Trandolapril/verapamil Disease Interactions
There are 20 disease interactions with trandolapril / verapamil.
- Angioedema
- Bone marrow suppression
- Hemodialysis
- Hyperkalemia
- Hypotension
- Aortic stenosis
- Bradyarrhythmia/AV block
- Cardiogenic shock/hypotension
- Coronary artery disease
- Liver disease
- Ventricular tachycardia
- Cirrhosis
- Accessory AV tracts
- CHF/AMI
- Hypertrophic cardiomyopathy
- Liver disease
- Renal dysfunction
- Neuromuscular transmission
- Renal dysfunction
- GI narrowing
ACE inhibitors (applies to trandolapril/verapamil) angioedema
Major Potential Hazard, Moderate plausibility.
The use of these agents is contraindicated in patients with hereditary angioedema or a history of idiopathic angioedema. Patients with a history of angioedema unrelated to ACE inhibitors may be at increased risk of angioedema while receiving an ACE inhibitor. Patients should be advised to immediately report any signs or symptoms suggestive of angioedema (swelling of face, extremities, eyes, lips, or tongue, or difficulty swallowing or breathing) and to stop taking the medication until otherwise directed by their physician. Emergency therapy and/or measures to prevent airway obstruction are required for angioedema involving the tongue, glottis, or larynx. Treatment with ACE inhibitors should be discontinued permanently if angioedema develops in association with therapy.
ACE inhibitors (applies to trandolapril/verapamil) bone marrow suppression
Major Potential Hazard, Moderate plausibility. Applicable conditions: Collagen Vascular Disease, Renal Dysfunction, Bone Marrow Depression/Low Blood Counts
ACE inhibitors may cause bone marrow suppression, rarely in uncomplicated individuals but more frequently in patients with renal impairment, especially if they also have a collagen-vascular disease such as systemic lupus erythematosus or scleroderma. Neutropenia, agranulocytosis, aplastic anemia, hemolytic anemia, eosinophilia and thrombocytopenia have been reported, mostly with captopril. Therapy with ACE inhibitors should be administered cautiously in patients with preexisting blood dyscrasias or complications that may increase the risk of bone marrow depression during ACE inhibitor therapy. Monitoring of blood counts, particularly white blood cells, should be considered.
ACE inhibitors (applies to trandolapril/verapamil) hemodialysis
Major Potential Hazard, Moderate plausibility.
Anaphylactoid reactions have been reported in patients undergoing hemodialysis with high-flux polyacrylonitrile membranes and treated concomitantly with an ACE inhibitor. The frequency and mechanism of this interaction have not been established, and it is not known whether the interaction occurs with other membrane types. Therapy with ACE inhibitors should be administered cautiously in patients requiring hemodialysis.
ACE inhibitors (applies to trandolapril/verapamil) hyperkalemia
Major Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction, Diabetes Mellitus
In patients with hyperkalemia, especially those associated with impaired renal function or congestive heart failure, ACE inhibitors may further raise serum potassium levels. Therapy with ACE inhibitors should be administered cautiously in patients with or predisposed to hyperkalemia, and serum potassium levels should be carefully monitored. Risk factors for the development of hyperkalemia during ACE inhibitor therapy include renal insufficiency, diabetes mellitus, and the concomitant use of potassium-sparing diuretics, potassium supplements, and/or potassium-containing salt substitutes.
ACE inhibitors (applies to trandolapril/verapamil) hypotension
Major Potential Hazard, Moderate plausibility. Applicable conditions: Diarrhea, Vomiting, hemodialysis, Dehydration, Hyponatremia, Ischemic Heart Disease, Cerebrovascular Insufficiency
ACE inhibitors can cause symptomatic hypotension, most often during the initiation of therapy and in patients who are volume- and/or sodium-depleted or treated for congestive heart failure (CHF). Therapy with ACE inhibitors should be administered cautiously in such patients and in those predisposed to hypovolemic or hyponatremic states (e.g., patients on diuretic therapy, especially if it was recently instituted; those on dietary salt restriction; those with severe or prolonged diarrhea or vomiting; and renal dialysis patients). Volume and/or sodium depletion should be corrected prior to initiating therapy with ACE inhibitors, and the patient should be hemodynamically stable. If concomitant diuretics and/or dietary sodium restriction are employed, reducing or temporarily withholding the dosing of diuretics and/or liberalizing dietary sodium intake for 2 to 3 days in advance can help minimize the risk of severe hypotension in patients who are able to tolerate such adjustments. ACE inhibitors should also be used cautiously in patients in whom excessive hypotension may have serious consequences, such as patients with coronary or cerebrovascular insufficiency. Patients at risk for excessive hypotension should initiate ACE inhibitor therapy under very close medical supervision, and followed closely for the first 2 weeks of treatment and whenever the dosage of ACE inhibitor or diuretic is increased.
CCBs (applies to trandolapril/verapamil) aortic stenosis
Major Potential Hazard, High plausibility.
The use of some calcium channel blockers (CCBs) is contraindicated in patients with advanced aortic stenosis. CCBs whose pharmacologic effect is partially dependent on their ability to reduce afterload (e.g., diltiazem, nicardipine, nifedipine, verapamil) may be of less benefit in these patients due to a fixed impedance to flow across the aortic valve and may, in fact, worsen rather than improve myocardial oxygen balance. Rarely, heart failure has developed following the initiation of these CCBs, particularly in patients receiving concomitant beta-blocker therapy.
CCBs (applies to trandolapril/verapamil) bradyarrhythmia/AV block
Major Potential Hazard, High plausibility. Applicable conditions: Heart Block, Sinus Node Dysfunction
The use of some calcium channel blockers (CCBs) is contraindicated in patients with severe bradyarrhythmia, sick sinus syndrome (unless a functioning pacemaker is present), or heart block greater than the first degree (unless a functioning pacemaker is present). CCBs like bepridil, diltiazem and verapamil have a negative effect on AV conduction and the SA node and may exacerbate these conditions.
CCBs (applies to trandolapril/verapamil) cardiogenic shock/hypotension
Major Potential Hazard, High plausibility.
In general, calcium channel blockers (CCBs) should not be used in patients with hypotension (systolic pressure < 90 mm Hg) or cardiogenic shock. Due to potential negative inotropic and peripheral vasodilating effects, the use of CCBs may further depress cardiac output and blood pressure, which can be detrimental in these patients. The use of verapamil and diltiazem is specifically contraindicated under these circumstances.
CCBs (applies to trandolapril/verapamil) coronary artery disease
Major Potential Hazard, Low plausibility. Applicable conditions: Ischemic Heart Disease
Increased frequency, duration, and/or severity of angina, as well as acute myocardial infarction, have rarely developed during initiation or dosage increase of calcium channel blockers (CCBs), particularly in patients with severe obstructive coronary artery disease and those treated with immediate-release formulations. The mechanism of this effect is not established. Therapy with CCBs should be administered cautiously in patients with significant coronary artery disease.
CCBs (applies to trandolapril/verapamil) liver disease
Major Potential Hazard, High plausibility.
Calcium channel blockers (CCBs) are extensively metabolized by the liver. The half-lives of CCBs may be prolonged substantially in patients with severe hepatic impairment, with the potential for significant drug accumulation. In addition, the use of some CCBs has been associated with elevations in serum transaminases, both with and without concomitant elevations in alkaline phosphatase and bilirubin. While these effects may be transient and reversible, some patients have developed cholestasis or hepatocellular injury. Therapy with CCBs should be administered cautiously and often at reduced dosages in patients with significantly impaired hepatic function. Periodic monitoring of liver function is advised.
Diltiazem/verapamil IV (applies to trandolapril/verapamil) ventricular tachycardia
Major Potential Hazard, High plausibility. Applicable conditions: Ventricular Arrhythmia
The use of intravenous diltiazem or verapamil is contraindicated in patients with ventricular tachycardia. IV administration of a calcium channel blocker can precipitate cardiac arrest in such patients. Marked hemodynamic deterioration and ventricular fibrillation have occurred in patients with wide-complex ventricular tachycardia (QRS >= 0.12 seconds) treated with IV verapamil.
Trandolapril (applies to trandolapril/verapamil) cirrhosis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
The clearance of trandolapril and its active metabolite, trandolaprilat, may be decreased in patients with hepatic cirrhosis. Following oral administration in patients with mild to moderate alcoholic cirrhosis, plasma concentrations of trandolapril and trandolaprilat were 9-fold and 2-fold greater, respectively, than in normal subjects. However, the inhibition of ACE activity was not affected. The manufacturer states that lower initial dosages should be considered in patients with hepatic insufficiency.
Verapamil (applies to trandolapril/verapamil) accessory AV tracts
Major Potential Hazard, High plausibility. Applicable conditions: Preexcitation Syndrome
The use of verapamil is contraindicated for the management of atrial flutter or fibrillation in patients with an accessory AV tract (e.g., those with Wolff-Parkinson-White or Lown-Ganong-Levine syndrome). Intravenous verapamil has been reported to cause ventricular fibrillation and cardiac arrest in such patients, the mechanism of which is related to the drug's ability to shorten the refractory period and accelerate antegrade conduction within the accessory pathway. Although these events have not been associated with chronic use of oral verapamil, a similar risk may exist.
Verapamil (applies to trandolapril/verapamil) CHF/AMI
Major Potential Hazard, High plausibility. Applicable conditions: Congestive Heart Failure, Myocardial Infarction
The use of verapamil is contraindicated in patients with severe left ventricular dysfunction (e.g., ejection fraction < 30%) or moderate to severe symptoms of cardiac failure and in patients with any degree of ventricular dysfunction if they are receiving a beta-adrenergic blocker. Likewise, verapamil should not be given to patients with acute myocardial infarction and pulmonary congestion documented by X-ray on admission, since associated heart failure may be acutely worsened. Verapamil has a negative inotropic effect, which in most patients is compensated by a simultaneous reduction in afterload (i.e. decreased systemic vascular resistance) without a net impairment of ventricular performance. However, congestive heart failure or pulmonary edema have developed in approximately 2% of patients treated with verapamil. Mild symptoms of cardiac failure should be under control, if possible, prior to initiating verapamil therapy.
Verapamil (applies to trandolapril/verapamil) hypertrophic cardiomyopathy
Major Potential Hazard, Moderate plausibility.
The use of verapamil in patients with hypertrophic cardiomyopathy, or idiopathic hypertrophic subaortic stenosis, has been associated with serious side effects such as pulmonary edema, severe hypotension, sinus bradycardia, AV block, sinus arrest, and death. However, a causal relationship has not been established. Therapy with verapamil should be administered cautiously in patients with hypertrophic cardiomyopathy. Dosage reduction or drug discontinuation may be required if severe adverse effects occur.
ACE inhibitors (applies to trandolapril/verapamil) liver disease
Moderate Potential Hazard, Moderate plausibility.
Rarely, elevations of liver enzymes and/or serum bilirubin have occurred with the use of ACE inhibitors. Patients receiving ACE inhibitors who develop jaundice or marked elevations of hepatic enzymes should discontinue the ACE inhibitor and receive appropriate medical follow-up.
ACE inhibitors (applies to trandolapril/verapamil) renal dysfunction
Moderate Potential Hazard, Moderate plausibility.
With the exception of fosinopril, ACE inhibitors (and/or their active metabolites in some cases) are primarily eliminated by the kidney and may accumulate in patients with renal impairment. ACE inhibitors can also worsen renal function in some patients by blocking the effect of angiotensin II-mediated efferent arteriolar vasoconstriction, thereby decreasing glomerular filtration. Therapy with ACE inhibitors should be administered cautiously in patients with preexisting renal dysfunction, particularly those with renovascular disease. Patients with moderate to severe renal impairment usually require lower or less frequent doses and smaller increments in dose. In addition, a dosage reduction or discontinuation of any concomitantly administered diuretics may be helpful. Fosinopril probably does not require dosage adjustments unless hepatic function is also significantly impaired.
In patients with bilateral renal artery stenosis or renal artery stenosis in a solitary kidney, ACE inhibitors may reduce renal perfusion to a critically low level. Renal function should be monitored closely for the first few weeks of therapy.
Verapamil (applies to trandolapril/verapamil) neuromuscular transmission
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Myopathy, Myoneural Disorder
Verapamil has been reported to decrease neuromuscular transmission in patients with Duchenne's muscular dystrophy and to prolong recovery from the neuromuscular blocking agent, vecuronium. Therapy with verapamil should be administered cautiously in patients with attenuated neuromuscular transmission or myopathy, since these conditions may be exacerbated. A reduced dosage may be appropriate.
Verapamil (applies to trandolapril/verapamil) renal dysfunction
Moderate Potential Hazard, High plausibility.
Approximately 70% of an administered dose of verapamil is excreted as metabolites in the urine. The primary metabolite, norverapamil, has about 20% the cardiovascular activity and can reach steady-state plasma concentrations approaching those of the parent drug. Patients with impaired renal function may be at greater risk for adverse effects due to drug and metabolite accumulation. Therapy with verapamil should be administered cautiously in such patients, with appropriate monitoring for excessive pharmacologic effects (e.g., abnormal prolongation of PR interval) and the dosage adjusted accordingly as necessary.
Verapamil HS (applies to trandolapril/verapamil) GI narrowing
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Gastrointestinal Obstruction
The controlled-onset, extended-release formulation of verapamil (Covera-HS) contains a non-deformable material. There have been rare reports of obstructive symptoms in patients with known strictures following the ingestion of similar sustained-release products. Therapy with the controlled-onset, extended-release formulation of verapamil should be administered cautiously in patients with preexisting severe gastrointestinal narrowing or obstruction, whether pathologic or iatrogenic.
Trandolapril/verapamil drug interactions
There are 805 drug interactions with trandolapril / verapamil.
Trandolapril/verapamil alcohol/food interactions
There are 4 alcohol/food interactions with trandolapril / verapamil.
More about trandolapril / verapamil
- trandolapril/verapamil consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
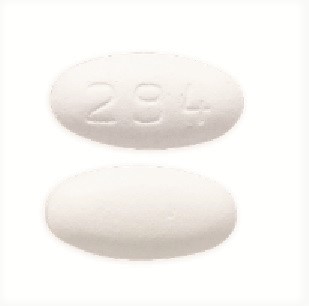
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: ACE inhibitors with calcium channel blocking agents
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.