Vandetanib Dosage
Medically reviewed by Drugs.com. Last updated on Apr 23, 2025.
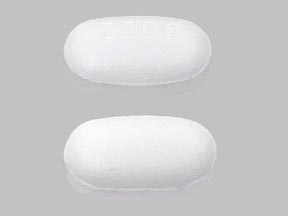
Applies to the following strengths: 100 mg; 300 mg
Usual Adult Dose for:
Additional dosage information:
Usual Adult Dose for Thyroid Cancer
Initial dose: 300 mg orally once daily.
Duration of therapy: Continue drug until disease progression or unacceptable toxicity occurs.
Use: For the treatment of symptomatic or progressive medullary thyroid cancer in patients with unresectable locally advanced or metastatic disease.
Renal Dose Adjustments
Mild renal impairment (CrCl 50 mL/min or greater): No dose adjustment recommended.
Moderate to severe renal impairment (CrCl less than 50 mL/min): Initial dose: 200 mg orally once daily.
Liver Dose Adjustments
Mild hepatic impairment: No dose adjustment recommended.
Moderate and severe hepatic impairment: Use not recommended.
Dose Adjustments
QT Interval Prolongation:
- For corrected QT interval Fridericia (QTcF) greater than 500 milliseconds (msec): Interrupt therapy; may resume at a reduced dose when QTcF returns to less than 450 msec.
For Adverse Reactions:
- For common terminology criteria for adverse event (CTCAE) Grade 3 or greater: Interrupt therapy; may resume at reduced dose of 200 mg orally once daily when toxicity resolves or improves to CTCAE grade 1.
For Recurrent Toxicities:
- For recurrent toxicities: Interrupt therapy; may resume at reduced dose of 100 mg orally once daily when toxicity resolves or improves to CTCAE grade 1; assess if continued treatment is warranted.
Due to long half-life (19 hours), adverse reactions, including QT prolongation, may take weeks to resolve; continued monitoring will be necessary.
Precautions
US REMS: The US FDA requires a Risk Evaluation and Mitigation Strategy (REMS) for this drug. It includes a medication guide, communication plan, elements to assure safe use, and implementation system. For additional information: www.fda.gov/REMS.
US BOXED WARNINGS:
- Vandetanib can prolong the QT interval.
- Torsades de pointes and sudden death have occurred in patients receiving vandetanib.
- Do not use in patients with long QT syndrome.
- Do not use in patients with hypocalcemia, hypokalemia, hypomagnesemia; correct electrolyte levels prior to administration and monitor electrolytes periodically.
- Avoid use with drugs known to prolong the QT interval.
- Only prescribers and pharmacies certified with the restricted distribution program may prescribe and dispense vandetanib.
Safety and efficacy have not been established in patients younger than 18 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- May be taken with or without food.
- Do not crush or chew tablets; swallow whole with water.
- For patients who have difficulty swallowing tablets, a dispersion of the tablet in water may be used: Drop tablet in 2 ounces of non-carbonated water, stir for about 10 minutes (tablet will not completely dissolve); swallow the dispersion immediately; to ensure complete dosing, mix any remaining residue with 4 ounces of non-carbonated water and swallow. The dispersion may also be administered through nasogastric or gastrostomy tubes.
- If contact occurs with crushed tablet, wash affected area well with water.
- Missed dose: If a dose is missed, the missed dose should be skipped if it is less than 12 hours before the next scheduled dose. Patients should not take a double dose to make up for a missed dose.
General:
- For patients with indolent, asymptomatic, or slowly progressing disease, carefully consider treatment-related risks.
- Treatment should be initiated and supervised by a clinician experienced with the management of medullary thyroid cancer, use of anticancer medicinal products, and experienced in the assessment of ECGs.
Monitoring:
- Obtain an ECG, serum potassium, calcium, magnesium, and TSH, at baseline, at 2 to 4 weeks, at 8 to 12 weeks, and every 3 months thereafter; maintain potassium at 4 mEq/L or higher (within normal range).
- Monitor electrolytes and ECG more frequently as clinically indicated.
- Perform ophthalmologic examination, including slit lamp examination, in patients who experience visual changes.
Patient Advice:
- Advise patient to contact healthcare provider if they experience cardiac symptoms, skin reactions, respiratory symptoms, diarrhea, or CNS symptoms such as seizures, visual disturbances, or difficulty thinking.
- Advise patient to use effective contraception during therapy and for 4 months following the last dose; if pregnancy is suspected, patients should seek medical advice and counseling.
- Advise patient to use appropriate sun protection during therapy and for 4 months following the last dose.
More about vandetanib
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- During pregnancy
- Drug class: EGFR inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.