Tocilizumab Disease Interactions
There are 8 disease interactions with tocilizumab.
- Infections
- Tuberculosis
- Demyelinating disorders
- Gastrointestinal perforation
- Lipid abnormalities
- Liver dysfunction
- Neutropenia/thrombocytopenia
- Renal impairment
Tocilizumab (applies to tocilizumab) infections
Major Potential Hazard, Moderate plausibility. Applicable conditions: Infection - Bacterial/Fungal/Protozoal/Viral
Serious and sometimes fatal infections due to bacterial, mycobacterial, invasive fungal, viral, or other opportunistic pathogens have been reported in patients receiving tocilizumab; the most common serious infections reported included pneumonia, urinary tract infection, cellulitis, herpes zoster, gastroenteritis, diverticulitis, sepsis, and bacterial arthritis. Tocilizumab should not be administered in patients with an active infection, including localized infections. The risks and benefits of treatment should be considered before starting tocilizumab in patients: with chronic/recurrent infection, who have been exposed to tuberculosis, with history of serious/opportunistic infection, who have resided/traveled in areas of endemic tuberculosis/mycoses, or with underlying conditions that may predispose them to infection. Patients should be closely monitored for signs/symptoms of infection during and after tocilizumab treatment as signs/symptoms of acute inflammation may be reduced due to suppression of acute phase reactants. If a serious infection, an opportunistic infection, or sepsis develops, tocilizumab should be interrupted until the infection is controlled. A patient who develops a new infection during treatment with tocilizumab should undergo a prompt and complete diagnostic workup appropriate for an immunocompromised patient; appropriate antimicrobial therapy should be started, and the patient should be monitored closely.
Patients with coronavirus disease 2019 (COVID-19) should be monitored for signs/symptoms of new infections during and after tocilizumab treatment. The risks and benefits of tocilizumab in COVID-19 patients with other concomitant infections should be considered.
References
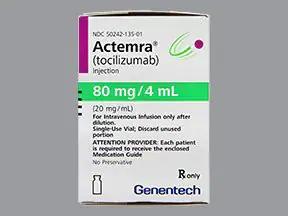
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab (applies to tocilizumab) tuberculosis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Tuberculosis -- Latent, History - Tuberculosis, Tuberculosis -- Active
Tocilizumab should not be given to patients with active tuberculosis (TB) infection. Patients should be evaluated for TB risk factors and tested for latent infection before starting tocilizumab and during therapy; testing for latent infection is not necessary before starting tocilizumab in patients with coronavirus disease 2019 (COVID-19). If positive for latent TB, patients should be treated with standard antimycobacterial therapy before starting tocilizumab. Anti-TB therapy should be considered prior to starting tocilizumab in patients with history of latent/active TB in whom an adequate course of treatment cannot be confirmed, and for patients with a negative test for latent TB but having risk factors for TB infection. Consultation with a physician with expertise in the treatment of TB is recommended to aid in the decision about whether initiating anti-TB therapy is appropriate for an individual patient. Patients should be closely monitored for signs/symptoms of TB, including patients who tested negative for latent TB infection prior to initiating therapy.
References
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab (applies to tocilizumab) demyelinating disorders
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Multiple Sclerosis
Clinical studies have reported that tocilizumab may have an effect on demyelinating disorders such as multiple sclerosis and chronic inflammatory demyelinating polyneuropathy. Patients should be monitored for signs/symptoms potentially indicative of demyelinating disorders. Caution should be exercised when considering the use of tocilizumab in patients with preexisting or recent onset demyelinating disorders.
References
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab (applies to tocilizumab) gastrointestinal perforation
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diverticulitis
The use of tocilizumab may cause gastrointestinal (GI) perforation. Tocilizumab should be used with caution in patients who may be at increased risk for GI perforation. Patients with new onset abdominal symptoms should be evaluated promptly for early detection of GI perforation.
References
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab (applies to tocilizumab) lipid abnormalities
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperlipidemia
Tocilizumab treatment was associated with increases in lipid parameters (e.g., total cholesterol, triglycerides, low-density lipoprotein [LDL] cholesterol, and/or high-density lipoprotein [HDL] cholesterol). Lipid parameters should be assessed about 4 to 8 weeks after initiation of therapy. Patients should be managed according to clinical guidelines for the management of hyperlipidemia.
References
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab (applies to tocilizumab) liver dysfunction
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
The safety and efficacy of tocilizumab have not been studied in patients with liver dysfunction, including patients with positive HBV and HCV serology. Treatment with tocilizumab is not recommended in patients with active liver disease or liver dysfunction.
Treatment with tocilizumab was associated with a higher incidence of transaminase elevations. For patients with rheumatoid arthritis (RA), giant cell arteritis (GCA), or systemic sclerosis-associated interstitial lung disease (SSc-ILD), a liver test panel (serum ALT, AST, alkaline phosphatase, total bilirubin) should be obtained before starting tocilizumab, every 4 to 8 weeks for the first 6 months of therapy, and every 3 months thereafter. Tocilizumab should not be started in patients with RA, GCA, or SSc-ILD with elevated ALT or AST greater than 1.5 times the upper limit of normal (1.5 x ULN) and should be discontinued in those who develop elevated ALT or AST greater than 5 x ULN. Modifications should be based on increased transaminases. A similar pattern of liver enzyme elevation was seen with tocilizumab in patients with polyarticular juvenile idiopathic arthritis (PJIA) or systemic juvenile idiopathic arthritis (SJIA); liver test panel should be monitored at the second dose and thereafter every 4 to 8 weeks for PJIA and every 2 to 4 weeks for SJIA.
Patients hospitalized with coronavirus disease 2019 (COVID-19) may have elevated ALT or AST levels; multi-organ failure with liver involvement is a complication of severe COVID-19. The decision to use tocilizumab should balance the potential benefit of treating COVID-19 against the potential risks of acute therapy. Tocilizumab should not be started in patients with COVID-19 who have elevated ALT or AST greater than 10 x ULN. ALT and AST should be monitored during treatment.
References
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab (applies to tocilizumab) neutropenia/thrombocytopenia
Moderate Potential Hazard, Moderate plausibility.
Tocilizumab treatment was associated with a higher incidence of neutropenia and a reduction in platelet counts. Tocilizumab should not be started in patients with rheumatoid arthritis (RA), giant cell arteritis (GCA), or systemic sclerosis-associated interstitial lung disease (SSc-ILD) who have a low neutrophil count (i.e., absolute neutrophil count [ANC] less than 2000 cells/mm3) or a platelet count less than 100,000 cells/mm3. Tocilizumab is not recommended in patients with RA, GCA, or SSc-ILD who develop an ANC less than 500 cells/mm3 or a platelet count less than 50,000 cells/mm3. Neutrophils and platelets should be monitored in these patients 4 to 8 weeks after the start of therapy and every 3 months thereafter; modifications should be based on ANC results and platelet counts. A similar pattern of low neutrophil and platelet counts was seen with tocilizumab in patients with polyarticular juvenile idiopathic arthritis (PJIA) or systemic juvenile idiopathic arthritis (SJIA); neutrophils and platelets should be monitored at the second dose and thereafter every 4 to 8 weeks for PJIA and every 2 to 4 weeks for SJIA. Tocilizumab should not be started in patients with coronavirus disease 2019 (COVID-19) who have an ANC less than 1000 cells/mm3 or a platelet count less than 50,000 cells/mm3; neutrophils and platelets should be monitored in these patients.
References
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab (applies to tocilizumab) renal impairment
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction
Tocilizumab has not been studied in patients with severe renal dysfunction; caution is recommended when using tocilizumab in these patients. No dose adjustment is required in patients with mild or moderate renal dysfunction.
References
- "Product Information. Actemra (tocilizumab)." Genentech SUPPL-138/SUPPL-49 (2022):
Tocilizumab drug interactions
There are 335 drug interactions with tocilizumab.
Tocilizumab alcohol/food interactions
There is 1 alcohol/food interaction with tocilizumab.
More about tocilizumab
- tocilizumab consumer information
- Check interactions
- Compare alternatives
- Reviews (52)
- Side effects
- Dosage information
- During pregnancy
- Drug class: interleukin inhibitors
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.