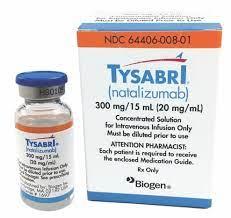
Natalizumab Dosage
Medically reviewed by Drugs.com. Last updated on Sep 13, 2023.
Applies to the following strengths: 300 mg/15 mL
Usual Adult Dose for:
Additional dosage information:
Usual Adult Dose for Multiple Sclerosis
300 mg IV over 1 hour once every 4 weeks
Comments:
- Only prescribers registered in the MS TOUCH (R) Prescribing Program may prescribe this drug for multiple sclerosis.
- Patients should be observed during the infusion and for one hour after the infusion is complete.
Use: Multiple Sclerosis (MS): As monotherapy for the treatment of patients with relapsing forms of multiple sclerosis
Usual Adult Dose for Crohn's Disease - Maintenance
300 mg IV over 1 hour once every 4 weeks
Comments:
- Only prescribers registered in the CD TOUCH (R) Prescribing Program may prescribe this drug for Crohn's disease.
- This drug should not be used with concomitant immunosuppressants (e.g., 6-mercaptopurine, azathioprine, cyclosporine, methotrexate) or concomitant inhibitors of TNF-alpha.
- Aminosalicylates may be continued during treatment with this drug.
- If the patient has not experienced therapeutic benefit by 12 weeks of induction therapy, this drug should be discontinued.
- For patients who start this drug while on chronic oral corticosteroids, steroid tapering should commence as soon as a therapeutic benefit of this drug has occurred; if the patient cannot be tapered off of oral corticosteroids within 6 months of starting this drug, then this drug should be discontinued.
- Other than the initial 6 month taper, prescribers should consider discontinuing this drug for patients who require additional steroid use that exceeds 3 months in a calendar year to control their Crohn's disease.
- Patients should be observed during the infusion and for one hour after the infusion is complete.
Use: Crohn's Disease (CD): For inducing and maintaining clinical response and remission in adult patients with moderately to severely active Crohn's disease with evidence of inflammation who have had an inadequate response to, or are unable to tolerate conventional CD therapies and inhibitors of TNF-alpha
Renal Dose Adjustments
Data not available
Liver Dose Adjustments
Data not available
Precautions
US REMS: The US FDA requires a Risk Evaluation and Mitigation Strategy (REMS) for natalizumab (R). It includes a medication guide, elements to assure safe use, and implementation system. For additional information: www.fda.gov/REMS
RESTRICTED DISTRIBUTION PROGRAM:
- Because of the risk of PML, this drug is available only through a special restricted distribution program called the TOUCH (R) Prescribing Program.
- Only prescribers, infusion centers, and pharmacies associated with infusion centers registered with the program are able to prescribe, distribute, or infuse the product.
- For physicians and patients, the TOUCH (R) Prescribing Program has 2 components:
2) CD TOUCH (R) (for patients with Crohn's disease)
Requirements of the TOUCH (R) Prescribing Program include the following:
Prescribers must be certified and comply with the following:
- Review the TOUCH (R) Prescribing Program prescriber educational materials, including the full prescribing information.
- Educate patients on the benefits and risks of treatment with this drug, ensure that patients receive the Medication Guide, and encourage them to ask questions.
- Review, complete, and sign the Patient-Prescriber Enrollment Form.
- Evaluate patients 3 months after the first infusion, 6 months after the first infusion, every 6 months thereafter, and for at least 6 months after discontinuing therapy.
- Determine every 6 months whether patients should continue on treatment and, if so, authorize treatment for another 6 months.
- Submit to Biogen Idec the "TYSABRI (R) Patient Status Report and Reauthorization Questionnaire" 6 months after initiating treatment and every 6 months thereafter.
- Complete an "Initial Discontinuation Questionnaire" when therapy is discontinued, and a "6-Month Discontinuation Questionnaire" following discontinuation of therapy.
- Report cases of PML, hospitalizations due to opportunistic infections, and deaths to Biogen Idec at 1-800-456-2255 as soon as possible.
- Patients must be enrolled in the TOUCH (R) Prescribing Program, read the Medication Guide, understand the risks associated with this drug, and complete and sign the Patient-Prescriber Enrollment Form.
- Pharmacies and infusion centers must be specially certified to dispense or infuse this drug.
US BOXED WARNINGS:
PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY:
- This drug increases the risk of progressive multifocal leukoencephalopathy (PML), an opportunistic viral infection of the brain that usually leads to death or severe disability.
- Risk factors for the development of PML include duration of therapy, prior use of immunosuppressants, and presence of anti-JCV antibodies. These factors should be considered in the context of expected benefit when initiating and continuing treatment.
- Healthcare professionals should monitor patients on this drug for any new sign or symptom that may be suggestive of PML.
- This drug should be withheld immediately at the first sign or symptom suggestive of PML.
- For diagnosis, an evaluation that includes a gadolinium-enhanced magnetic resonance imaging (MRI) scan of the brain and, when indicated, cerebrospinal fluid analysis for JC viral DNA are recommended.
- Because of the risk of PML, this drug is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the TOUCH Prescribing Program.
Safety and efficacy have not been established in patients younger than 18 years.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Therapy with this drug should be initiated and supervised by neurologists, in centers with timely access to MRI.
- This drug should be administered within 8 hours of preparation.
Storage advice:
- Consult the manufacturer product information.
Reconstitution/preparation techniques:
- Consult the manufacturer product information.
General:
- This drug should not be administered as an IV push or bolus.
- In CD, discontinue in patients that have not experienced therapeutic benefit by 12 weeks of induction therapy, and in patients that cannot discontinue chronic concomitant steroids within six months of starting therapy.
Monitoring:
- Patients should be observed during the infusion and for one hour after the infusion is complete for adverse reactions.
Frequently asked questions
- Does Tysabri suppress the immune system?
- How long can you take Tysabri for?
- Is Tysabri a form of chemotherapy?
- Does Tysabri cause cancer?
- How many biosimilars have been approved in the United States?
- How to prevent hair loss from Tysabri (natalizumab)?
More about natalizumab
- Check interactions
- Compare alternatives
- Reviews (101)
- Side effects
- During pregnancy
- Drug class: selective immunosuppressants
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.