
Following oral administration, 30–60 minutes for effects on GI tract.
Following IM administration, 10–15 minutes for effects on GI tract.
Following IV administration, 1–3 minutes for effects on GI tract.
Duration
1–2 hours.
Food
Administration of the orally disintegrating tablets immediately after a high-fat meal did not affect extent of absorption, but decreased peak blood concentration by 17% and increased time to peak concentration to 3 hours (compared with 1.75 hours under fasting conditions). Clinical importance of decreased peak concentration is unknown.
Special Populations
Patients with gastric stasis: Absorption may be delayed or diminished.
Moderate or severe renal impairment: AUC following oral administration is approximately twice that observed in individuals with normal renal function; in end-stage renal disease requiring dialysis, AUC is approximately 3.5 times that observed in individuals with normal renal function.
Females: AUC and peak concentration following intranasal administration are increased by 34 and 42%, respectively, compared with males. Clinical relevance unknown.
Body weight: Following intranasal administration, lower systemic exposure expected in individuals with higher lean body weight (within range of 34–94 kg). Clinical relevance unknown.
Infants and children: Pharmacodynamics are highly variable; relationship between drug plasma concentrations and pharmacodynamic effects not established.
Infants: Metoclopramide may accumulate in plasma after multiple doses; mean peak plasma concentration was 2-fold higher after 10th dose compared with that after first dose in infants (3.5 weeks–5.4 months of age) with gastroesophageal reflux receiving metoclopramide oral solution.
Distribution
Extent
In mice, distributed into most body tissues and fluids; high concentrations in GI mucosa, liver, biliary tract, and salivary glands, with lower concentrations in brain, heart, thymus, adrenals, adipose tissue, and bone marrow.
Crosses the placenta.
Distributed into milk in humans; milk concentrations are higher than plasma concentrations 2 hours after oral administration.
Plasma Protein Binding
13–30% (principally albumin).
Elimination
Metabolism
Undergoes enzymatic metabolism via oxidation as well as conjugation with glucuronic acid and sulfuric acid in the liver. Monodeethylmetoclopramide, a major oxidative metabolite, is formed mainly by CYP2D6, which is subject to genetic variability. (See Pharmacogenomics under Cautions.)
Elimination Route
Excreted in urine (85%) as unchanged drug and metabolites and also in feces (about 5%) within 72 hours following an oral dose. About 18–20% of an oral dose excreted in urine as unchanged drug within 36 hours.
Minimally removed by hemodialysis or peritoneal dialysis.
Half-life
Biphasic; terminal-phase half-life is 2.5–6 hours in adults. Half-life of 8.1 hours reported following intranasal administration.
Elimination half-life is about 4.1–4.5 hours in children.
Special Populations
Renal impairment: Half-life may be prolonged and plasma concentrations increased. (See Absorption: Special Populations, under Pharmacokinetics.)
Severe hepatic impairment (Child-Pugh class C): Average clearance following oral administration is reduced by approximately 50% compared with individuals with normal hepatic function.
Data insufficient to determine whether pharmacokinetics of the drug in children are similar to those in adults.
Neonates: Reduced clearance, possibly associated with immature renal and hepatic functions present at birth.
Stability
Storage
Nasal
Solution
20–25°C (may be exposed to 15–30°C). Discard 4 weeks after opening.
Oral
Tablets
Tight, light-resistant containers at 20–25°C.
Tablets, Orally Disintegrating
20–25°C. Protect from moisture. Do not remove from blister pack until immediately before administration.
Solution
Tight, light-resistant containers at 20–25°C. Protect from freezing.
Parenteral
Injection
20–25°C. Protect from light.
Following dilution with 5% dextrose, 0.9% sodium chloride, 5% dextrose and 0.45% sodium chloride, Ringer’s, or lactated Ringer’s injection, store for up to 48 hours (without freezing) when protected from light or for up to 24 hours under normal light conditions (i.e., unprotected from light).
May be stored frozen for up to 4 weeks following dilution with 0.9% sodium chloride injection.
Degradation occurs if metoclopramide is diluted in 5% dextrose injection and frozen.
Compatibility
Parenteral
Solution Compatibility124 267
|
Compatible |
|---|
|
Amino acids 2.75%, dextrose 25%, electrolytes |
|
Dextrose 5% in sodium chloride 0.45% |
|
Ringer’s injection |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.9% |
|
Variable |
|
Dextrose 5% in water |
Manufacturer states that sodium chloride 0.9% is preferred diluent because metoclopramide hydrochloride is most stable in this solution.
Drug Compatibility
|
Compatible |
|---|
|
Clindamycin phosphate |
|
Mannitol 20% |
|
Meperidine HCl |
|
Meropenem |
|
Morphine sulfate |
|
Multivitamins |
|
Oxycodone HCl |
|
Potassium acetate |
|
Potassium chloride |
|
Potassium phosphates |
|
Ranitidine HCl |
|
Tramadol HCl |
|
Verapamil HCl |
|
Incompatible |
|
Dexamethasone sodium phosphate with lorazepam and diphenhydramine HCl |
|
Erythromycin lactobionate |
|
Fluorouracil |
|
Furosemide |
|
Compatible |
|---|
|
Acetaminophen |
|
Aldesleukin |
|
Amifostine |
|
Aztreonam |
|
Bivalirudin |
|
Bleomycin sulfate |
|
Cangrelor tetrasodium |
|
Ceftaroline fosamil |
|
Ceftolozane sulfate-tazobactam sodium |
|
Ciprofloxacin |
|
Cisatracurium besylate |
|
Cisplatin |
|
Cladribine |
|
Clarithromycin |
|
Cyclophosphamide |
|
Dexmedetomidine HCl |
|
Diltiazem HCl |
|
Docetaxel |
|
Doripenem |
|
Doxapram HCl |
|
Doxorubicin HCl |
|
Droperidol |
|
Etoposide phosphate |
|
Famotidine |
|
Fenoldopam mesylate |
|
Fentanyl citrate |
|
Filgrastim |
|
Fluconazole |
|
Fludarabine phosphate |
|
Fluorouracil |
|
Foscarnet sodium |
|
Gallium nitrate |
|
Gemcitabine HCl |
|
Granisetron HCl |
|
Heparin sodium |
|
Hetastarch in lactated electrolyte injection |
|
Hydromorphone HCl |
|
Idarubicin HCl |
|
Isavuconazonium sulfate |
|
Leucovorin calcium |
|
Levofloxacin |
|
Linezolid |
|
Melphalan HCl |
|
Meperidine HCl |
|
Meropenem |
|
Meropenem-vaborbactam |
|
Methadone HCl |
|
Methotrexate sodium |
|
Mitomycin |
|
Morphine sulfate |
|
Ondansetron HCl |
|
Oxaliplatin |
|
Paclitaxel |
|
Palonosetron HCl |
|
Pemetrexed disodium |
|
Piperacillin sodium–tazobactam sodium |
|
Plazomicin sulfate |
|
Quinupristin-dalfopristin |
|
Remifentanil HCl |
|
Sargramostim |
|
Tacrolimus |
|
Tedizolid phosphate |
|
Telavancin HCl |
|
Teniposide |
|
Thiotepa |
|
Tigecycline |
|
Topotecan HCl |
|
Vinblastine sulfate |
|
Vincristine sulfate |
|
Vinorelbine tartrate |
|
Zidovudine |
|
Incompatible |
|
Allopurinol sodium |
|
Amsacrine |
|
Doxorubicin HCl liposome injection |
|
Furosemide |
|
Variable |
|
Acyclovir sodium |
Actions
-
Complex pharmacology; mechanism(s) of action not fully elucidated; principal effects involve the GI tract and CNS.
-
At low concentrations in vitro, metoclopramide increases the resting tone and phasic contractile activity of GI smooth muscle.
-
Increases lower esophageal sphincter pressure.
-
Accelerates gastric emptying and intestinal transit from the duodenum to the ileocecal valve by increasing the amplitude and duration of esophageal contractions, resting tone of the lower esophageal sphincter, and amplitude and tone of gastric (especially antral) contraction and by relaxing the pyloric sphincter and the duodenal bulb, while increasing peristalsis of the duodenum and jejunum.
-
Unlike nonspecific cholinergic-like stimulation of upper GI smooth muscle, the stimulant effects of metoclopramide on GI smooth muscle coordinate gastric, pyloric, and duodenal motor activity.
-
Precise mechanism of antiemetic action is unclear. Directly affects medullary chemoreceptor trigger zone (CTZ), apparently by blocking dopamine receptors; increases CTZ threshold and decreases sensitivity of visceral nerves that transmit impulses from GI tract to vomiting center; and enhances gastric emptying (believed to minimize stasis that precedes vomiting). Also may inhibit serotonin (5-HT3) receptors (at relatively high doses).
-
Produces varying degrees of sedation and lethargy.
-
May cause extrapyramidal reactions and worsen symptoms in patients with parkinsonian syndrome.
Advice to Patients
-
Importance of providing patient or caregiver with a copy of the manufacturer’s medication guide. Importance of instructing patient or caregiver to read and understand the contents of the medication guide before initiating therapy and each time the prescription is refilled.
-
Importance of informing patients that oral and intranasal formulations of metoclopramide are recommended for use in adults only.
-
Importance of instructing patients receiving intranasal metoclopramide therapy on appropriate use of the metered-dose inhaler and providing them with a copy of the manufacturer's instructions for use.
-
Risk of tardive dyskinesia. Importance of contacting clinician immediately if new, abnormal, involuntary, or uncontrollable muscle movements occur (e.g., lip smacking, chewing, puckering mouth, frowning, scowling, tongue protrusion, blinking, eye movements, arm and leg shaking). Importance of not taking metoclopramide for >12 weeks.
-
Risk of NMS. Importance of contacting clinician immediately if signs or symptoms of NMS (e.g., high fever, stiff muscles, difficulty thinking, fast or uneven heartbeat, increased sweating) occur.
-
Risk of dystonic reactions, parkinsonian symptoms, or akathisia. Importance of contacting clinician immediately if such reactions occur.
-
Risk of depression and/or suicidality. Importance of contacting clinician immediately if depression or suicidality occurs.
-
Potential for drowsiness or dizziness to occur.
-
Potential for metoclopramide to impair mental alertness or physical coordination; avoid driving or operating machinery until effects on individual are known. Advise patient that alcohol, opiate analgesics, sedatives or hypnotics, anxiolytic agents, other CNS depressants, and other drugs that cause extrapyramidal symptoms may enhance such impairment.
-
For patients receiving metoclopramide nasal solution, importance of not repeating a dose if uncertain whether the spray entered the nostril and of not administering an extra dose or a double dose to make up for a missed dose; instead, administer the next dose at the regularly scheduled time.
-
Importance of informing patients with phenylketonuria that metoclopramide orally disintegrating tablets contain aspartame.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses. Advise patient that concomitant use of metoclopramide with many other drugs may precipitate or worsen tardive dyskinesia, extrapyramidal symptoms, NMS, and CNS depression.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Nasal |
Solution |
15 mg (of metoclopramide) per metered spray |
Gimoti |
Evoke |
|
Oral |
Solution |
5 mg (of metoclopramide) per 5 mL* |
Metoclopramide Hydrochloride Oral Solution |
|
|
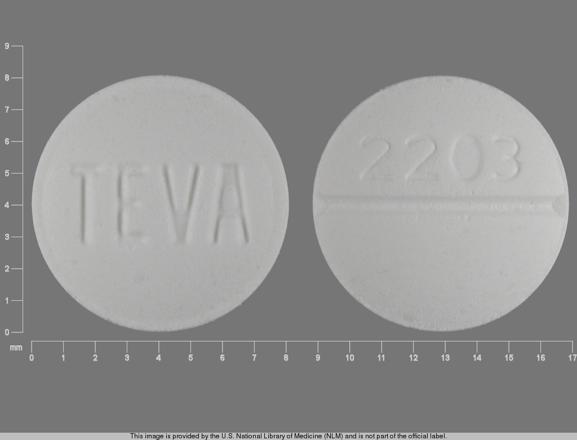
Tablets |
5 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Tablets |
||
|
Reglan |
ANI |
|||
|
10 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Tablets |
|||
|
Reglan (scored) |
ANI |
|||
|
Tablets, orally disintegrating |
5 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Orally Disintegrating Tablets |
||
|
10 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Orally Disintegrating Tablets |
|||
|
Parenteral |
Injection |
5 mg (of metoclopramide) per mL* |
Metoclopramide Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions March 15, 2021. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about metoclopramide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (514)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: GI stimulants
- Breastfeeding
Patient resources
Professional resources
- Metoclopramide Injection prescribing information
- Metoclopramide Oral Solution (FDA)
- Metoclopramide Orally DisintegratingTablets (FDA)
- Metoclopramide Tablets (FDA)