Vandetanib Side Effects
Medically reviewed by Drugs.com. Last updated on Jul 16, 2023.
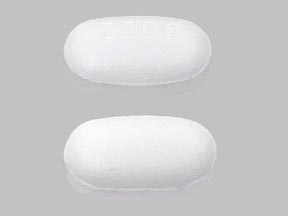
Applies to vandetanib: oral tablet.
Warning
Oral route (Tablet)
Vandetanib can prolong the QT interval, and torsades de pointes and sudden death have been reported with its use. Do not use in patients with hypocalcemia, hypokalemia, hypomagnesemia, or long QT syndrome; electrolyte depletion must be corrected prior to starting vandetanib and should be periodically monitored. Avoid drugs that are known to prolong the QT interval. Vandetanib is only available through a restricted distribution program (Vandetanib REMS).
Serious side effects of Vandetanib
Along with its needed effects, vandetanib may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking vandetanib:
More common
- Bleeding gums
- blindness
- blistering, crusting, irritation, itching, or reddening of the skin
- blurred vision
- body aches or pain
- chest pain or tightness
- chills
- cloudy urine
- confusion
- cough
- coughing up blood
- difficulty with breathing or swallowing
- dizziness
- ear congestion
- fainting
- fever
- headache
- increased menstrual flow or vaginal bleeding
- increased sensitivity of the skin to sunlight
- irregular heartbeat, recurrent
- loss of voice
- muscle cramps in the hands, arms, feet, legs, or face
- nervousness
- nosebleeds
- numbness and tingling around the mouth, fingertips, or feet
- paralysis
- pounding in the ears
- prolonged bleeding from cuts
- red or black, tarry stools
- red or dark brown urine
- seizures
- severe sunburn
- slow or fast heartbeat
- sneezing
- sore throat
- stomach cramps or pain
- stuffy or runny nose
- tenderness
- tremor
- trouble breathing
- unusual tiredness or weakness, severe
- watery or bloody diarrhea
Less common
- Blue lips, fingernails, or skin
- dilated neck veins
- extreme tiredness or weakness
- infection from breathing foreign substance into the lungs
- irregular heartbeat
- irregular, fast or slow, or shallow breathing
- lightheadedness
- swelling of the face, fingers, feet, or lower legs
- weight gain
Rare
- Bloating
- constipation
- decreased urine output
- indigestion
- loss of appetite
- nausea
- pains in the stomach, side, or abdomen, possibly radiating to the back
- yellow eyes or skin
Other side effects of Vandetanib
Some side effects of vandetanib may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Belching
- blemishes on the skin
- change in or loss of taste
- cracked, dry, or scaly skin
- cracks in the skin
- decreased weight
- depression
- discoloration of the fingernails or toenails
- dry mouth or skin
- hair loss or thinning of the hair
- heartburn
- lack or loss of strength
- loosening of the fingernails
- loss of heat from the body
- muscle aches or spasms
- pimples
- rash with flat lesions or small raised lesions on the skin
- redness or other discoloration of the skin
- redness or soreness around the fingernails
- stomach discomfort or upset
- trouble sleeping
For Healthcare Professionals
Applies to vandetanib: oral tablet.
General
The most commonly reported adverse effects in decreasing order of frequency included diarrhea/colitis, rash, acneiform dermatitis, hypertension, nausea, headache, upper respiratory tract infections, decreased appetite, and abdominal pain.
During clinical trials, treatment discontinuation due to adverse reactions occurred in 21% of patients. Events leading to discontinuation included asthenia, rash, diarrhea, fatigue, pyrexia, elevated creatinine, QT prolongation, and hypertension. Dose interruption occurred in 47% of patients and dose reduction in 36%.[Ref]
Cardiovascular
Very common (10% or more): Hypertension/hypertensive crisis/accelerated hypertension (33%); ECG QT prolonged (14%)
Uncommon (0.1% to 1%): Heart failure, arrhythmia, atrial fibrillation, bradycardia, pericarditis, chest pain, cardiac arrest
Frequency not reported: Torsades de pointes; ventricular tachycardia[Ref]
Common terminology criteria for adverse events (CTCAE) grade 3 to 4 hypertension/hypertensive crisis/accelerated hypertension was reported in 9% of patients.
CTCAE grade 3 to 4 QT prolongation was reported in 8% of patients. Among patients who experienced QT prolongation, 69% experienced a QT interval Fridericia (QTcF) greater than 450 milliseconds (msec) with 7% having reported a QTcF greater than 500 msec. In a pharmacodynamics study in patients with medullary thyroid cancer receiving vandetanib 300 mg orally once daily, mean change in QTcF was 35 msec and mean change in QTcF remained above 30 msec for the duration of the trial (up to 2 years). A change in QTcF greater than 60 msec was reported in 36% of patients experience and 4.3% of patients had a QTcF greater than 500 msec.[Ref]
Dermatologic
Types of rash reported included rash, rash (erythematous, generalized, macular, maculopapular, popular, pruritic, and exfoliative), dermatitis, bullous dermatitis, generalized erythema, and eczema. CTCAE grade 3 to 4 rash, dermatitis/acneiform/acne, photosensitivity reaction, and pruritus were reported in 5%, 1%, 2%, and 1% of patients, respectively.
Nail abnormalities reported included nail disorder, nail bed inflammation, nail bed tenderness, paronychia, nail bed infection, and nail infection.[Ref]
Very common (10% or more): Rash (53%); dermatitis acneiform/acne (35%); dry skin (15%); photosensitivity reaction (13%); pruritus (11%)
Common (1% to 10%): Nail abnormalities; alopecia
Uncommon (0.1% to 1%): Skin ulcer
Frequency not reported: Stevens-Johnson syndrome, erythema multiforme[Ref]
Gastrointestinal
Very common (10% or more): Diarrhea/colitis (57%); nausea (33%); abdominal pain (21%); vomiting (15%); dyspepsia (11%);
Common (1% to 10%): Dry mouth
Uncommon (0.1% to 1%): Pancreatitis, intestinal perforation, dysphagia, gastrointestinal hemorrhage, colitis, gastritis, ileus, peritonitis[Ref]
CTCAE grade 3 to 4 diarrhea/colitis, nausea, abdominal pain, and vomiting were reported in 11%, 1%, 3%, and 1%, respectively.[Ref]
Genitourinary
Very common (10% or more): Proteinuria (10%)
Common (1% to 10%): Urinary tract infection
Uncommon (0.1% to 1%): Calculus ureteric[Ref]
Hematologic
Less than 1% of patients experienced CTCAE grade 3 to 4 neutropenia. Bleeding events were grade 1 to 2 events.[Ref]
Very common (10% or more): Bleeding (14%); neutropenia (10%)
Common (1% to 10%): Thrombocytopenia (9%)[Ref]
Hepatic
An ALT increase classified as CTCAE grade 3 to 4 was experienced in 2% of patients.[Ref]
Very common (10% or more): ALT increased (51%)
Uncommon (0.1% to 1%): Cholecystitis, cholelithiasis[Ref]
Metabolic
CTCAE grade 3 to 4 hypocalcemia, decreased appetite, and hypomagnesemia occurred in 6%, 4%, and less than 1 % of patients, respectively.[Ref]
Very common (10% or more): Hypocalcemia (57%); hypoglycemia (24%); decreased appetite (21%)
Common (1% to 10%): Hypomagnesemia, hypokalemia, hypercalcemia, hyperglycemia, dehydration, hyponatremia, weight loss
Uncommon (0.1% to 1%): Hypokalemia[Ref]
Musculoskeletal
Common (1% to 10%): Muscle spasms[Ref]
Nervous system
Very common (10% or more): Headache (26%); paresthesia, dizziness
Common (1% to 10%): Dysgeusia, tremor, lethargy, loss of consciousness, balance disorder
Uncommon (0.1% to 1%): Convulsion, clonus, brain edema
Frequency not reported: Reversible posterior leukoencephalopathy syndrome[Ref]
Ocular
Ocular abnormalities included corneal edema, corneal opacity, corneal dystrophy, corneal pigmentation, keratopathy, arcus lipoides, corneal deposits, acquired corneal dystrophy. Slit lamp examination of vandetanib-treated patients revealed vortex keratopathy.[Ref]
Very common (10% or more): Corneal abnormalities (13%)
Common (1% to 10%): Blurred vision
Uncommon (0.1% to 1%): Glaucoma[Ref]
Other
Very common (10% or more): Fatigue (24%); asthenia (15%)
Common (1% to 10%): Pyrexia[Ref]
CTCAE grade 3 to 4 fatigue was reported in 6% of patients.[Ref]
Psychiatric
CTCAE grade 3 to 4 depression was reported in 2% of patients.[Ref]
Very common (10% or more): Insomnia (13%); depression (10%)
Common (1% to 10%): Anxiety
Uncommon (0.1% to 1%): Bipolar disorder[Ref]
Renal
Very common (10% or more): Increased creatinine (16%)
Common (1% to 10%): Pyelonephritis
Uncommon (0.1% to 1%): Nephrolithiasis, anuria, renal colic, renal failure, tubulointerstitial nephritis
Respiratory
Very common (10% or more): Upper respiratory tract infections (23%); cough (11%)
Common (1% to 10%): Pneumonia, epistaxis
Uncommon (0.1% to 1%): Pneumonitis, hemoptysis, bronchospasm, chylothorax, dyspnea, respiratory arrest, respiratory failure[Ref]
Endocrine
Very common (10% or more): Thyroid stimulating hormone (TSH) elevation (18.6%)
Common (1% to 10%): Hypothyroidism
More about vandetanib
- Check interactions
- Compare alternatives
- Drug images
- Dosage information
- During pregnancy
- Drug class: EGFR inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
References
1. Product Information. Vandetanib (vandetanib). Astra-Zeneca Pharmaceuticals. 2011.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.