Alphanate Dosage
Generic name: HUMAN COAGULATION FACTOR VIII/VON WILLEBRAND FACTOR COMPLEX 250[iU] in 5mL; water 1mL in 1mL
Dosage form: injection
Drug class: Miscellaneous coagulation modifiers
Medically reviewed by Drugs.com. Last updated on Jun 6, 2023.
For intravenous injection after reconstitution only
- Treatment with ALPHANATE should be initiated under the supervision of a physician experienced in the treatment of hemophilia.
- Each vial of ALPHANATE has the antihemophilic factor (AHF) potency (FVIII:C activity) expressed in International Units (IU) FVIII/vial on the label. Additionally, ALPHANATE contains von Willebrand Factor:Ristocetin Cofactor (VWF:RCo), which is expressed in IU VWF:RCo/vial for the treatment of VWD.
Dose
Treatment and Prevention of Bleeding Episodes and Excess Bleeding During and After Surgery in Patients with Hemophilia A
- Dosage and duration of treatment depend on the severity of the FVIII deficiency, the location and extent of bleeding, presence of inhibitors, and the patient’s clinical condition. Careful control of replacement therapy is especially important in cases of major surgery or life-threatening bleeding episodes.
- Dosing requirements and frequency of dosing is calculated on the basis of an expected initial response of 2% of normal FVIII:C increase per IU FVIII:C/kg body weight administered.1The expected in vivo peak increase in FVIII level expressed as IU/dL (or % of normal) can be estimated using the following formulas:
Dosage (international units) = body weight (kg) x desired FVIII rise (IU/dL or % normal) x 0.5 (IU/kg per IU/dL)
or
IU/dL (or % of normal) = [Total Dose (IU)/body weight (kg)] x 2
- Titrate dose and frequency to the patient’s clinical response, including individualized needs, severity of the deficiency, severity of the hemorrhage, presence of inhibitors, and FVIII level desired. Patients may vary in their pharmacokinetic (e.g., half-life, in vivo recovery) and clinical responses to ALPHANATE.
- Table 1 provides dosage guidelines for the control and prevention of bleeding episodes in hemophilia A patients. Dosing should aim at maintaining a plasma factor VIII activity level at or above the plasma levels (in IU/dL or in % of normal) outlined in the table.
| Type of Bleeding | FVIII:C Level Required(% of normal) | Doses(IU/kg) | Frequency of Doses(hours) | Duration of Therapy (days) |
| Minor • Large bruises • Significant cuts or scrapes • Uncomplicated joint hemorrhage |
30 | 15 | 12 (twice daily) | Until hemorrhage stops and healing has been achieved (1–2 days). |
| Moderate • Nose, mouth and gum bleeds • Dental extractions Hematuria |
50 | 25 | 12 (twice daily) |
Until healing has been achieved (2–7 days, on average). |
| Major • Joint hemorrhage • Muscle hemorrhage • Major trauma • Hematuria • Intracranial and intraperitoneal bleeding |
80–100 | Initial: 40–50 Maintenance: 25 |
12 (twice daily) |
For at least 3–5 days Until healing has been achieved for up to 10 days. Intracranial hemorrhage may require prophylaxis therapy for up to 6 months. |
| Surgery | Prior to surgery: 80–100 After surgery: 60–100 |
40–50 30–50 |
Once 12 (twice daily) |
Prior to surgery For the next 7–10 days, or until healing has been achieved. |
- Monitoring parameters:
- Monitor plasma FVIII levels periodically to evaluate individual patient response to the dosage regimen.
- If dosing studies have determined that a particular patient exhibits a lower/higher than expected response and shorter/longer half-life, adjust the dose and the frequency of dosing accordingly.
- Failure to achieve the expected plasma FVIII:C level or to control bleeding after an appropriately calculated dosage may be indicative of the development of an inhibitor (an antibody to FVIII:C). Quantitate the inhibitor level by appropriate laboratory procedures and document its presence. Treatment with AHF in such cases must be individualized.2
Treatment and Prevention of Excess Bleeding During and After Surgery or Other Invasive Procedures in Patients with von Willebrand Disease
- The ratio of VWF:RCo to FVIII in ALPHANATE varies by lot, so with each new lot, check IU VWF:RCo/vial to ensure accurate dosing.
- Dosage and duration of treatment depend on the severity of the VWF deficiency, the location and extent of bleeding, and the patient’s clinical condition. Careful control of replacement therapy is especially important in cases of major surgery or life-threatening bleeding episodes.
- The median incremental in vivo recoveries of VWF:RCo and FVIII:C were 3.12 (IU/dL)/(IU/kg) [mean, 3.29 ± 1.46 (IU/dL)/(IU/kg); range: 1.28 to 5.73 (IU/dL)/(IU/kg)] for VWF:RCo and 1.95 (IU/dL)/(IU/kg) [mean, 2.13 ± 0.58 (IU/dL)/(IU/kg); range: 1.33 to 3.32 (IU/dL)/(IU/kg)] for FVIII:C.
- Table 2 provides dosing guidelines for pediatric and adult patients with von Willebrand Disease.3-6
|
a The therapeutic goal is referenced in the NHLBI Guidelines.7 |
||
|
b The safety parameter is extracted from Mannucci 2009.8 |
||
| Minor Surgery/Bleeding | ||
| Parameter | VWF:RCo | Target FVIII:C Activity Levels |
| Pre-operative/pre-procedure dose: | Adults: 60 IU VWF:RCo/kg body weight. Pediatrics: 75 IU VWF:RCo/kg body weight. |
40-50 IU/dL |
| Maintenance dose: | Adults: 40 to 60 IU VWF:RCo/kg body weight at 8 to 12 hour intervals as clinically needed for 1-3 days. Pediatrics: 50 to 75 IU VWF:RCo/kg body weight at 8 to 12 hour intervals as clinically needed for 1-3 days. |
40-50 IU/dL |
| Therapeutic Goal (Trough)a : | >50 IU/dL | >50 IU/dL |
| Safety Monitoring: | Peak and trough at least once daily | Peak and trough at least once daily |
| Safety Parameterb : | Should not exceed 150 IU/dL | Should not exceed 150 IU/dL |
| Major Surgery/Bleeding | ||
| Parameter | VWF:RCo | Target FVIII:C Activity Levels |
| Pre-operative/pre-procedure dose: | Adults: 60 IU VWF:RCo/kg body weight. Pediatrics: 75 IU VWF:RCo/kg body weight. |
100 IU/dL |
| Maintenance dose: | Adults: 40 to 60 IU VWF:RCo/kg body weight at 8 to 12 hour intervals as clinically needed for at least 3-7 days. Pediatrics: 50 to 75 IU VWF:RCo/kg body weight at 8 to 12 hour intervals as clinically needed for at least 3-7 days. |
100 IU/dL |
| Therapeutic Goal (Trough)a : | >50 IU/dL | >50 IU/dL |
| Safety Monitoring: | Peak and trough at least daily | Peak and trough at least daily |
| Safety Parameterb: | Should not exceed 150 IU/dL | Should not exceed 150 IU/dL |
Reconstitution
- Always use aseptic technique.
- Ensure that concentrate (ALPHANATE) and diluent (Sterile Water for Injection, USP) are at room temperature (but not above 37 ˚C) before reconstitution.
- Remove the plastic flip off cap from the diluent vial.
- Gently swab the exposed stopper surface with a cleansing agent such as alcohol trying to avoid leaving any excess cleansing agent on the stopper.
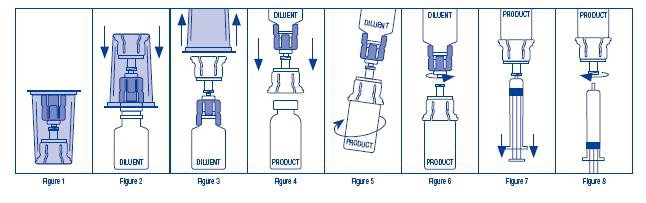
- Open the Mix2Vial package by peeling away the lid (Figure 1). Leave the Mix2Vial in the clear outer packaging.
- Place the diluent vial upright on an even surface and hold the vial tight and pick up the Mix2Vial in its clear outer packaging. Holding the diluent vial securely, push the blue end of the Mix2Vial vertically down through the diluent vial stopper (Figure 2).
- While holding onto the diluent vial, carefully remove the clear outer packaging from the Mix2Vial set, ensuring the Mix2Vial remains attached to the diluent vial (Figure 3).
- Place the product vial upright on an even surface, invert the diluent vial with the Mix2Vial attached.
- While holding the product vial securely on a flat surface, push the clear end of the Mix2Vial set vertically down through the product vial stopper (Figure 4). The diluent will automatically transfer out of its vial into the product vial.
NOTE: If the Mix2Vial is connected at an angle, the vacuum may be released from the product vial and the diluent will not transfer into the product vial. - With the diluent and product vials still attached to the Mix2Vial, gently swirl the product vial to ensure the product is fully dissolved (Figure 5). Reconstitution requires less than 5 minutes. Do not shake the vial.
- Disconnect the Mix2Vial into two separate pieces (Figure 6) by holding each vial adapter and twisting counterclockwise. After separating, discard the diluent vial with the blue end of the Mix2Vial.
- Draw air into an empty, sterile syringe. Keeping the product vial upright with the clear end of the Mix2Vial attached, screw the disposable syringe onto the luer lock portion of the Mix2Vial device by pressing and twisting clockwise. Inject air into the product vial.
- While keeping the syringe plunger depressed, invert the system upside down and draw the reconstituted product into the syringe by pulling the plunger back slowly (Figure 7).
- When the reconstituted product has been transferred into the syringe, firmly hold the barrel of the syringe and the clear vial adapter (keeping the syringe plunger facing down) and unscrew the syringe from the Mix2Vial (Figure 8). Hold the syringe upright and push the plunger until no air is left in the syringe. Attach the syringe to a venipuncture set.
NOTE: If the same patient is to receive more than one vial of concentrate, the contents of two vials may be drawn into the same syringe through a separate unused Mix2Vial set before attaching to the venipuncture set. - When reconstitution procedure is strictly followed, a few small particles may occasionally remain. The Mix2Vial set will remove particles and the labeled potency will not be reduced.
- Discard all reconstitution equipment after use into the appropriate safety container. Do not reuse.
- Use the prepared drug as soon as possible within 3 hours after reconstitution.
Administration
For intravenous use after reconstitution only
- Inspect parenteral drug products visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
- Do not refrigerate after reconstitution. Store reconstituted ALPHANATE at room temperature (not to exceed 30 °C) prior to administration, but administer intravenously within three hours.
- Use plastic disposable syringes.
- Do not administer ALPHANATE at a rate exceeding 10 mL/minute.
- Discard any unused contents into the appropriate safety container.
More about Alphanate (antihemophilic factor/von willebrand factor)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Side effects
- During pregnancy
- Drug class: miscellaneous coagulation modifiers
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.