Fluoxetine Dosage
Medically reviewed by Drugs.com. Last updated on Apr 22, 2024.
Applies to the following strengths: 90 mg; 10 mg; 20 mg; 40 mg; 60 mg; 20 mg/5 mL; 15 mg
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Bulimia
Immediate-release oral formulations: 60 mg orally once a day in the morning
Comments:
- Some patients may need to be started at a lower dose and titrated up over several days to the recommended dose.
- Daily doses greater than 60 mg have not been systematically studied for the treatment of bulimia.
Use: Acute and maintenance treatment of binge-eating and vomiting behaviors in moderate to severe bulimia nervosa
Usual Adult Dose for Depression
Immediate-release oral formulations:
Initial dose: 20 mg orally once a day in the morning, increased after several weeks if sufficient clinical improvement is not observed
Maintenance dose: 20 to 60 mg orally per day
Maximum dose: 80 mg orally per day
Delayed release oral capsules:
Initial dose: 90 mg orally once a week, commenced 7 days after the last daily dose of immediate-release fluoxetine 20 mg formulations.
Comments:
- Doses above 20 mg per day may be given in divided doses, in the morning and at noon.
- The full effect may be delayed until after at least 4 weeks of treatment.
- If a satisfactory response with the once weekly oral fluoxetine is not maintained, a change back to daily fluoxetine dosing using the immediate-release oral formulations should be considered.
- Acute episodes of Major Depressive Disorder (MDD) require several months or longer of sustained pharmacologic therapy.
- Whether the dose needed to induce remission is the same as the dose needed to maintain and/or sustain euthymia is unknown.
Use: Acute and maintenance treatment of MDD
Usual Adult Dose for Obsessive Compulsive Disorder
Immediate-release oral formulations:
- Initial dose: 20 mg orally once a day in the morning, increased after several weeks if sufficient clinical improvement is not observed.
- Maintenance dose: 20 to 60 mg orally per day
- Maximum dose: 80 mg orally per day
Comments:
- Doses above 20 mg per day may be given in divided doses, in the morning and at noon.
- The full effect may be delayed until after at least 5 weeks of treatment.
Use: Acute and maintenance treatment of obsessions and compulsions in patients with Obsessive Compulsive Disorder (OCD)
Usual Adult Dose for Panic Disorder
Immediate-release oral formulations:
- Initial dose: 10 mg orally once a day, increased after one week to 20 mg orally once a day
- Maintenance dose: 20 to 60 mg orally per day
- Maximum dose: 60 mg orally per day
Comments:
- Doses above 20 mg per day may be given in divided doses, in the morning and at noon.
- A dose increase may be considered after several weeks if clinical improvement is not observed.
- Doses greater than 60 mg per day have not been systematically studied for the treatment of panic disorder.
Use: Acute treatment of panic disorder with/without agoraphobia
Usual Adult Dose for Premenstrual Dysphoric Disorder
Immediate-release oral formulations:
Initial dose:
- Continuous regimen: 20 mg orally once a day on every day of the menstrual cycle
- Cyclic regimen: 20 mg orally once a day starting 14 days prior to the anticipated start of menstruation through to the first full day of menses, and repeated with each new cycle
Maximum dose: 80 mg orally per day
Comments:
- A daily dose of 60 mg has not been shown to be significantly more effective than 20 mg daily.
- Daily doses above 60 mg have not been systematically studied in patients with this condition.
- The 20 mg daily dosage has been shown to be effective for up to 6 months of treatment.
Use: Treatment of premenstrual dysphoric disorder (PMDD)
Usual Pediatric Dose for Depression
Immediate-release oral formulations:
8 to 18 years:
Initial dose: 10 to 20 mg orally once a day; the 10 mg daily dose may be increased after one week to 20 mg orally once a day
Lower weight children:
- Initial dose: 10 mg orally once a day, increased to 20 mg orally once a day after several weeks if sufficient clinical improvement is not observed
- Maintenance dose: 10 to 20 mg orally once a day
Comments:
- The full effect may be delayed until after at least 4 weeks of treatment.
- The potential risks versus clinical need should be assessed prior to using this drug in children and adolescents.
Use: Acute and maintenance treatment of MDD
Usual Pediatric Dose for Obsessive Compulsive Disorder
Immediate-release oral formulations:
7 to 17 years:
Adolescents and higher weight children:
- Initial dose: 10 mg orally once a day, increased to 20 mg orally once a day after 2 weeks
- Maintenance dose: 20 to 60 mg orally per day
- Maximum dose: 60 mg orally per day
Lower weight children:
- Initial dose: 10 mg orally once a day, increased after several weeks if sufficient clinical improvement is not observed
- Maintenance dose: 20 to 30 mg orally once a day
- Maximum dose: 60 mg orally per day
Comments:
- Additional dose increases may be considered after several more weeks if clinical improvement is insufficient.
- Doses above 20 mg per day may be given in divided doses, in the morning and at noon.
- In lower weight children, there is minimal experience with doses greater than 20 mg per day, and none with doses greater than 60 mg per day.
- The full effect may be delayed until after at least 5 weeks of treatment.
- The potential risks versus clinical need should be assessed prior to using this drug in children and adolescents.
Use: Acute and maintenance treatment of obsessions and compulsions in patients with
OCD
Renal Dose Adjustments
No adjustment recommended
Liver Dose Adjustments
Liver dysfunction (including cirrhosis):
- Immediate-release oral formulations: Lower or less frequent dosing may be appropriate in these patients
- Delayed-release oral capsules: Data not available
Dose Adjustments
A lower or less frequent dose should be considered in elderly patients, and/or those on multiple concomitant medications or with concurrent disease.
Switching from:
- MAOI therapy to this drug: At least 14 days should elapse
- This drug to MAOI therapy: At least 5 weeks should elapse
- This drug to tricyclic antidepressant (TCA) therapy: The dose of the TCA may need to be reduced and plasma levels temporarily monitored
Treatment withdrawal:
- A gradual dose reduction is recommended instead of abrupt cessation where possible.
- If intolerable symptoms occur, it is recommended to consider resuming the previously prescribed dose and to decrease the dose at a more gradual rate.
Precautions
US BOXED WARNINGS:
SUICIDAL THOUGHTS AND BEHAVIORS:
- Antidepressants increase the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term studies. These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients over age 24; there was a reduction in risk with antidepressant use in patients aged 65 and older.
- In patients of all ages who are started on antidepressant therapy, monitor closely for worsening and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber.
- Fluoxetine is not approved for use in children less than 7 years of age.
Safety and efficacy have not been established in pediatric patients younger than 7 years (OCD) and 8 years of age (MDD).
Safety and efficacy in the treatment of PMDD have not been established in pediatric patients.
Consult WARNINGS section for additional precautions.
Dialysis
No adjustment recommended
Other Comments
Administration advice:
- A once a day dose should be taken in the morning; doses greater than 20 mg per day may be divided into morning and noon doses.
- Oral dissolving tablets may be swallowed with fluid or dispersed in water just prior to administration; the tablets should not be crushed or chewed.
- Because fluoxetine may cause insomnia, night-time dosing should be limited to those patients experiencing sedation.
Storage requirements:
- Oral solution and some tablet formulations: Protect from light.
General:
- The delayed release oral capsule (given weekly) contains enteric-coated pellets.
- Oral capsules, tablets, oral solution, and delayed release oral capsules (given weekly) are bioequivalent
- Changes in dose will not be fully reflected in plasma for several weeks due to the long elimination half-lives of fluoxetine and its major active metabolite.
- The need for ongoing treatment should be regularly reviewed.
- Patients should be maintained on the lowest effective dose.
- Avoid use as monotherapy in treatment-resistant depression i.e., patients who do not respond to two antidepressants of adequate dose and duration in the current episode.
Monitoring:
- Cardiovascular: ECG monitoring (in patients with risk factors for QT-interval prolongation)
- Hepatic: Liver function
- Metabolic: Electrolyte levels (especially in patients at risk of hyponatremia), weight (especially in underweight depressed or bulimic patients)
- Nervous system: Seizure activity (especially in patients at risk of seizures), serotonin syndrome
- Psychiatric: Emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Patient advice:
- Tell your healthcare provider about all of the medicines that you take, including prescription and non-prescription medicines.
- This medicine may increase the risk of suicidal thoughts and behavior. Be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Report any behavior of concern to your healthcare provider as soon as possible.
- Patients should be advised to speak to a healthcare provider if they are pregnant, intend to become pregnant, or are breastfeeding.
- This medicine may cause impaired judgment, thinking, or motor skills; do not drive a car or operate dangerous machinery until you know how this drug affects you.
Frequently asked questions
- SSRIs vs SNRIs - What's the difference between them?
- Is Prozac (fluoxetine) safe for dogs?
- Prozac vs Zoloft - What are the Differences & Similarities?
- What are some common side effects of antidepressants?
- Taking fluoxetine, what can I use for a bad cough from cold or strep throat?
More about fluoxetine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2,203)
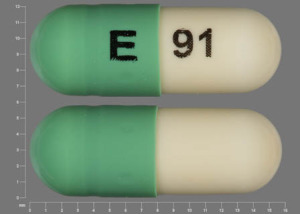
- Drug images
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: selective serotonin reuptake inhibitors
- Breastfeeding
Patient resources
- Fluoxetine drug information
- Fluoxetine Capsules and Tablets
- Fluoxetine Capsules and Tablets (PMDD)
- Fluoxetine Delayed-Release Capsules
- Fluoxetine Solution
Other brands
Prozac, Sarafem, Prozac Weekly, Rapiflux, Selfemra
Professional resources
- FLUoxetine monograph
- Fluoxetine (FDA)
- Fluoxetine Capsules (FDA)
- Fluoxetine Delayed Release Capsules (FDA)
- Fluoxetine Solution (FDA)
Other brands
Prozac, Sarafem, Prozac Weekly
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.